Systemic lupus erythematosus (SLE) is a heterogeneous autoimmune disease with a wide range of clinical manifestations that may affect any organ. Polyarteritis nodosa (PAN) is defined as necrotizing inflammatory changes in the medium and small vessels, a rare form of systemic necrotizing vasculitis in childhood. This article discusses the case of a patient with a history of deep venous thrombosis of the left leg, who presented with erythematosus purple lesions in her right hand, associated with pain, intermittent claudication, progressive limping and generalized edema. While in hospital, she was diagnosed with SLE with renal involvement and medium vessel vasculitis mainly of the upper limbs. She also met the criteria for PAN, a rare association that is seldom described in the medical literature.
El lupus eritematoso sistémico (LES) es una enfermedad autoinmune heterogénea con una amplia variedad de manifestaciones clínicas que pueden afectar cualquier órgano. La panarteritis nodosa (PAN) se define como cambios inflamatorios necrotizantes en arterias medianas o pequeñas, siendo una vasculitis necrotizante sistémica rara en la infancia. Presentamos el caso de una paciente con antecedente de trombosis venosa profunda de miembro inferior izquierdo, que presenta lesiones violáceas eritematosas en mano derecha, asociadas a dolor, claudicación intermitente, limitación funcional progresiva, así como edema generalizado. Durante la hospitalización se llega al diagnóstico de LES con compromiso renal y vasculitis de vasos medianos con predominio de miembros superiores que cumple criterios de PAN, asociación rara muy poco descrita en la bibliografía.
Systemic Lupus Erythematous (SLE) is a heterogeneous, autoimmune disease with a broad range of clinical and serological manifestations that may affect any organ; lupus nephritis, neuropsychiatric disorders, and cytopenia, are the most frequent manifestations.1 The prevalence of vasculitis in SLE ranges between 11 and 36%,2,3 affecting mostly the small vessels and to a lesser extent, the medium vessels; the latter increases the morbidity and mortality and is associated with more significant visceral involvement.4 Polyarteritis nodosa (PAN) is a rare vasculitis in childhood,5 and PAN criteria, according to the European League Against Rheumatism (EULAR)/Pediatric Rheumatology International Clinical Trials Organization (PRINTO)/and the Pediatric Rheumatology European Society (PRES) are: mandatory finding of anomalies in a small to medium sized artery identified by means of a biopsy as necrotizing vasculitis, or angiographically, identifying aneurisms, stenosis or occlusions not associated with fibromuscular dysplasia; and, at least, one of the following 5 systemic characteristics: skin involvement (livedo reticularis, subcutaneous nodules, skin infarctions), myalgia or muscle sensitivity, hypertension, peripheral neuropathy, renal involvement.6 This article discusses the case of a 15-year old female patient with SLE, who developed medium vessel vasculitis, predominantly in the upper extremities, and meets the criteria for PAN.
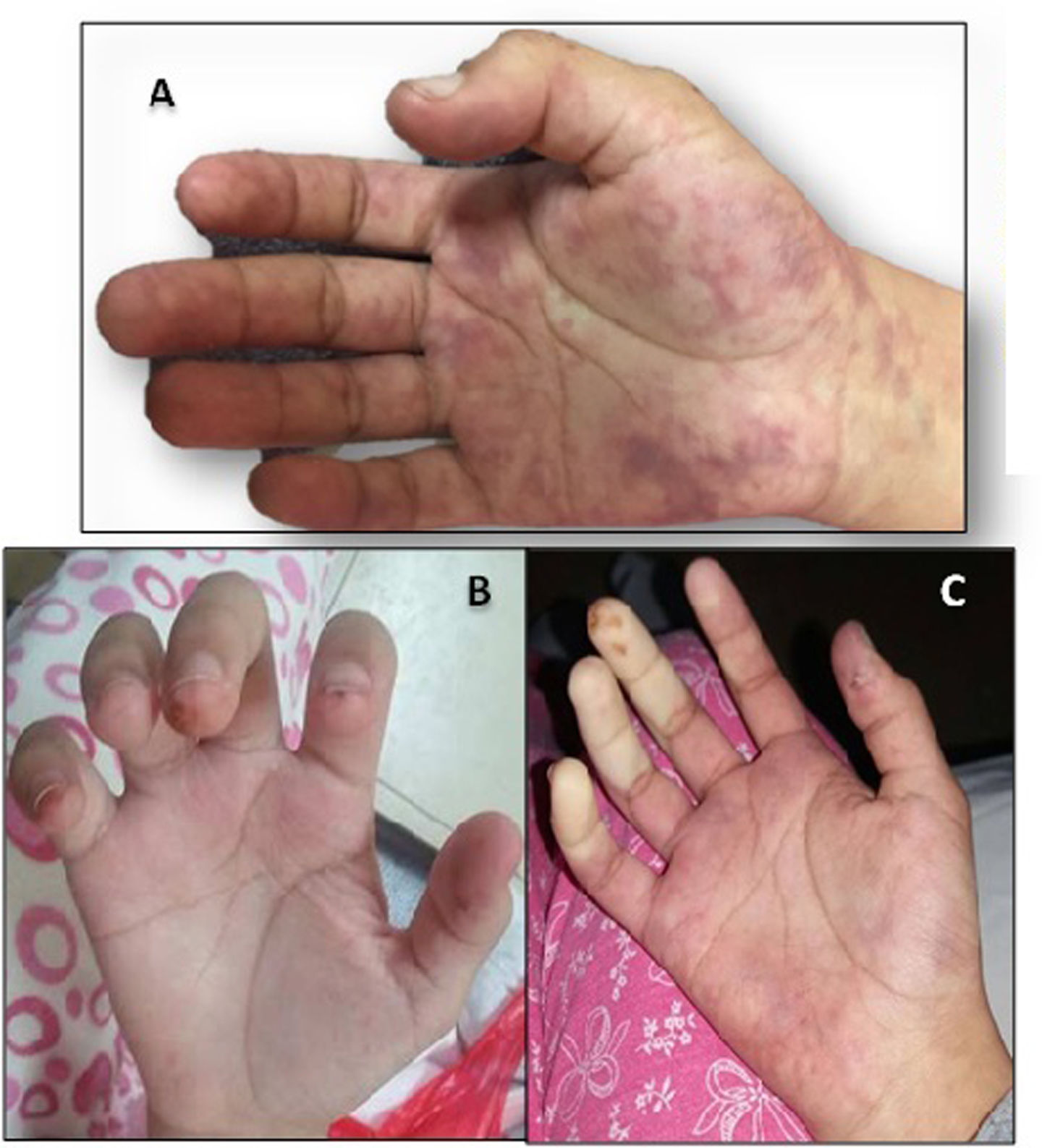
Case reportA 15-year old female patient from Lima, Perú, with unremarkable history, and 7 months of evolution of the disease characterized by pain and increased volume of the left leg. The patient was seen at the hospital and was diagnosed with deep venous thrombosis of the left lower limb and received 2 doses of subcutaneous enoxaparin. Two months prior to her admission she experienced right hand pain associated with erythema and purple lesions under the nails. Three weeks before, the patient also experienced decreased temperature, pallor, purple erythematous lesions in the right hand associated with pain, intermittent claudication, and a feeling of “pressure” in the right upper limb. One week earlier, she also presented with intense cyanosis of the right hand and progressive functional limitation, in addition to edema of the lower limbs, the face and eyelids. The physical examination at admission showed eyelid and lower limbs edema resulting in fovea, purple lesions on the palm of the hand and trophic fingertip changes in the digits of the right hand, distal coldness, decreased radial and ulnar pulses of the right arm (Fig. 1, increased volume and pain in the proximal and distal interphalangeal joints. During hospitalization the patient presented high blood pressure, which required the use of antihypertensives. The diagnosis of SLE was based on clinical and immunological criteria: arthritis, renal involvement; and ANA + speckled pattern 1/320, native anti-DNA + 1/40, +lupus anticoagulant. The diagnosis of renal involvement was based on massive proteinuria 24 h proteinuria = 5814 mg; however, no renal biopsy was performed. The patient received 3 pulses of methylprednisolone 1 g/dose and 2 pulses of cyclophosphamide 500 and 750 mg/m2/dose). This treatment led to a remission of the edemas and a reduction in proteinuria. Because of the history of deep venous thrombosis, the possibility of antiphospholipid syndrome was entertained. One additional laboratory criterion – moderate positive lupus anticoagulant – was included, but anticardiolipin tested negative on 2 occasions. For this reason, further imaging tests were conducted (angio-CT and arteriography of the upper extremities) and the presence of thrombi was ruled out.
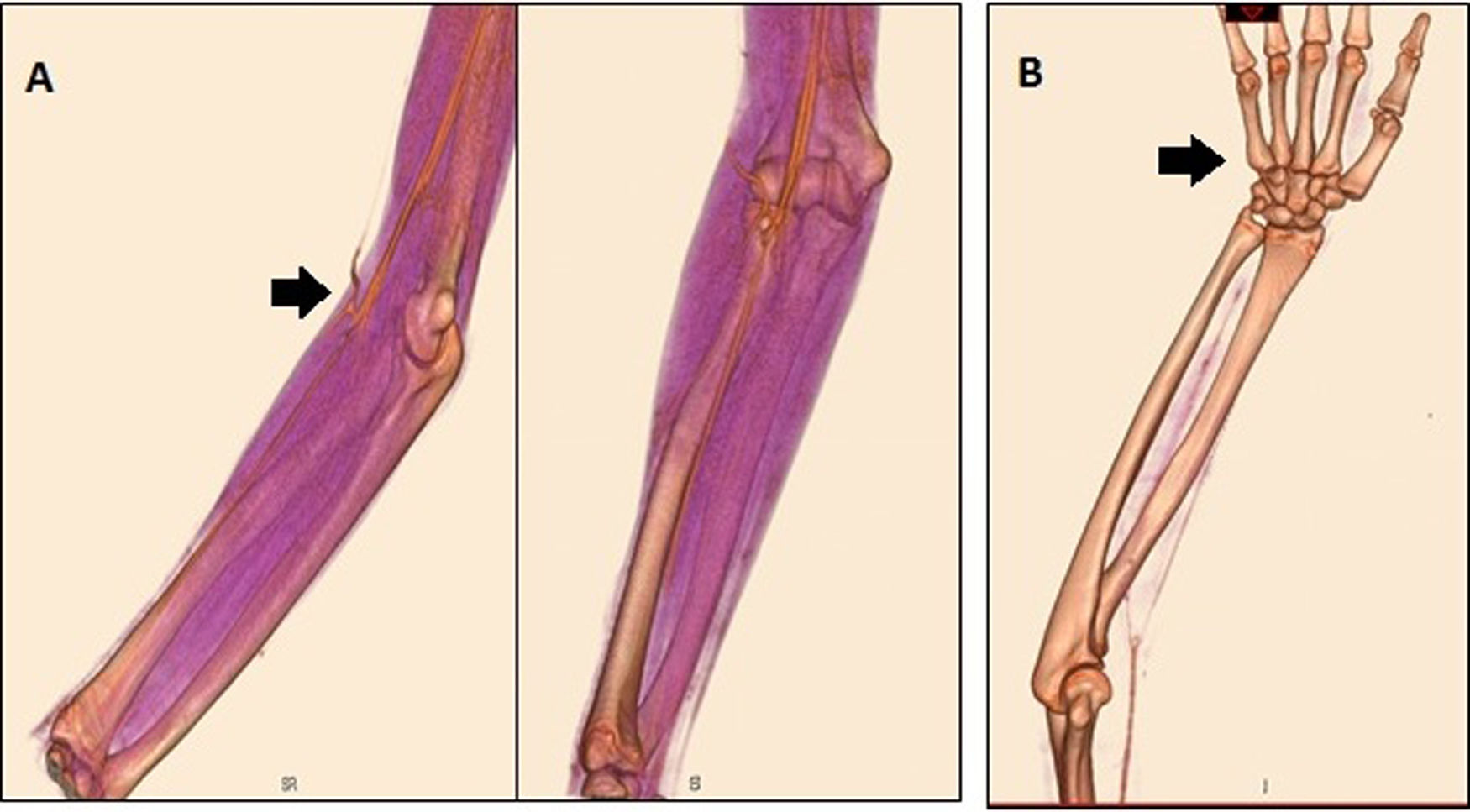
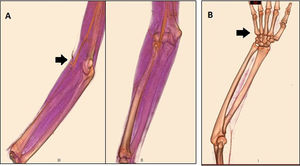
The diagnosis of vasculitis was confirmed by peripheral arteriography with comparative selective catheterization of the upper extremities, evidencing stenosis of the ulnar artery in the proximal third at the bifurcation, in addition to areas of segmental stenosis of the brachial, radial and median arteries of the right arm, and areas of segmental and filamentous-like arterial stenosis in the distal radial artery of the left arm, leading to the diagnosis of arteritis with a predominance of the upper extremities (Fig. 2). The management approach was balloon dilation angioplasty, with favorable recovery and presence of radial pulse (Fig. 3).
PAN is a primary systemic necrotizing vasculitis that predominantly compromises the medium-sized arteries. The clinical presentation ranges from mild forms (purpuras, urticaria lesions, livedo reticularis) to severe forms with systemic compromise.7 The musculoskeletal system, the kidneys, and the gastrointestinal tract are the most affected areas, characterized by frequent relapses.8
In our case, the criteria for the diagnosis of SLE were complemented with SLICC1 6/17 criteria and of the American College of Rheumatology9 4/11. If we consider the EULAR/PRINTO/PRES criteria, our patient meets the PAN criteria (arteriographic findings + skin compromise + renal compromise). Even considering renal compromise as a form of lupus nephritis, the patient still meets 2 criteria needed to consider overlap.
Kumar et al. describe the case of a 17-year old adolescent who was previously healthy, with a history of photosensitivity that developed a condition characterized by mild fever, rash, mouth ulcers, arthritis and necrosis of the first digit of the right foot. The physical examination revealed absent distal pulse in the right femoral artery. The patient progressed to generalized tonic-clonic seizures and the brain MRA showed signs of vasculitis. The MR performed in other vessels showed lumen irregularities in other arteries (renal, superior mesenteric and celiac trunk) and the patient was classified as SLE with extensive medium vessel vasculitis.7 A potential association with PAN was considered in this case, but unlike our patient, this teenager failed to meet at least two criteria.
Nada et al. described a 10-year old girl with fever of one year of evolution and pain in both hands, associated with a history of alopecia, recurrent mouth ulcers, and progressive weight loss over the last year. The physical examination described reduced pulses of the upper limbs, systolic hypertension, anasarca and lymphadenopathies. During the evolution, ANA became positive. The CT angiography of the upper limbs identified long occluded segments in the left brachial artery and distal remodeling of the radial and ulnar arteries. Similar findings were observed in the right side.10
SLE - PAN overlap in children is extremely rare in the literature. There is a Brazilian publication from 2016 of a probable case in a 30-year old data series including 5593 patients in the rheumatology unit,11 and another case in an Indian publication,10 which makes this case noteworthy.
The Ethics Committee of the National Institute of Child Health, Lima, Peru, has reviewed and approved the manuscript. The personal data of the patient are confidential, and informed consent was obtained from her legal guardian. The authors declare they have no conflict of interest.
Conflict of interestsThe authors have no conflict of interests to disclose.
Please cite this article as: Schult Sandra, Genaro Susan, Cajas Mirella, Ponce Patricia. Reporte de un caso de probable overlap de lupus eritematoso sistémico con panarteritis nodosa. Rev Colomb Reumatol. 2020;27:61–64.