Cocaine use is associated with several rheumatic syndromes. A series of cases is presented of 10 patients (7 male and 3 female), age at onset: 19–38 years-old. They consulted due to a variety of symptoms: fever, arthritis, swollen hands, stroke, fetal losses, arterial hypertension, alveolar hemorrhage, leucocytoclastic vasculitis, genital bleeding, among others. Half of them showed positive ANA and Ro antibodies, lymphopenia and positive P-ANCA. Treatments with steroids in bolus, cyclophosphamide and rituximab were used, with a good response. This series highlights clinical manifestations at onset that can mimic primary rheumatic diseases. Rheumatologists should consider cocaine use in the differential diagnoses of vasculitis and pseudovasculitis syndromes.
El uso de cocaína se asocia con varios síndromes reumáticos. Se trata de 10 pacientes (7 varones y 3 mujeres) con una edad al inicio del cuadro entre 19-38 años, quienes consultaron por una variedad de síntomas: fiebre, artritis, tumefacción de manos, accidente isquémico transitorio, pérdidas fetales, hipertensión arterial, hemorragia alveolar, vasculitis leucocitoclástica y hemorragia genital, entre otros. La mitad de estos pacientes presentaron ANA y anticuerpo anti-Ro positivos, linfopenia y p-ANCA positivo. Fueron tratados con corticoides intravenosos en bolo, ciclofosfamida y rituximab, con buena respuesta. Esta serie resalta las manifestaciones clínicas que, al inicio del cuadro, pueden imitar una enfermedad reumática primaria. Los reumatólogos debieran considerar a la cocaína en el diagnóstico diferencial de las vasculitis y los síndromes seudovasculíticos.
Substance abuse is common in some communities and can mimic rheumatic syndromes and vasculitis. In fact, cocaine is a substance that has been associated to the immune response and also with the presence of a variety of syndromes, symptoms and antibodies, such as thrombocytopenia, hemolytic anemia, necrotizing vasculitis, pulmonary hemorrhage, acute renal failure, hemorrhagic stroke, antinuclear antibodies (ANA), antineutrophil cytoplasmic antibodies (ANCA) and antiphospholipid antibodies.1,2 Patients are usually reluctant to admit their cocaine use, leading physicians to overlook cocaine as a cause of disease. Thus, a high clinical suspicion and the knowledge of manifestations secondary to the use of recreational drugs will avoid extensive studies, unnecessary hospitalizations and therapeutic mistakes.3,4
In this report, we describe 10 cases of patients with clinical, immune and laboratory manifestations that were associated with cocaine addiction. This association was confirmed when the patients admitted its use (mostly snorting), when the patient's kin revealed the patient's addiction or when cocaine or its metabolites could be measured in urine.
CasesCase 1: A 38-year-old male cnsulted for erythematous and swollen hands and feet, burning ensation, right Achilles enthesis, cutaneous psoriasis, lymphopenia, eosinophilia and increased titer of CRP. Psoriatic arthropathy was suspected and the patient received anti-inflammatory drugs, without improvement. Of note, the patient started symptoms following cocaine snort. He improved when he quit the use of cocaine.
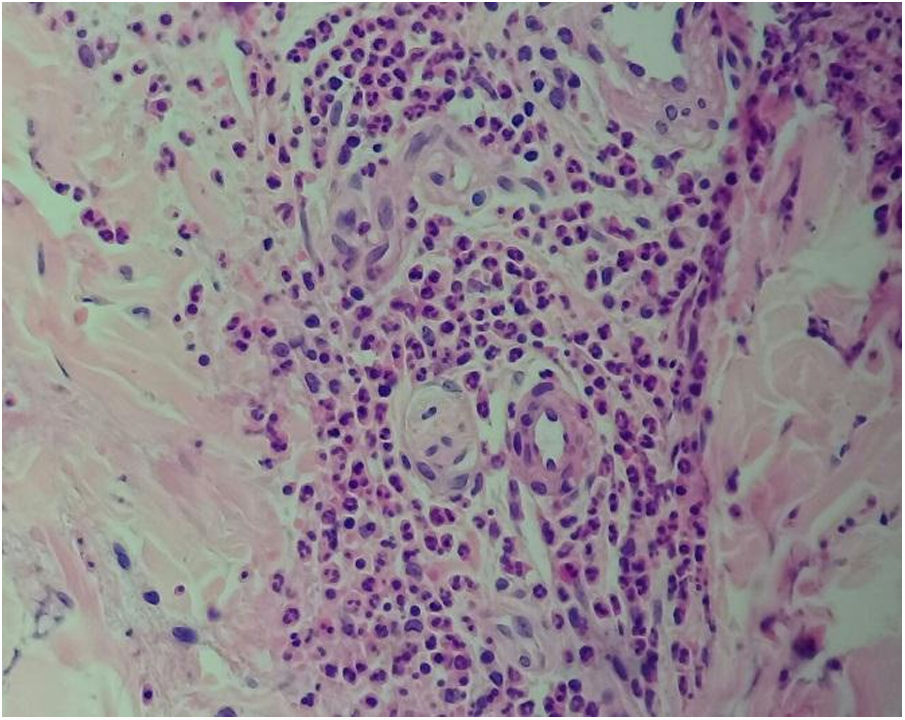
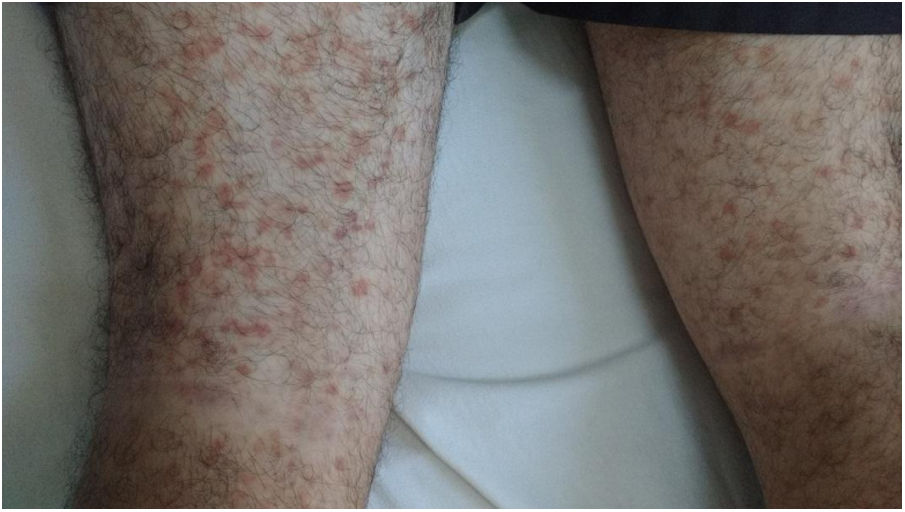
Case 2: A 23-year-old male came to consultation with pharyngitis and palpable purpura in lower limbs, arthralgias, myalgias and abdominal pain; lymphopenia (less of 4000whitecells/mm3) and ANA (+) 1/160 speckled pattern (HeP-2 ELISA). Due to palpable purpura and abdominal pain, an IgA vasculitis was suspected skin biopsy was carried out and the patient received prednisone 1mg/kg/day and methotrexate 15mg/week with good response. Then, we received the histological report: leucocytoclastic vasculitis without deposits of IgA, IgG, IgM and C3 (Figs. 1 and 2).
Later on, the family found cocaine within patient's personal belongings. After improving, the patient did not return to control.
Case 3: A 19-year-old-woman was hospitalized due to ischemic cerebrovascular attack, with motor involvement, two fetal looses, arterial hypertension, aortic aneurysm and renal impairment. Lab results showed the presence of eosinophilia, positive anticardiolipins and Beta 2 glycoprotein I. An antiphospholipid syndrome was suspected and the patient received aspirin, enalapril, atenolol and acenocoumarol. Later on, the patient admitted cocaine addiction. The patient was discharged with a 3 days-dialysis plan and after 18 months of follow-up, she did not return to a rheumatologic control.
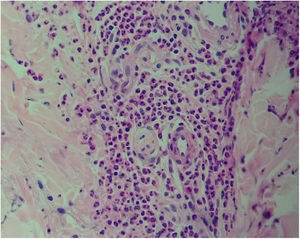
Case 4: A 38-year-old woman came to the emergency room due to shortness of breath, hemoptysis and genital bleeding. Personal history: hyperthyroidism, alcoholism, tobacco and cocaine use during the last 20 years. She presented with fever, petechiae on hard palate and legs, ulcers on nasal septum, liver and spleen enlargement, and ecchymosis. Idiopathic thrombocytopenic purpura was suspected. Lab exams showed anemia, thrombocytopenia (5000k/μl), elevated liver enzymes and positive ANA 1/320 homogeneous pattern (HeP-2-ELISA), C-ANCA (by IIF) and Ro antibodies. Bronchoalveolar lavage confirmed the presence of alveolar hemorrhage, so she was treated with intravenous gammaglobulin, methylprednisone and cyclophosphamide with partial response. The patient developed a cerebrovascular accident in left temporal lobe, with intracranial bleeding. Rituximab 375mg/m2/week for 4 weeks was added, improving the alveolar hemorrhage, thrombocytopenia and neurological event. After 2 years of follow-up, the patient did not return to a control visit (Fig. 3).
Case 5: A 34-year-old male who came to consultation with bleeding gums, fever, testicular pain, purpuric lesions in lower limbs and hematuric urine. Renal biopsy: mesangiocapillary glomerulonephritis with IgG and IgM deposits. Suspected diagnosis: polyarteritis nodosa and vasculitis secondary to cocaine addiction. He was treated with steroids in bolus and intra-venous cyclophosphamide. The patient admitted cocaine addiction. After 7 months of treatment, the patient developed obstructive respiratory failure due to tonsil enlargement (Candida infection) and died.
Case 6: A 33-year-old male who was hospitalized because of weight loss, arthritis, fever, nasal septum perforation, polyserositis, ear necrosis, alveolar hemorrhage, and proliferative extracapilar glomerulonephritis with fibrous crescents with IgM deposits. Systemic lupus erythematosus and vasculitis were suspected and the patient received steroids in bolus and intravenous cyclophosphamide. The symptoms of the patient improved. Later on, he admitted the addiction to cocaine since he was 15 years-old.
Case 7: A 27-year-old male came to consultation with arthralgias and morning stiffness of 30min. With a suspected diagnosis of rheumatoid arthritis, vasculitis or systemic lupus erythematosus, anti-inflammatory drugs were started. The patient returned to consultation after 4 months with hemoptysis and admitting his addiction to cocaine. Alveolar hemorrhage was confirmed by bronchoalveolar lavage. He was hospitalized and received steroids in bolus and intravenous cyclophosphamide and after 2 years of treatment the patient improved.
Case 8: A 33-year-old male addict to cocaine since 4 years ago consulted for fever, arthalgias, myalgias, arthritis, nasal septum perforation, lymph node, liver and spleen enlargement and subcutaneous nodules. Lab results showed the presence of leucopenia, lymphopenia, and ANA positive 1/640 homogeneous pattern (HeP-2 by ELISA). Ro, La, Sm and ds-DNA antibodies: negative results. Systemic lupus erythematosus and vasculitis secondary to cocaine addiction were suspected. The patient quit the habit to consume cocaine; hydroxychloroquine and diclofenac were administrated and his symptoms improved. He did not return to control after 18 months of follow-up.
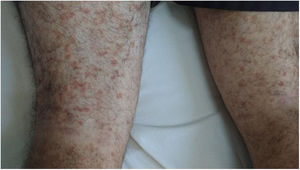
Case 9: A 25-year-old woman hospitalized because of cheek purpuric lesions, cutaneous and ear necrosis, spleen enlargement, fever and alveolar hemorrhage. Positive ANA 1/200 homogeneous pattern (HeP-2 by ELISA), positive P-ANCA 1/5120 (by IIF), positive anti-Ro antibody, anticardiolipin IgM and retrovirus (+). Skin biopsy: cutaneous vasculitis with IgM and complement deposits. Systemic lupus erythematosus and cryoglobulinemic vasculitis were considered, so steroids in bolus and intravenous cyclophosphamide were administered with good results. Later on, the patient admitted cocaine addiction and the urine test was positive for cocaine. After 6 months of treatment, the patient was lost of follow-up (Figs. 4 and 5).
Case 10: A 28-year-old male, alcoholic, addict to cocaine, with cutaneous psoriasis on physical exam and fracture of tibia and fibula that later on developed osteomyelitis, was hospitalized due to headache, fever, arthritis, dyspnea, hemoptoic sputum and pulmonary bilateral infiltration in tomographic scan of thorax. Due to the presence of arthritis and cutaneous psoriasis, a peripheral spondyloarthritis was suspected. Pulmonary thromboembolism and infections were ruled out. An alveolar hemorrhage was confirmed by bronchoalveolar lavage and the patient was treated with high doses of steroids with good response. He also quit the habit of cocaine consumption.
DiscussionDrug addiction is common in many communities and causes significant morbidity and mortality specially associated to harmful physiopathological effects of the substance itself but also by its adulterants.3
The preferred drug among Argentinian users is cocaine (inhaled).5 In Argentina, the greatest impact of freebase cocaine use is on the less fortunate members of society. Its impact has been described as a social consequence of the financial, political and social crisis that lead large numbers of Argentinians to poverty and marginal status.6
According to epidemiologic data the use of cocaine is more frequent among males than females and among 12–24 year-old individuals than in other age groups,7 similar to what was observed in our patients.
Cocaine can induce inflammatory syndrome, vasculitis and/or autoantibody production mimicking primary idiopathic vasculitis.3,8 Although cocaine associated vasculitis is of uncommon occurrence, 50% of our patients presented with purpura, pulmonary hemorrhage, nasal septum perforation and P-ANCA (+). The use of cocaine can be associated with an ANCA (+) vasculitis and pseudovasculitis with special specificity for human neutrophil elastase (HNE-ANCA). This ANCA shares sequence and structural homology with the classic C-ANCA associated antigen PR-3 and would be present in vasculitis induced by cocaine use,9 allowing to differentiate between both types of vasculitis. HNE-ANCA could not be measured in the present study.
Clinical manifestations depend on the way cocaine is administered (the majority of this patients used inhalatory route). The presence of purpuric lesions, thrombocytopenia, neutropenia, elevated erythrosedimentation rate and PCR is attributed to levamisole (anthelmintic substance used to adulterate cocaine) more than to cocaine itself.10 These findings were noted in our patients but we could not prove the presence of this additive in our series. Association between levamisole and renal and pulmonary lesions was rarely present.11 On the contrary, neurological and cardiovascular lesions were attributed directly to cocaine.2
Treatment is supportive but patients should stop their addiction.
More severe lesions may benefit with high steroids doses (although steroids benefits are not so clear) and/or immunosuppression, plasmapheresis and surgical debridement of areas of cutaneous necrosis.1
We could not determine in the present series if patients had quit the use of cocaine, since half of them were lost of follow-up. The majority of them had been treated with I.V. steroids and immunosuppressants (cyclophosphamide, methotrexate, rituximab, I.V. gammaglobulina) with good response.
Awareness of the effects produced by cocaine and/or adulterants will allow suspecting it when an ANCA (+) vasculitis (or not) occurs in a young person.
Rheumatologists should consider cocaine in the differential diagnoses of vasculitis12 and pseudovasculitis syndromes (cholesterol embolia, atrial myxoma, bacterial endocarditis, calciphylaxis, paraneoplastic syndromes, antiphospholipid syndrome, organ transplant rejection, ergot abuse, amyloidosis and fibromuscular dysplasia, among other causes).
FundingThere is no pharmaceutical or industry support.
We do not receive any support from the National Institutes of Health (NIH), Wellcome Trust, Howard Hughes Medical Institute (HHMI).
Conflict of interestNone declared.
The authors are grateful to Ricardo Jiménez MD (Assistant Professor; UC, Irvine Department of Pathology) for his help in translating this manuscript.