Polymyalgia Rheumatica is one of the most frequent inflammatory musculoskeletal disorders in adults over 50 years of age that can present with polyarthritis. The case is presented of a 65-year-old woman with chronic disabling severe polyarticular pain associated with polyarthritis. It was initially diagnosed as seronegative rheumatoid arthritis, in which bilateral sub-deltoid and trochanteric bursitis was demonstrated by ultrasound, along with bicipital tenosynovitis, all features of polymyalgia rheumatica. A good clinical and ultrasound response to corticosteroid treatment is also described.
La polimialgia reumática es una de las patologías inflamatorias musculoesqueléticas más frecuentes en adultos mayores de 50 años que pueden presentarse con poliartritis. Se presenta el caso de una mujer de 65 años con cuadro crónico de dolor poliarticular severo incapacitante, asociado a poliartritis, diagnosticada inicialmente como artritis reumatoide seronegativa, en quien se demostró, mediante ultrasonido, bursitis subdeltoidea y trocantérica bilaterales, así como tenosinovitis bicipital, todas características de polimialgia reumática. Se describe también una buena respuesta clínica y ultrasonográfica al tratamiento con corticoides.
Polymyalgia rheumatica (PMR) is an inflammatory rheumatic disease common in older adults, characterized by proximal pain in the shoulders, the neck and the pelvic girdle associated with prolonged morning stiffness, which does not have a specific laboratory test or inflammatory marker to make the diagnosis.1 Its incidence varies between the United States and the European countries, ranging from 12.7 to 112.6 cases per 100,000 inhabitants in adults over 50 years of age, with the highest incidence in Norway2 and in people over 70 years of age.3,4
Almost 50% of the patients diagnosed with this disease may have distal manifestations such as peripheral arthritis and swollen hands, which can lead us to confuse the diagnosis with late-onset rheumatoid arthritis (RA).5 Nevertheless, it has been established that both are separate entities, despite the fact that they share phenotypic similarity at the beginning.6
For this reason, new criteria to diagnose PMR in a more specific way were established in 2012, including, in addition to the mentioned classic clinical and laboratory criteria, some abnormal ultrasound (US) findings on the shoulders and hips.1
On the other hand, the US Point of Care (POC US) is defined as a US study conducted by the physician in charge of the patient, usually as an adjunct to the physical examination, to identify the presence or absence of a limited number of specific findings.7 Thus, it can be used in an elderly patient with a clinical picture of polyarticular inflammation without a precise diagnosis, looking for the presence of bursitis in the shoulders and trochanters to identify a case of PMR.
The indexed bibliography does not report PMR cases in Peru. Consequently, our objective is to report a case of polymyalgia rheumatica associated with seronegative polyarthritis that was diagnosed using the POC US, in order to identify some of the current criteria for the diagnosis of this disease.
Case presentationA 65-year-old woman admitted due to a clinical picture that had started 6 months before with pain in the temporomandibular joint and the jaw, bilateral, with an intensity of 7/10, that impeded mastication, associated with pain of the same intensity, in addition to bilateral stiffness in the occipital region, posterior neck, trapezius muscles and shoulders, which prevented her from moving and lifting the shoulders and turning the neck. In addition, she presented pain in the right hip (gluteal and trochanteric region) that increased when she was sitting for more than 20 min and prevented her from walking. These pains were persistent, with no variation between day and night.
Five months before her admission, she had an increase in volume in the metacarpophalangeal joints of both hands, related to pain of intensity 7/10, without associated erythema.
Four months before her admission, these symptoms increased to an intensity of 8/10, with an increase in local temperature and edema of all the fingers of both hands and wrists associated with a non-quantified sensation of thermal rise for 15 days, which resolved spontaneously. This was associated with stiffness of all the involved joints.
Two months prior to her admission, bilateral pain in the neck, shoulder girdle, hands and wrists persisted, and erythematous spots were added in the dorsal aspect of all the proximal interphalangeal (PIP) and metacarpophalangeal (MCP) joints of both hands. In addition, she had stiffness in all these joints throughout the whole day, predominantly in the morning, which lasted for several hours and improved moderately as the day passed due to movement, but did not disappear completely. This stiffness was more intense in the hands, to the point that she could not clench her fist or grasp things. She also experienced Raynaud's phenomenon in the hands and was unable to stand up without help due to additional similar involvement of both knees. It was not possible for her to close her hands to hold things.
The patient received 10 mg of prednisone during a month, without improvement in her condition, because her treating doctor thought at this time that it was an “activity of a rheumatoid arthritis”. Throughout the course of the disease, the polyarticular pain ranged between 7/10 and 10/10, predominantly in the morning.
One month before admission, bilateral pain and increase in volume of the ankles and toes were added. At this time, the intensity of the polyarticular pain was 10/10.
Ten days before admission, due to the pain and stiffness described, she could no longer get out of bed, it was not possible to separate her arms from her body and she depended on others to wash, eat, bathe, go to the bathroom or write. During the entire time of the disease, she presented hyporexia and lost 12 kg in total.
She had no previous headache, visual disturbances, jaw claudication, pain or swelling in temporal regions, cutaneous lesions on the face, malar rash, photosensitivity, foamy urine, or cardiorespiratory symptoms at the time of admission.
She has the antecedent of having suffered from inflammatory joint disease of the shoulders, back and hands 35 years ago, which at this time was diagnosed as “seronegative rheumatoid arthritis” and treated with prednisone 10 mg/day, conditional to the symptoms (last episode 3 years ago). Likewise, she had had osteoarthrosis of the hands 10 years ago; arterial hypertension 5 years ago, treated with losartan; fibromyalgia and depression 5 years before, treated with pregabalin, NSAIDs, sertraline and alprazolam; dry eye syndrome 5 years before, treated with artificial tears; and «fatty liver» 3 years ago. There was no history of previous diabetes mellitus, thyroid disease, cerebrovascular or neuromuscular disease.
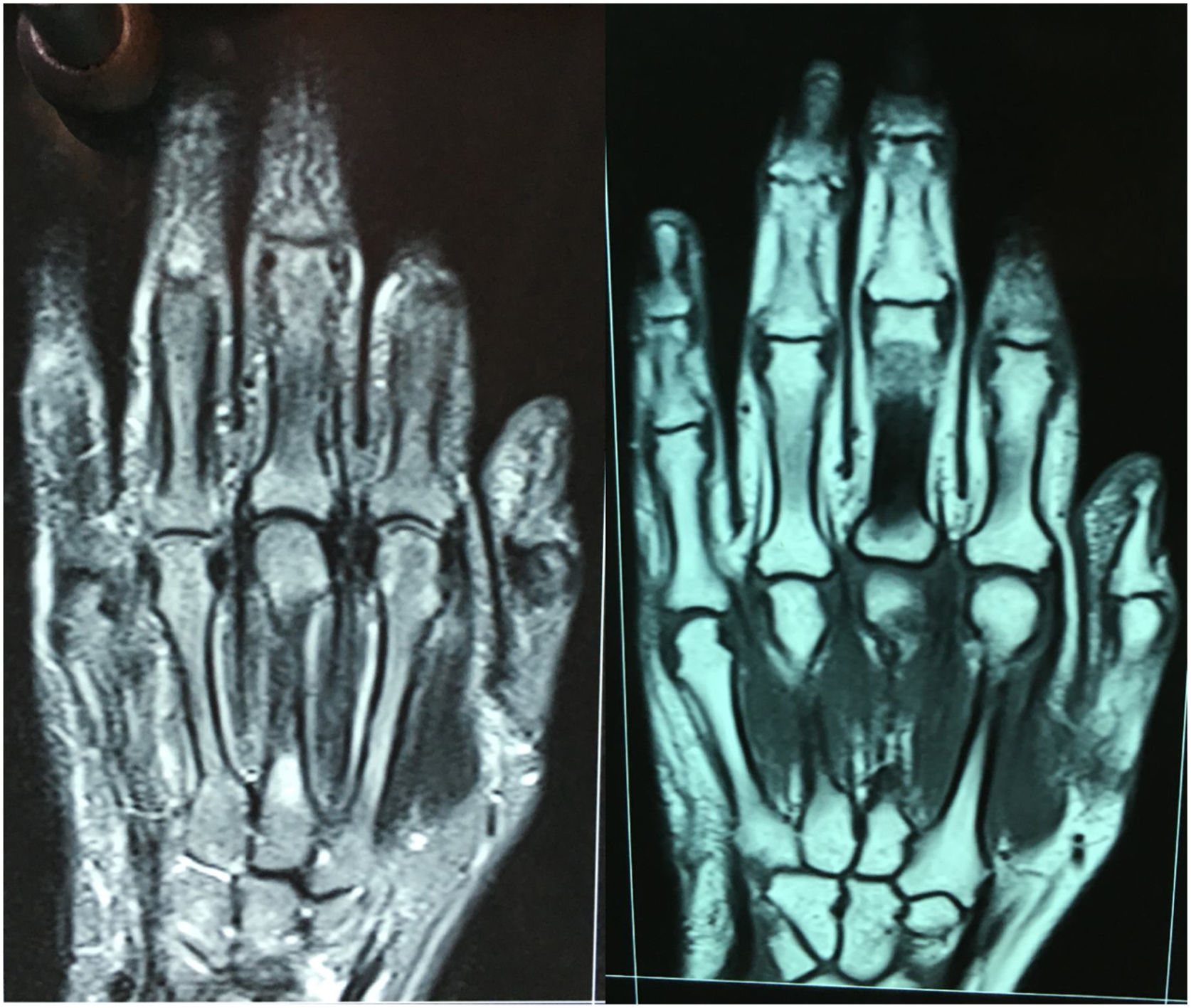
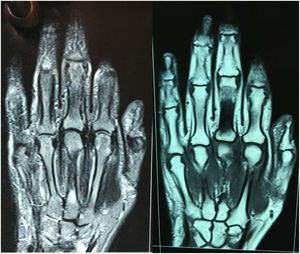
In the physical examination on admission she had a blood pressure of 130/60 mmHg, a hearth rate of 72 beats per minute, respiratory rate (RR) of 24 breaths per minute, temperature of 37.6 °C and oxygen saturation of 95% with ambient oxygen. She had mild conjunctival pallor, but without scleral icterus. The temporal arteries were not painful and they did not appear increased in caliber or consistency. Erythematous spots were found in the skin of the dorsal area of the PIP and MCP joints of both hands (Fig. 1). She did not have malar rash or lesions in the face and the trunk.
In the articular examination, she had increased volume of all the joints of the hands, both wrists, shoulders, elbows, knees, ankles and joints of both feet, with a bilateral positive squeeze test in the hands and feet. She had mild synovitis in the PIP and MCP joints in both hands (Fig. 1, left).
The examination was painful on muscle palpation of both deltoids, while the active abduction of the shoulders was minimal due to severe pain. In addition, she presented increased volume and pain on palpation and digitopressure of the subtrochanteric area in both thighs. The muscle mass was greatly decreased in the thighs, shoulders, arms and forearms, but the muscle tone was normal.
The abdominal, neurological, pulmonary and cardiac examination was normal.
In the laboratory tests she presented erythrocyte sedimentation rate (ESR) of 65 mm/h and C reactive protein of 9.7 mg/dl (NV: 0–0.5). The immunological markers showed negative anti-extractable nuclear antigen (ENA profile), anti-cyclic citrullinated peptide (anti-CCP), antinuclear (ANA) antibodies and rheumatoid factor. In the laboratory tests she had Hb in 10 g/dL, with normal corpuscular constants, in addition to normal counts of leukocytes and platelets. In the biochemical tests, the glucose, creatinine, DHL, TGO, total CPK, serum calcium, albumin and globulin were within normal ranges.
The electromyography only showed signs of bilateral carpal tunnel syndrome without myopathic involvement. A magnetic resonance imaging (MRI) of the hands was also performed, in which adequate regular and symmetric metacarpophalangeal and proximal interphalangeal joint spaces were evidenced, without synovial thickening or joint erosions in proximal interphalangeal, metacarpophalangeal, carpometacarpal and midcarpal joints, although a slight increase in volume of periarticular structures was observed, especially in the second and third metacarpophalangeal joints (Fig. 2).
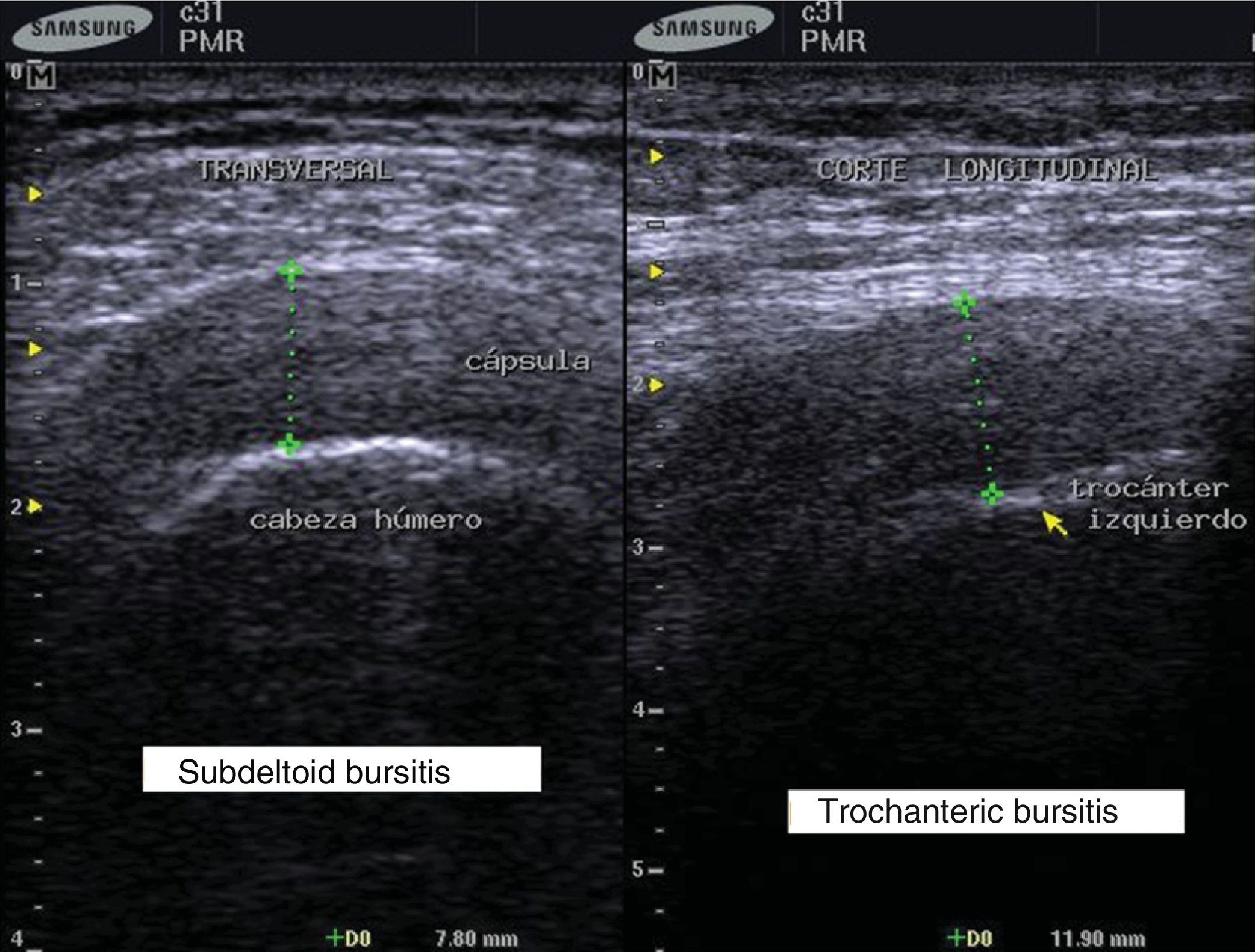
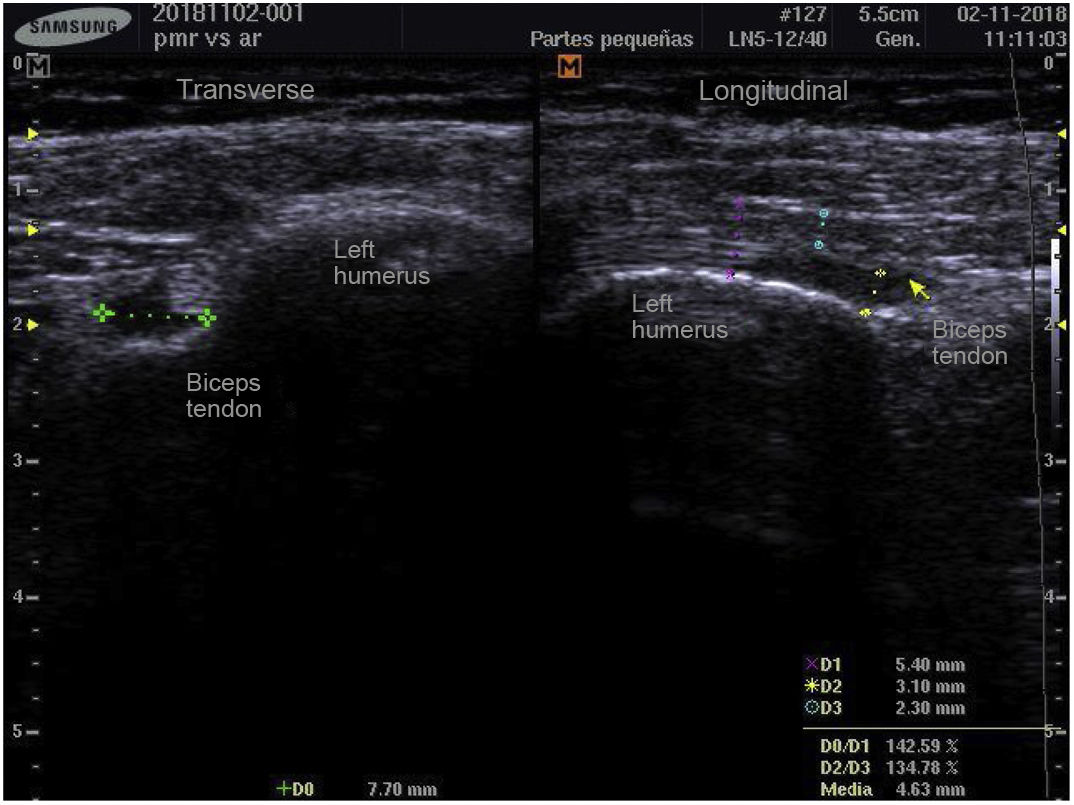
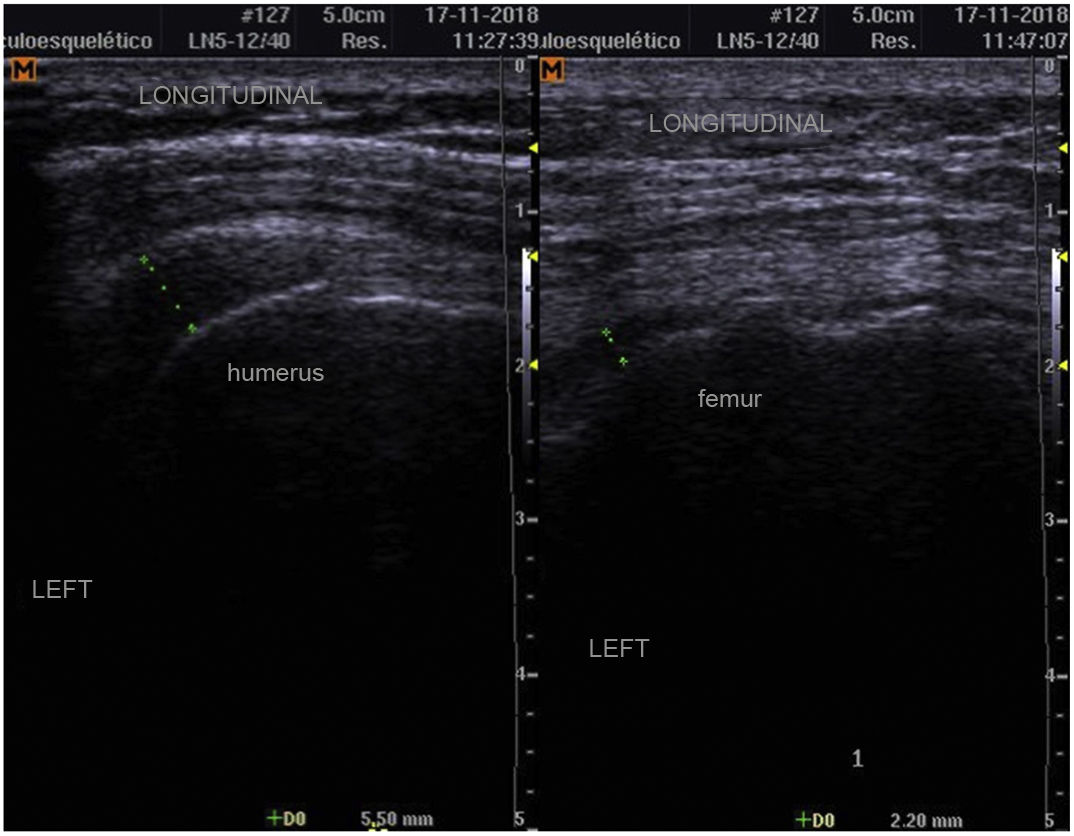
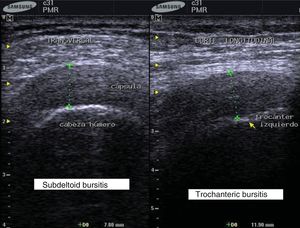
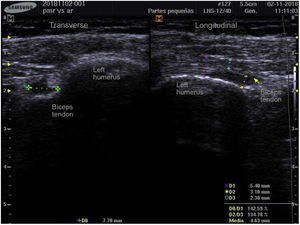
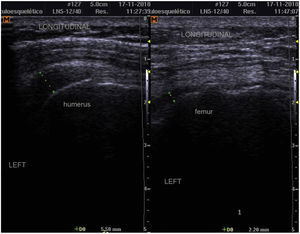
POC US studies of the shoulders, wrists and hands were performed with a Samsung® SonoAceR3 ultrasound equipment, with a high frequency linear transducer to establish the diagnosis, and subdeltoid bursitis was evidenced in both shoulders (greater in the left than in the right) (Fig. 3, left), as well as tenosynovitis in the left biceps tendon (Fig. 4) and bilateral trochanteric bursitis with synovitis of the hip (Fig. 3, right).
With these findings, the diagnosis of PMR was confirmed and treatment was started with 20 mg of oral prednisone, but there was no improvement on the first day, so the dose of this drug was increased to 30 mg. As a result, the pain intensity decreased at 24 h from 8/10 to 5/10. Likewise, the periarticular inflammation in the hands, wrists and ankles decreased, and the patient was able to sit up by herself at the second day of treatment with 30 mg of prednisone.
The patient was discharged on the fifth day of use of prednisone 30 mg per day, walking on her own, eating by herself and very satisfied with having improving substantially and with the global pain intensity in 4–5/10.
Treatment with 20 mg of methotrexate weekly associated with oral folic acid daily was also started, according with the 2015 EULAR/ACR guidelines,8 because the patient had previously been a user of corticosteroids and she had several relapses in the last year, especially the last episode which was disabling, and also because she had a high risk of adverse effects from the corticosteroids.
The patient was reevaluated after 2 weeks of treatment with methotrexate weekly and prednisone 30 mg/day, and she was already walking alone, raised her arms above her shoulders and could flex her fingers better (Fig. 1, right). In addition, she reported a pain intensity of 3–4/10 (and some days she reported no pain), but that allowed her to fend for herself.
An ultrasound control was performed, in which a considerable decrease in the subdeltoid (from 7.8 mm to 5.5 mm) and trochanteric bursitis (from 11.9 mm to 2.2 mm) was evidenced (Figs. 4 and 5).
DiscussionThe reported case describes an older adult patient with multiple pathological antecedents who presented with a chronic clinical picture of osteomyoarticular pain. This picture had started in the shoulder girdle, the neck, and the hips, and then it became generalized to the hands, knees, and ankles, without improvement with low doses of prednisone, NSAIDs, and pregabalin. Since in this case there were previous episodes of osteoarticular pain for more than 30 years, the patient was previously diagnosed as seronegative RA and she partially improved with low doses of corticosteroids until this last episode.
Even though a clinical picture of PMR in older adults can be confused not only with RA, but also with other rheumatologic pathologies (arthritis due to crystals, vasculitis, among others),9 the patient had negative RF, anti-CCP, ANA and ANCA.
Despite the fact that PMR is frequently associated with giant cell arteritis,10,11 this patient did not have clinical symptoms of giant cell arteritis. Thus, since she presented non-specific rheumatological symptoms, including arthritis and synovitis, she was cataloged as seronegative RA (although the arthritis was non-erosive) and received low doses of corticosteroids without finding improvement in the clinical picture. This led her to a functional disability, to the point of making her completely dependent to perform some activity.
In Latin America, cases of PMR have been reported only in Colombia, and patients very frequently report pain or stiffness in the shoulder girdle (99%) and in the pelvic girdle (90%), with predominance in the female gender (80%), cervical pain (49%), fatigue (36%), weight loss (21%), arthritis (21%) and fever (16%).12 The reported patient presented all these characteristics.
Due to the multiple clinical criteria for the diagnosis of PMR, in 2012 the EULAR/ACR agreed to include criteria of ultrasonography images in order be able to establish a diagnosis of this disease with a sensitivity and specificity of more than 90%. These criteria are unilateral or bilateral subdeltoid bursitis, bicipital tenosynovitis or trochanteric bursitis, either unilateral or bilateral.1,10
Moreover, US is being increasingly used as an extension of the physical examination for the initial evaluation of many musculoskeletal inflammatory diseases, since it is portable, non-invasive, does not involve radiation, and it is inexpensive.11 Then, when we performed the POC US studies in the patient looking for these abnormalities, we found bilateral involvement of the three anatomical structures described, and according to the 2012 criteria,1 the patient had a score of more than five points with US.
With this, we classified the patient as PMR and agreed with her to start therapy with prednisone at a dose higher than the recommended of 15 mg, since she was already receiving this drug at doses between 10 and 20 mg for about 6 months (due to a misdiagnosis of seronegative RA) and she did not improve. In this way the patient fulfilled a criterion of definition of a patient resistant to glucocorticoids.13 With the increase to 30 mg of prednisone, the expected clinical response was obtained in 48 h, as described above.
Findings of certain characteristics of patients with PMR resistant to glucocorticoids, such as female gender, C-reactive protein value higher than 8 mg/dl, ESR higher than 80 mm/h, greater pain intensity at admission by visual analogue scale (between 7 and 10), morning stiffness for more than 2 h and presence of peripheral arthritis are described.13 Our patient had all these characteristics, except the ESR value. For this reason, therapy with methotrexate was added.
On the other hand, a comparative MRI of the hands was performed to the patient before she was admitted to hospitalization, without observing articular changes suggestive of RA, such as bone edema, synovitis or bone erosions, which are reported in between 80 and 100% of the cases of rheumatoid arthritis, even in early RA of less than 3 months of evolution.14
Although there are studies that suggest some findings in the MRI of the hands that are more frequent in patients with PMR than in healthy controls, such as tenosynovitis of the common extensor of the fingers without significant synovitis,15 the tendon of this muscle could not be visualized in the incidence of the MRI image of the reported patient.
After discharge, we reevaluated the patient 14 days after the initiation of the therapy with prednisone and methotrexate, and when we conducted another POC US study we evidenced a decrease in the echographic extension of the bursitis, both subdeltoid and trochanteric. This was consistent with the improvement in the pain and in the general clinical picture with the immunosuppressive treatment.
This is in agreement with previous studies that also suggest that US can be used as a useful tool for monitoring the response to treatment in PMR, either with corticosteroids, or with anti-TNF.12 Even, a decrease in shoulder bursitis is reported, from in 61% of the patients before treatment, to 36% after 12 weeks of treatment with tocilizumab.16
For this reason, we consider that the MRI, despite detecting findings characteristic of PMR; has higher costs and technical difficulties compared with a POC US study at the bedside of the patient, which can find the same results that are observed in the MRI: trochanteric and subdeltoid bursitis and bicipital synovitis, as established by the current classification criteria for PMR.1 In addition, an US equipment can be available immediately and, when it is used by trained personnel, it can report these findings more quickly than a MRI, at the same moment of the clinical evaluation of the patient, either in hospitalization, or even in some doctor’s offices.
We can conclude, then, that PMR can present in an older adult patient associated with non-erosive symmetric polyarthritis, without presenting giant cell arteritis with elevated inflammatory markers, and that it can be differentiated from RA by having negative RF and anti-CCP, and findings in the US POC of bicipital tendinitis and shoulder and trochanteric bursitis.
In the case of women over 50 years of age with chronic polyarticular pain of inflammatory type, that makes us suspect late onset RA, but who have negative markers for this pathology, we should investigate whether a possible PMR is present. For this reason we recommend to carry out POC US studies in patients over 50 years of age with chronic osteomyoarticular pain, to be able to differentiate between the true synovial and articular involvement and the bursae and tendon involvement, especially when the greatest pain commitment is in the pelvic and shoulder girdle. Even, the POC US can be used for monitoring the response to pharmacological management, which goes hand in hand with the clinical response.
Conflict of interestThe author declares that he has no conflict of interest.
Please cite this article as: Guillén López OB. Ultrasonografía point of care para el diagnóstico de polimialgia reumática en poliartritis crónica seronegativa: un reporte de caso. Rev Colomb Reumatol. 2022;29:68–73.