Rheumatoid arthritis (RA) is a burdensome disease from both individual and societal perspectives, in which access to a rheumatologist plays a pivotal role in disease activity and reduction of its impact. We describe preliminary results of our study aimed at exploring whether healthcare regime affiliation influences disease outcomes of Colombian patients with RA.
Materials and methodsWe performed a retrospective observational study of RA patients (2010 ACR/EULAR classification criteria) with at least 3 assessments in rheumatology clinics from different healthcare regimes: Contributory (CR), Subsidized (SR), a centre of clinical excellence (C3) that follows CR patients. We retrieved data from clinical charts including a follow-up period of 2 years.
ResultsWe included one hundred and sixty patients (C3: 79 [49.4%], CR: 26 [16.2%], SR: 55 [34.2%]). Median initial age was 54 years (IQR 48–62) and most patients were women (77.8%). Of the patients, 79% had established RA and 70% had high disease activity at the beginning of the follow-up. We observed statistical differences between groups with regards to (1) median time to scheduled visits, (2) percentage of visits accomplished in scheduled time, (3) median time to real visit, (4) adherence, (5) median percentage of time in high disease activity, and (6) percentage of patients in high disease activity at the end of follow-up. The best outcomes were observed in the C3 cohort.
ConclusionsAccess opportunity and clinical outcomes of Colombian patients with RA appear to differ between healthcare regimes. Although systematic bias may be present due to sample size, these data imply the healthcare regime is a major determinant of disease outcomes.
La artritis reumatoide (AR) presenta una alta carga de enfermedad tanto desde una perspectiva individual como social. La posibilidad de acceder a un reumatólogo desempeña un papel fundamental en la actividad de la enfermedad y la reducción de su impacto. Se describen los resultados preliminares de un estudio que tiene por objetivo explorar la influencia del régimen de afiliación en salud en los desenlaces de la enfermedad en pacientes colombianos con AR.
Materiales y métodosSe realizó un estudio observacional retrospectivo en pacientes colombianos con AR (criterios de clasificación ACR/EULAR 2010), con al menos 3 consultas por reumatología, en 3 servicios ambulatorios de diferentes regímenes de atención: contributivo (RC), subsidiado (RS) y un centro de cuidado clínico de excelencia (C3). Se recogieron datos de las historias clínicas, incluyendo un periodo de seguimiento de 2 años.
ResultadosSe incluyó un total de 160 pacientes (C3: 79 [49,4%], RC: 26 [16,2%], RS: 55 [34,2%]). La mediana de la edad inicial fue de 54 años (RIC 48-62) y la mayoría fueron mujeres (77,8%). El 79% de los pacientes tenía AR establecida y el 70% presentaba una alta actividad de la enfermedad al inicio del seguimiento. Se encontraron diferencias estadísticas entre los grupos en: 1) la mediana del tiempo programado para la siguiente consulta; 2) el porcentaje de las consultas cumplidas en el tiempo previsto; 3) la mediana del tiempo real en consulta; 4) la mediana de la adherencia a la toma de laboratorios; 5) la mediana del porcentaje de tiempo durante el seguimiento en alta actividad, y 6) el porcentaje de pacientes con alta actividad al final del seguimiento. Los mejores desenlaces se observaron en el grupo C3.
ConclusionesLa oportunidad de acceso y los desenlaces clínicos de pacientes colombianos con AR parecen diferir según el régimen de afiliación en salud. Aunque puede existir un sesgo sistemático debido al tamaño de la muestra, estos datos apuntan a que el régimen de afiliación en salud es un determinante mayor en los desenlaces de la enfermedad.
Rheumatoid arthritis (RA) is a chronic autoimmune systemic disease with a high burden of disease and a prevalence close to 1% in Colombia.1–3 Current national and international management guidelines support the pivotal role of the rheumatologist as “the specialist who should primarily care for patients with RA”; thus, opportune access is crucial.4,5 The healthcare system structure and, whenever appropriate, the type of insurance influence the access of patients to an adequate standard of care.6,7
Currently, it is estimated that 95% of the Colombian population is covered by the healthcare system.8 Colombian residents are allocated to one of the following three affiliation regimes: (1) contributory regime (CR), in which formal workers contribute with a percentage of their wage to have access to healthcare services and to finance the national fund. They have the alternative to affiliate to private insurance companies for additional benefits; (2) subsidized regime (SR), in which the low income and vulnerable population is affiliated and have access to the system by means of the resources from the national fund; and (3) the special benefit regime, which covers military forces, teachers, and workers from the national petroleum company. Differences in access to health services are often perceived by the users. In addition, recent data have shown differential clinical outcomes between the insurance regimes.9,10
As a response to the poor performance of healthcare systems in Latin America aiming to manage chronic diseases, the creation of Centers of Excellence for the treatment of these pathologies were proposed as a strategy to improve healthcare outcomes. Centers of Excellence are highly specialized comprehensive care units aiming to give an integrative approach to the management of patients with chronic diseases in an effective and efficient way. These units make an active search of patients with the disease in order to concentrate the population, ensure a multidisciplinary approach to their management through standardized guidelines and protocols, always trying to achieve a responsible and efficient use of the limited resources available.11 The implementation of Centers of Excellence have been proposed as a feasible alternative to improve clinical outcomes of patients with RA, regardless of their healthcare affiliation regime.12,13 To the best of our knowledge, evidence supporting differences in clinical outcomes between regimes in RA is lacking.14 Thus, we aimed at exploring access opportunities and disease outcomes of Colombian patients with RA, based on their healthcare regime affiliation; hereby, we present our preliminary results.
Materials and methodsStudy design and populationThis was a retrospective observational study of Colombian patients who were 18 years of age or older with a diagnosis of RA based on the 2010 ACR/EULAR classification criteria and with at least 3 assessments by a rheumatologist (including the first assessment and follow-up appointments) for a period of 2 years. Clinical charts from three outpatient services were assessed: (1) Contributory regime (CR): outpatient rheumatology consultation from a healthcare provider institution affiliated to a contributory regime insurance company in Bogota D.C, Colombia; (2) Subsidized regime (SR): North Hospital sub-network in Bogota D.C, Colombia; (3) Excellence Clinical Care Center (C3): RA Clinical Care Center at the Fundación Santa Fe de Bogota University Hospital in Bogota D.C, Colombia (Patients belonged to the CR).
Data collectionWe performed a convenience sampling strategy, in which clinical charts were included and assessed in a chronologically order (i.e., from the oldest to the newest appointment). We retrieved the following variables: age, sex, healthcare regime, RA classification, number of appointments, previous treatment with disease-modifying anti-rheumatic drugs (DMARD), disease activity at each appointment, lag times between appointments (scheduled and real), number of appointments accomplished on time, adherence to treatment, and accomplishment of follow-up laboratories. Based on the definitions given by the Colombian Clinical Practice Guideline for the diagnosis and management of RA,4 early RA was defined as a patient with symptoms onset within the first year prior to diagnosis. Prior DMARDs use was defined as a patient who was receiving any DMARD prior to the first appointment.
Disease activityDisease activity was measured with multiple endorsed disease activity indices, including DAS-28 (ESR or C-RP), CDAI and SDAI, as laboratories were not available in every appointment. Disease activity was defined as the qualitative interpretation of any of the indices (i.e., remission, low, moderate, or high activity). We categorized disease activity as ‘high activity’ when the score category was either moderate or high, and ‘low activity’ when the score category was either low or remission.15–17 The proportion of patients with high disease activity at the first and the last visit were calculated. In addition, the percentage of time in high disease activity was calculated, which was estimated considering that disease activity between two appointments was equal to the measured activity at the first of these visits. Then, we summed up only the days between those appointments considered as ‘at high disease activity’, and this sum was divided by the total days of follow-up (i.e., from the first to the last appointment).
Lag timesWe calculated the days between appointments (i.e., lag times) for two scenarios: scheduled and real appointments. A ‘scheduled appointment’ was considered as a visit that occurs within the time indicated by the treating rheumatologist (i.e., expected date or earlier). A ‘real appointment’ is the real time elapsed between consultation and the next follow-up appointment. The proportion of appointments accomplished on time (i.e., ‘scheduled appointment’) was also calculated.
AdherenceSelf-reported medication adherence was collected from the clinical record: If a patient was not taking their medication (due to self-choice or lack of dispensation), this information was written by the treating rheumatologist. For laboratory adherence, the patients were told to attend the samplings to monitor safety (typically, complete blood count, acute phase reactants, transaminases, etc.), to confirm the diagnosis (e.g., anti-CCP, rheumatoid factor, etc.) or for individualized circumstances. The information of the requested laboratories was collected at each visit, and the recorded results in the next follow-up. Thus, the complete accomplishment was considered when all the requested laboratories were recorded.
Statistical analysisWe summarized variables with descriptive statistics, percentages, median and interquartile ranges. We explored statistical differences between groups using the Chi-squared test (X2) or Kruskal–Wallis equality of populations rank test. As we performed multiple comparisons, we applied the Bonferroni's test to determine significant findings. We considered p values<0.05 as significant. We performed statistical analyses using GraphPad Prism 8.0 for Mac.
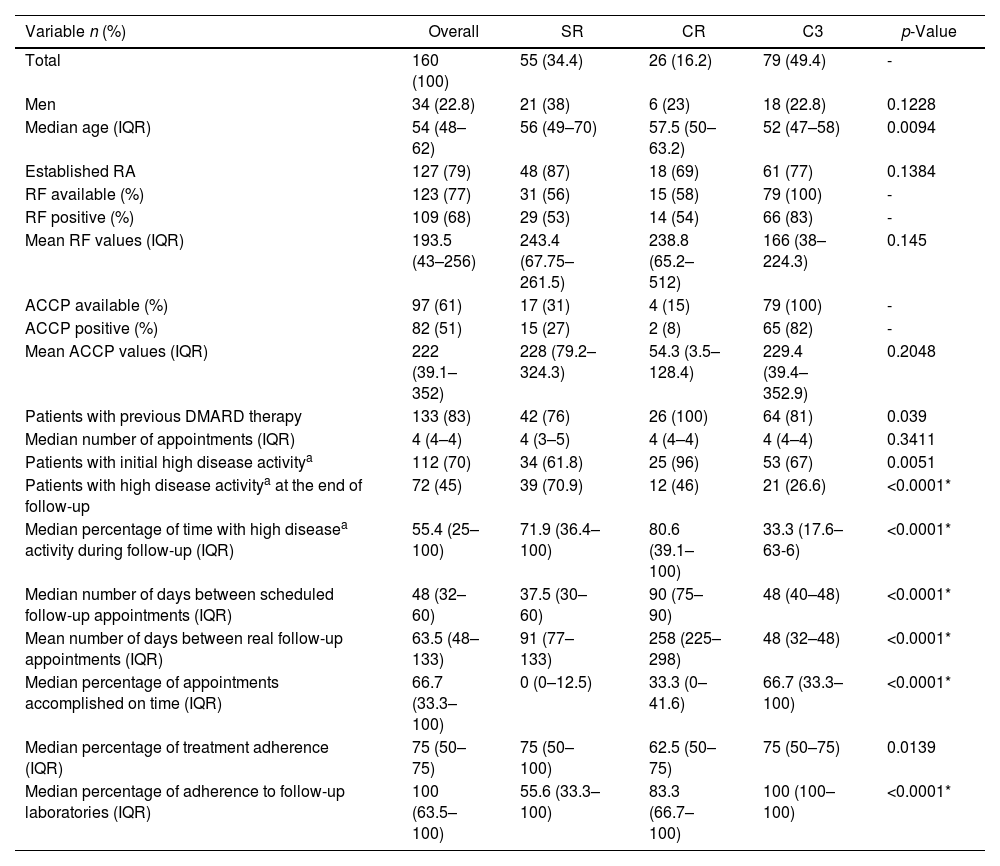
ResultsWe included a total of 160 patients (C3: 79, CR: 26, SR 55 [34%]). Demographic characteristics are summarized in Table 1. Male patients constituted 22.8% of patients. The median initial age of the overall cohort was 54 years (IQR 48–62). Based on the onset of symptoms, 21% (33 patients) of patients had early RA, with the higher proportion in the CR group (31%) and the lowest proportion in SR (13%). At the time of the first visit, previous DMARD therapy was being received by 83% of patients and most patients (70%) had a high disease activity. The median number of appointments for patients during the 2 years follow-up period was 4 in all the groups.
Demographic and clinical variables assessed for overall, Subsidized, Contributory and Excellence Clinical Care Center healthcare regime in Colombian patients with RA.
| Variable n (%) | Overall | SR | CR | C3 | p-Value |
|---|---|---|---|---|---|
| Total | 160 (100) | 55 (34.4) | 26 (16.2) | 79 (49.4) | - |
| Men | 34 (22.8) | 21 (38) | 6 (23) | 18 (22.8) | 0.1228 |
| Median age (IQR) | 54 (48–62) | 56 (49–70) | 57.5 (50–63.2) | 52 (47–58) | 0.0094 |
| Established RA | 127 (79) | 48 (87) | 18 (69) | 61 (77) | 0.1384 |
| RF available (%) | 123 (77) | 31 (56) | 15 (58) | 79 (100) | - |
| RF positive (%) | 109 (68) | 29 (53) | 14 (54) | 66 (83) | - |
| Mean RF values (IQR) | 193.5 (43–256) | 243.4 (67.75–261.5) | 238.8 (65.2–512) | 166 (38–224.3) | 0.145 |
| ACCP available (%) | 97 (61) | 17 (31) | 4 (15) | 79 (100) | - |
| ACCP positive (%) | 82 (51) | 15 (27) | 2 (8) | 65 (82) | - |
| Mean ACCP values (IQR) | 222 (39.1–352) | 228 (79.2–324.3) | 54.3 (3.5–128.4) | 229.4 (39.4–352.9) | 0.2048 |
| Patients with previous DMARD therapy | 133 (83) | 42 (76) | 26 (100) | 64 (81) | 0.039 |
| Median number of appointments (IQR) | 4 (4–4) | 4 (3–5) | 4 (4–4) | 4 (4–4) | 0.3411 |
| Patients with initial high disease activitya | 112 (70) | 34 (61.8) | 25 (96) | 53 (67) | 0.0051 |
| Patients with high disease activitya at the end of follow-up | 72 (45) | 39 (70.9) | 12 (46) | 21 (26.6) | <0.0001* |
| Median percentage of time with high diseasea activity during follow-up (IQR) | 55.4 (25–100) | 71.9 (36.4–100) | 80.6 (39.1–100) | 33.3 (17.6–63-6) | <0.0001* |
| Median number of days between scheduled follow-up appointments (IQR) | 48 (32–60) | 37.5 (30–60) | 90 (75–90) | 48 (40–48) | <0.0001* |
| Mean number of days between real follow-up appointments (IQR) | 63.5 (48–133) | 91 (77–133) | 258 (225–298) | 48 (32–48) | <0.0001* |
| Median percentage of appointments accomplished on time (IQR) | 66.7 (33.3–100) | 0 (0–12.5) | 33.3 (0–41.6) | 66.7 (33.3–100) | <0.0001* |
| Median percentage of treatment adherence (IQR) | 75 (50–75) | 75 (50–100) | 62.5 (50–75) | 75 (50–75) | 0.0139 |
| Median percentage of adherence to follow-up laboratories (IQR) | 100 (63.5–100) | 55.6 (33.3–100) | 83.3 (66.7–100) | 100 (100–100) | <0.0001* |
Abbreviations: SR: subsidized regime; CR: contributory regime; C3: Excellence Clinical Care Center; IQR: Interquartile Range; n: number of patients; %: percentage; RA: rheumatoid arthritis; DMARD: Disease Modifying Anti-Rheumatic Drugs; RF: Rheumatoid factor; ACCP: anti-cyclic citrullinated protein antibodies.
Significant differences between groups were observed with regard to (1) the median number of days between scheduled follow-up appointments (p<0.0001), with the longest periods among patients from the CR; (2) the median number of days between real follow-up appointments (p<0.0001), which were higher when compared to the scheduled ones, being longest among patients from the CR group; (3) the median percentage of follow-up appointments accomplished (p<0.0001), which was particularly low in SR group (0%); (4) the median percentage of adherence to laboratories (p<0.0001), which was particularly high among C3 group patients; (5) the median percentage of time in high disease activity (p<0.0001), being shorter in the C3 group; and (6) the percentage of patients in high disease activity at the end of follow-up (p<0.0001), which was exceptionally high (almost 80%) in the SR group.
DiscussionDifferences in access opportunities and clinical outcomes of Colombian patients with RA appear to be present, and to be influenced by the type healthcare regime affiliation. A positive influence appears to be present for patients being followed at a Center of Excellence (i.e., C3 group) and to be particularly negative for the most vulnerable patients (i.e., SR).
Based on data up to January 2020, almost 48% of Colombian population have access to the healthcare system through affiliation to the SR.8 Our results suggest that RA patients in this regime present a lower access opportunity and worse clinical outcomes. For instance, this population appear to have a lower adherence to medications and follow-up laboratories, and to spent more time in high disease activity, thus suggesting the existence of disparities in healthcare due to insurance status. Previous reports have informed that healthcare insurance is a major determinant of disease outcomes. One example was reported by Cifaldi and colleagues, indicating that patients with Medicaid insurance in the United States were less likely to have access to rheumatology consultation, also DMARDs were less prescribed and obtention of drugs was more difficult, generating poor health outcomes in patients with RA.7 Nonetheless, one shall not forget that this population may present confounding factors, that may influence outcomes. For instance, a lower socio-economic level has been widely associated with poorer outcomes in RA (6). Excellence Clinical Care Centers may be implemented in our country to counteract healthcare structural barriers.12,18 In line with our results, Santos et al. previously reported improvement in clinical outcomes using this model.13
Our study has some limitations. First, as a retrospective observational study, recall bias may be present, as the information was retrieved from clinical charts. Second, systematic bias may be present due to the small sample in the CR group, and lack. Further efforts are being executed to overcome these statistical barriers. Nonetheless, to the best of our knowledge, this study is the first attempt in our country to explore the impact of the healthcare regime on clinical outcomes in patients with RA.
ConclusionHealth inequity poses the most vulnerable social groups in a greater disadvantage to access healthcare. The affiliation to healthcare appears to mediate this phenomenon in Colombian patients with RA. Excellence Clinical Care Centers could be an alternative to overcome this issue.
Funding sourcesThis study was funded with a grant from the Colombian Association of Rheumatology.
Conflict of interestNo conflict of interests was declared by the authors.