In our study, we investigated the role of Parkinsonism-associated protein 7 (PARK-7), known as DJ-1, which is involved in several pathways that counteract oxidative stress. This stress is thought to contribute to the development of fibrosis and vascular damage in patients with systemic sclerosis (SSc). Our study aims to investigate the correlation between PARK-7 levels, laboratory and clinical findings related to SSc and treatment regimens.
Materials and methodsIn our study, we included fifty patients aged 18 years and older diagnosed with SSc and thirty healthy individuals without any systemic, malignant, or autoimmune diseases as a control group. We collected demographic data, clinical manifestations, laboratory and radiological findings, pulmonary function test (PFT), and echocardiography reports, information on comorbidities and prescribed medications from medical records, hospital database analysis, and direct patient interviews. Disease activity was quantified and documented using activity scoring systems developed by the European Scleroderma Study Group (EScSG) and the United Kingdom's (UK) Functional Activity Scoring. PARK-7 levels in venous blood samples from participating patients were quantified by Enzyme-Linked Immunosorbent Assay (ELISA).
ResultsThe PARK-7 level was 21.26±15.83 in the patient group and 16.11±11.83 in the control group. There was no significant difference in PARK-7 levels between the patient and control groups (p=.22). In terms of disease subtypes, PARK-7 levels were 21.35±18.36 in the limited form, 23.18±13.83 in the diffuse form. No statistically significant differences were observed between PARK-7 levels, the control group, and the different disease forms (p>.05). In patients classified as having active disease according to the EScSG scoring system, the PARK-7 level was 25.69±18.10 compared to 16.00±10.91 in the inactive group. No significant correlation was found between the presence of high-resolution computed tomography (HRCT) findings, other systemic involvement, and PARK-7 levels.
ConclusionsOver the past decade, numerous reports have highlighted the therapeutic potential of PARK-7 and its related molecules for the treatment of various diseases. Whether PARK-7 can be effectively used in the treatment of SSc remains unclear due to the cross-sectional design of our study. We believe that a study measuring PARK-7 levels in patients newly diagnosed or in the early stages of SSc, followed by randomised and prospective follow-up of clinical outcomes with and without treatment, could significantly improve our understanding of the role of PARK-7 in the pathogenesis of SSc and its potential applicability in the treatment of SSc patients.
En nuestro estudio, investigamos el papel de la proteína 7 asociada al Parkinson (PARK-7), la cual participa en varias vías que contrarrestan el estrés oxidativo. Se cree que este estrés contribuye al desarrollo de fibrosis y daño vascular en pacientes con esclerosis sistémica (ES). Nuestro estudio tiene como objetivo investigar la correlación entre los niveles de PARK-7, los hallazgos clínicos y de laboratorio relacionados con la ES y los regímenes de tratamiento.
Materiales y métodosEn nuestro estudio, incluimos cincuenta pacientes de 18 años o más diagnosticados con SSc y 30 individuos sanos sin ninguna enfermedad sistémica, maligna o autoinmune como grupo de control. Recopilamos datos demográficos, manifestaciones clínicas, hallazgos de laboratorio y radiológicos, pruebas de función pulmonar (PFT) e informes de ecocardiografía, información sobre comorbilidades y medicamentos prescritos de los registros médicos, análisis de bases de datos hospitalarias y entrevistas directas a los pacientes. La actividad de la enfermedad se cuantificó y documentó utilizando sistemas de puntuación de actividad desarrollados por el Grupo de Estudio Europeo sobre Esclerodermia (EScSG) y la Puntuación de Actividad Funcional del Reino Unido. Los niveles de PARK-7 en muestras de sangre venosa de los pacientes participantes se cuantificaron mediante un ELISA.
ResultadosEl nivel de PARK-7 fue de 21,26±15,83 en el grupo de pacientes y de 16,11±11,83 en el grupo de control. No hubo diferencias significativas en los niveles de PARK-7 entre los grupos de pacientes y control (p=0,22). En cuanto a los subtipos de enfermedad, los niveles de PARK-7 fueron 21,35±18,36 en la forma limitada y 23,18±13,83 en la forma difusa. No se observaron diferencias estadísticamente significativas entre los niveles de PARK-7, el grupo control y las diferentes formas de enfermedad (p>0,05). En los pacientes clasificados como con enfermedad activa según el sistema de puntuación EScSG, el nivel de PARK-7 fue de 25,69±18,10 en comparación con 16,00±10,91 en el grupo inactivo. No se encontró correlación significativa entre la presencia de hallazgos en la tomografía computarizada de alta resolución (TCAR), otra afectación sistémica y los niveles de PARK-7.
ConclusionesDurante la última década, numerosos informes han destacado el potencial terapéutico de PARK-7 y sus moléculas relacionadas para el tratamiento de diversas enfermedades. Aún no está claro si PARK-7 se puede utilizar eficazmente en el tratamiento de la SSc debido al diseño transversal de nuestro estudio. Creemos que un estudio que mida los niveles de PARK-7 en pacientes recién diagnosticados o en las primeras etapas de SSc, seguido de un seguimiento aleatorio y prospectivo de los resultados clínicos con y sin tratamiento, podría mejorar significativamente nuestra comprensión del papel de PARK-7 en la patogénesis de la SSc y su potencial aplicabilidad en el tratamiento de pacientes con SSc.
SSc is an autoimmune connective tissue disease characterised by a chronic and progressive course involving multiple systems. It is characterised by unexplained vasculopathy and fibrosis, which contribute to increased morbidity and mortality.1 Research has shown that the pathogenesis of SSc is influenced by a number of factors, including infections, environmental elements and genetic factors.2 Parkinson's-associated protein-7 (PARK-7), a multifunctional protein, acts as a molecular chaperone with protease properties. It plays a role in responding to oxidative stress, reactivating transcription and regulating mitochondrial function.3–6
PARK-7 is primarily located in the cytoplasm of cells, with a lesser presence in the nucleus and mitochondria. It has been identified in various tissues including brain, kidney, liver, pancreas and skeletal muscle. PARK-7 regulates antioxidant, anti-apoptotic and anti-inflammatory pathways. This is achieved by reducing the production of reactive oxygen species (ROS)7 and upregulating the expression of superoxide dismutase (SOD2) in the nucleus and simultaneously reducing the accumulation of ROS. This beneficial effect was observed during the progression of renal fibrosis.8 Studies in SSc have shown that measuring plasma SOD2 activity can be a valuable parameter in assessing the progression of fibrosis and the presence of Raynaud's phenomenon.9 Oxidative stress resulting from increased production of ROS by fibroblasts, endothelial cells and T-cells, which play a central role in the pathogenesis of SSc, is thought to be associated with significant aspects of the disease, including fibrosis and vascular damage.10 The expression of endothelial nitric oxide synthase (eNOS) was significantly increased in cells overexpressing PARK-7. This observation suggests that the protein may contribute to vasorelaxation and may act as an antioxidant.11 Reduced expression, impaired function and suppression of eNOS within the pulmonary endothelium contribute to increased vascular smooth muscle constriction and remodelling. This process ultimately leads to the initiation and progression of pulmonary arterial hypertension (PAH).12 Renal PARK-7 is thought to play a role in regulating oxidative stress during the progression of ROS-induced hypertension.13 In this study, we investigated the role of PARK-7 in counteracting oxidative stress through multiple pathways, which is thought to contribute to fibrosis and vascular damage in individuals with SSc. The observation that PARK-7 enhances eNOS expression suggests its potential as a therapeutic target for PAH, a condition that significantly increases morbidity and mortality in SSc patients. The aim of our study was to investigate the correlation between PARK-7 levels and both laboratory and clinical aspects of SSc patients.
Patients and methodsThe study protocol was submitted to our Clinical Research Ethics Committee and approval was granted under decision number 2022.95.05.22 during the meeting on 31.05.2022. Our study included 50 patients over 18 years of age who had been diagnosed with SSc according to the European League Against Rheumatism and American College of Rheumatology classification criteria.14 These patients were followed in the rheumatology outpatient clinic between 01/06/2022 and 01/12/2022. In addition, 30 healthy individuals with no systemic diseases, malignancies or autoimmune diseases were included in the control group. Patients’ demographic characteristics, clinical observations, laboratory and radiological findings, PFT and echocardiography results, concomitant diseases and prescribed medications were collected from medical records, hospital automation system records and direct patient interviews. The presence and extent of skin fibrosis was assessed using the modified Rodnan skin score (mRSS). Interstitial lung disease was identified on the basis of HRCT scan findings. SSc activity was quantified and recorded using EScSG activity scoring systems15 (active disease defined as ≥3) and the UK Functional Activity Scoring was used for calculation. Functional status was assessed using the EScSG index and mRSS.
Venous blood samples were taken from participating patients after an average fasting period of 10–12h. These samples were collected in standard biochemistry tubes. The collected blood samples were then centrifuged at 3000rpm for ten minutes using a centrifuge machine. After routine biochemical analyses, the remaining serum samples were separated. The serum samples obtained were stored at −80°C in a refrigerator until the following analyses were performed. Before analysis, the serum samples were thawed at room temperature and then homogenised by vortexing. PARK-7 levels were measured using BT brand Human Protein DJ-1, PARK7 ELISA kit and ELISA method, all according to the manufacturer's instructions.
After measuring PARK-7 levels in our subjects, we explored the correlation between PARK-7 levels and the presence of high-frequency antibodies, systemic involvement patterns, and disease activity based on EScSG scoring.
Statistical analysisThe statistical analysis of the data collected in our study was carried out using SPSS 24 software, and the assessment was made within a 95% confidence interval. T-tests and ANOVA tests were used to compare groups. Descriptive statistics included standard deviation, mean and percentages. Categorical variables within groups were examined using the Chi-squared test. In situations where the expected value in cells was less than 5, the Pearson Chi-squared test and Fisher's exact test were used to ensure that appropriate statistical methods were used.
ResultsThe study included 50 patients in the SSc group and 30 healthy volunteers in the control group. Of the patients, 45 (90%) were female and five (10%) were male. In the control group, 27 (90%) were female and three (10%) were male. The mean age of the SSc group was 54.38±11.25 years and of the control group was 54.30±10.67 years. There was no statistically significant difference in the age distribution between groups. Among participants, 12 were active smokers, two were ex-smokers, and 36 had no history of smoking. When patients were categorised according to the type of SSc, 27 (54%) were identified as having the limited form, 20 (40%) had the diffuse form.
Within the patient group, two individuals had a family history of SSc and seven had a history of other rheumatic diseases. Regarding comorbidities, hypertension was found in 16 patients, diabetes mellitus in nine, chronic renal failure in ten, hypothyroidism in nine, hyperlipidemia in four, coronary artery disease in three, chronic obstructive pulmonary disease in one, and primary biliary cholangitis in one.
Of the patients, 11 (22%) were using angiotensin converting enzyme (ACE) inhibitors or angiotensin receptor blockers, 14 (28%) were using methotrexate (MTX), eleven (22%) were using mycophenolate mofetil (MMF), seven (14%) were using bosentan, five (10%) were using azathioprine, 21 (42%) were prescribed colchicine, 14 (28%) were using pentoxifylline, six (12%) were using phosphodiesterase inhibitors, 13 (26%) used corticosteroids, seven (14%) used iloprost, 37 (74%) used calcium channel blockers,39 (78%) used hydroxychloroquine, 39 (78%) used acetylsalicylic acid, 30 (60%) used proton pump inhibitors (PPIs), and two (4%) used nintedanib. No patients received rituximab or cyclophosphamide during the trial.
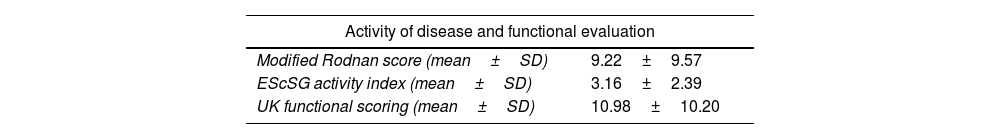
It was observed that 48 patients tested positive for anti-nuclear antibody (ANA), 19 for anti-topoisomerase-1 (anti-TP-1), 36 for anti centromere antibodies (ACA), ten for anti-RO, three for anti-LA and two for anti-RNP. Two patients with the diffuse pattern were both ACA and anti-TP-1 positive. One patient had both ACA and RNP positivity. Coexistence of anti-TP-1 and RNP positivity was not observed. Activity of disease, laboratory findings of the patients and antibody positivity are gathered. PFTs, HRCT and echocardiographic findings were obtained (Table 1).
Activity of disease, laboratory findings, pulmonary function tests (PFTs), high resolution computed tomography (HRCT) and echocardiographic findings of our patients.
| Activity of disease and functional evaluation | |
|---|---|
| Modified Rodnan score (mean±SD) | 9.22±9.57 |
| EScSG activity index (mean±SD) | 3.16±2.39 |
| UK functional scoring (mean±SD) | 10.98±10.20 |
| Laboratory findings | (mean±SD) |
|---|---|
| Sedimentation (mm/h) | 25.48±19.52 |
| CRP (mg/dl) | 4.52±12.09 |
| AST (U/L) | 17.16±8.03 |
| ALT (U/L) | 22.56±7.34 |
| Cre (mg/dl) | 0.74±0.22 |
| Hb (g/dl) | 12.22±1.34 |
| Hct (%) | 37.52±3.62 |
| WBC (1000/μL) | 6.19±1.83 |
| PLT (1000/μL) | 236.56±86.04 |
| Pro BNP (pg/dl) | 171.76±232.94 |
| Antibody | n (%) |
|---|---|
| Anti nuclear antibody | |
| ANA (1+) | 1 (2) |
| ANA (2+) | 6 (12) |
| ANA (3+) | 10 (20) |
| ANA (4+) | 31 (62) |
| Anti topoisomerase | 19 (38) |
| Anti Ro | 10 (20) |
| Anti La | 3 (6) |
| Anti centromer | 36 (72) |
| RNP | 2 (4) |
| PFT, HRCT, echocardiographic findings | Systemic sclerosis |
|---|---|
| FVC mean±SD (normal: >80) | 89.24±21.93 |
| DLCO mean±SD (normal: 60–120) | 70.34±25.37 |
| EF mean±SD | 58.44±8.80 |
| PAP increase n (%) | 21 (42) |
| HRCT findings n (%) | 20 (40) |
Abbreviations: EScSG: European Scleroderma Study Group, UK: United Kingdom, SD: standard deviation, CRP: C-reactive protein, AST: aspartate aminotransferase, ALT: alanine transaminase, cre: creatinine, Hb: haemoglobin, Hct: hematocrit, WBC: white blood cell count, PLT: platelet count, pro BNP: pro brain natriuretic peptide, ANA: anti nuclear antibody, anti-RNP: anti-ribonucleoprotein, FVC: forced vital capacity, EF: ejection fraction, PAP: pulmonary arterial pressure, DLCO: diffusing capacity of the lungs for carbon monoxide, anti-Ro and anti-La: anti-Sjögren's-syndrome-related antigen A autoantibodies.
Gastrointestinal involvement was identified in 30 patients, interstitial lung disease (ILD) in 20, cardiac involvement in 12, and renal involvement in 10.When PARK-7 levels were compared between the patient and control groups, PARK-7 levels were 21.26±15.83 in the patient group and 16.11±11.83 in the control group. No significant difference in PARK-7 levels was observed between the patient and control groups (p=0.220). PARK-7 levels were 21.35±18.36 in the limited form and 23.18±13.83 in the diffuse form.
When examining the relationship between the presence of high frequency positive antibodies in SSc and PARK-7 levels, no significant correlations were found (ANA p=0.211, anti TP-1 p=0.780, ACA p=0.171). The PARK-7 level was 25.69±18.10 in the group with active disease according to EScSG scoring compared to 16.00±10.91 in the inactive group, which showed a significant difference (p=0.019). No significant correlations were found between HRCT findings, other systemic involvement and PARK-7 levels.
DiscussionDespite the absence of statistical significance among the groups in our study, the pivotal nature of this research lies in its role as the inaugural exploration of PARK-7 in SSc patients, marking the starting point for further discussion and investigation into this crucial area. In the existing literature, there are no studies that investigate serum PARK-7 levels in patients with SSc.
Some scientific research has shown that PARK-7 plays a pivotal role in suppressing the production of pro-inflammatory cytokines.16 Because of PARK-7's cytoprotective properties, current research is focusing on therapeutic approaches to enhance its cellular effects. One such strategy involves the use of phenylbutyrate to target PARK-7. This avenue of investigation holds great promise for enhancing the beneficial effects of PARK-7 and potentially leading to new treatment options for various diseases.17 Over the past decade, numerous studies and reports have highlighted the therapeutic potential of PARK-7 and molecules targeting it to treat neurodegenerative diseases.18
Our evaluation of the correlation between antibodies commonly found in SSc and PARK-7 did not yield significant results and no significant correlation was found between laboratory values such as ESR and CRP and serum PARK-7 levels, During our interpretation, we considered the possibility that the acute phase values might have been influenced by infections occurring concurrently with the patients throughout the course of the disease, adding a layer of complexity to our analysis. Furthermore, the potential overlap of connective tissue diseases in the course of scleroderma may have also impacted the association between antibodies and PARK-7. Considering these confounding factors, further research is needed to clarify the exact relationship between PARK-7 and its potential role in the treatment of SSc.
In accordance with the EScSG scoring system, we observed that the PARK-7 level was higher in the active disease group (25.69±18.10) than in the inactive group (16.00±10.91), and this difference was statistically significant (p=0.019). However, our analysis did not reveal any significant correlations between HRCT findings, the presence of gastrointestinal, pulmonary, cardiac and renal involvement and PARK-7 levels. It's important to recognise that SSc is a complex disease affecting multiple systems, which can lead to limitations in research. The intricate interplay of different factors in SSc makes it difficult to identify direct associations in specific cases.
The expression of PARK-7 appears to be differentially altered depending on the specific disease conditions and/or cell types involved. For example, PARK-7 is upregulated in acute lung injury induced by lipopolysaccharides, but downregulated in lung disease caused by heavy smoking.19,20 In our study, the mean PARK-7 level was 18.31±12.03 in smokers and 22.16±16.91 in the non-smokers. Although PARK-7 may play a role in the pathogenesis of SSc, its relationship with clinical and laboratory findings and disease activity remains inconclusive. Further research, incorporating a broader range of variables and a larger sample size while considering selection bias, could be conducted to gain deeper insights into this issue.
We believe that a study involving the measurement of PARK-7 levels in early or newly diagnosed patients, followed by randomised and prospective follow-up of their clinical outcomes both with and without treatment, could significantly contribute to a comprehensive understanding of the role of PARK-7 in the pathogenesis and its potential applicability in treatment. Given the relatively low incidence of the disease, it would be more appropriate for such a study to be multicentre.
ConclusionSignificantly contributing to the scientific landscape, the strength of our study lies in that it stands out as the first of its kind to investigate the correlation between the PARK-7 molecule, previously studied in neurodegenerative and inflammatory diseases, and the manifestations observed in SSc, along with the disease's progression. This pioneering effort not only sheds light on a novel perspective but also establishes a foundation for further exploration into the intricate connections between PARK-7 and the complexities of SSc. Due to the inherent limitations of its cross-sectional nature, prospective investigations are essential to further elucidate the role of PARK-7 in disease activity. The presence of confounding factors, coupled with the small sample size, underscores the need for a more comprehensive understanding. Exploring its potential as a targeted therapeutic option necessitates a longitudinal approach to unravel the complexities inherent in SSc.
Ethical considerationManuscript has no ethical implications in its methodology or results that the reader should consider. Written consent has been obtained from the patient.
Conflict of interestsNone.