Granulomatosis with polyangiitis (GPA) and pyoderma gangrenosum are rare and difficult-to-diagnose pathologies with severe manifestations and a high burden of morbidity. GPA is a necrotizing systemic vasculitis of small vessels, while pyoderma gangrenosum is an inflammatory skin disease.
ObjectivesThe aim of this study is to describe the comprehensive clinical-pathological study process necessary to accurately identify these conditions and establish an effective treatment plan.
Materials and methodsA retrospective study was conducted on a case of a patient with cutaneous lesions suspected of pyoderma gangrenosum. Clinical data, including symptoms, laboratory tests, biopsies, and imaging results, were collected. A multidisciplinary review of the findings was carried out to reach an accurate diagnosis. The treatment consisted of administering methotrexate.
ResultsFollowing the comprehensive clinical-pathological study, the diagnosis of granulomatosis with polyangiitis associated with pyoderma gangrenosum-like lesions was confirmed. The patient responded favourably to methotrexate treatment, and the cutaneous lesions completely resolved after one year.
ConclusionsThis case illustrates the difficulty in diagnosing granulomatosis with polyangiitis and pyoderma gangrenosum, highlighting the importance of a multidisciplinary approach in their management. The comprehensive clinical-pathological study and appropriate treatment led to successful resolution of the patient’s lesions. It is crucial to promote collaboration among different medical specialties to improve the diagnosis and treatment of these rare and highly morbid diseases.
La granulomatosis con poliangeítis (GPA) y el pioderma gangrenoso son patologías raras y difíciles de diagnosticar, con manifestaciones graves y una alta carga de morbilidad. La GPA es una vasculitis sistémica necrosante de pequeños vasos, y el pioderma gangrenoso es una enfermedad inflamatoria de la piel.
ObjetivosSe busca describir el proceso de estudio clínico-patológico exhaustivo necesario para identificar correctamente estas condiciones y establecer un plan de tratamiento efectivo.
Materiales y métodosSe realizó un estudio retrospectivo del caso de una paciente con lesiones cutáneas sospechosas de pioderma gangrenoso. Se recopilaron los datos clínicos, incluyendo síntomas, estudios de laboratorio, biopsias y resultados de imagen. Se llevó a cabo una revisión multidisciplinaria de los hallazgos para llegar a un diagnóstico preciso. El tratamiento consistió en la administración de metotrexato.
ResultadosTras un estudio clínico-patológico exhaustivo, se confirmó el diagnóstico de granulomatosis con poliangeítis asociada con lesiones similares al pioderma gangrenoso. La paciente respondió favorablemente al tratamiento con metotrexato, y las lesiones cutáneas se resolvieron por completo al cabo de un año.
ConclusionesEste caso ilustra la dificultad del diagnóstico de la granulomatosis con poliangeítis y el pioderma gangrenoso, y destaca la importancia de un enfoque multidisciplinario en su manejo. El estudio clínico-patológico exhaustivo y el tratamiento adecuado permitieron una resolución exitosa de las lesiones en la paciente. Es fundamental promover la colaboración entre diferentes especialidades médicas para mejorar el diagnóstico y el tratamiento de estas enfermedades raras y de alta morbilidad.
Granulomatosis with polyangiitis (GPA) is a necrotizing vasculitis of small vessels, associated with anti-neutrophil cytoplasmic antibodies (ANCA) and multisystem involvement, predominantly in the respiratory and genitourinary tract. Cutaneous involvement occurs in 30%–50% of patients; the most frequent manifestation is palpable purpura.1 Pyoderma gangrenosum is a rare neutrophilic dermatosis characterized by the development of papules or pustules that subsequently form painful ulcers with undermined edges and peripheral edema.2 It is a diagnosis that requires the exclusion of other inflammatory and ulcerative diseases.
There are few case reports documenting pyoderma gangrenosum-like lesions in patients with GPA, which presents a diagnostic challenge due to overlapping manifestations and the need for extensive histopathologic studies.3 We present the case of a patient with GPA-like ANCA vasculitis and pyoderma gangrenosum-like skin lesions.
Case presentationWe present the case of a 55-year-old woman referred to the emergency department of our institution for hematology, who presented with a condition of 8 months’ duration characterized by the appearance of painful nodules that subsequently ulcerated. The nodules were located on the face, oral mucosa, pubis, and extremities (Fig. 1), associated with unintentional loss of 10 kg of weight and nocturnal diaphoresis under suspicion of lymphoproliferative syndrome by a histological study performed on an outpatient basis.
Evolution of the primary lesion on the right forearm. (A) Initial lesion with its progression prior to institutional assessment (photos taken by the patient and published under her consent). (B) Ulcer progression with deep tissue exposure during hospital stay (photos taken under patient’s consent). (C) Outpatient evolution under treatment with steroid and methotrexate (photos taken by the patient and published under her consent).
She had been under outpatient follow-up by other institutions due to the appearance of an ulcer (Fig. 1A) 4 years earlier, after a traumatic fracture of the right distal radius, which required an open reduction and a skin flap due to a covering defect. His evolution had been sluggish due to recurrent osteomyelitis, and he developed a skin fistula that was under ambulatory management.
On admission to our institution, the patient was hemodynamically stable, but with multiple ulcerated and necrotic lesions on the face, right forearm, right pinna, pubis, and feet (Fig. 1 and 2). In the histology report of the biopsy of the forearm ulcer, there was suspicion of atypical T lymphoma due to the presence of atypical and angiocentric T lymphoid infiltrate, with a uniform granulomatous component in all samples. No alterations were found in the admission paraclinical and extension studies, while viral infections (hepatitis B and C, syphilis and HIV) were negative.
Lesions documented in the physical examination on admission to our institution. (A) In the right nasolabial region there is a small ulcer with yellowish cordoned edges. In the melolabial sulcus there are also two depressed brownish plaques of cicatricial aspect. (B) Distal necrosis of the hallux of the left foot. (C) Large ulcer in pubic and suprapubic region with violaceous borders, edematous to the cruciate periphery, and in the center with granulation tissue.
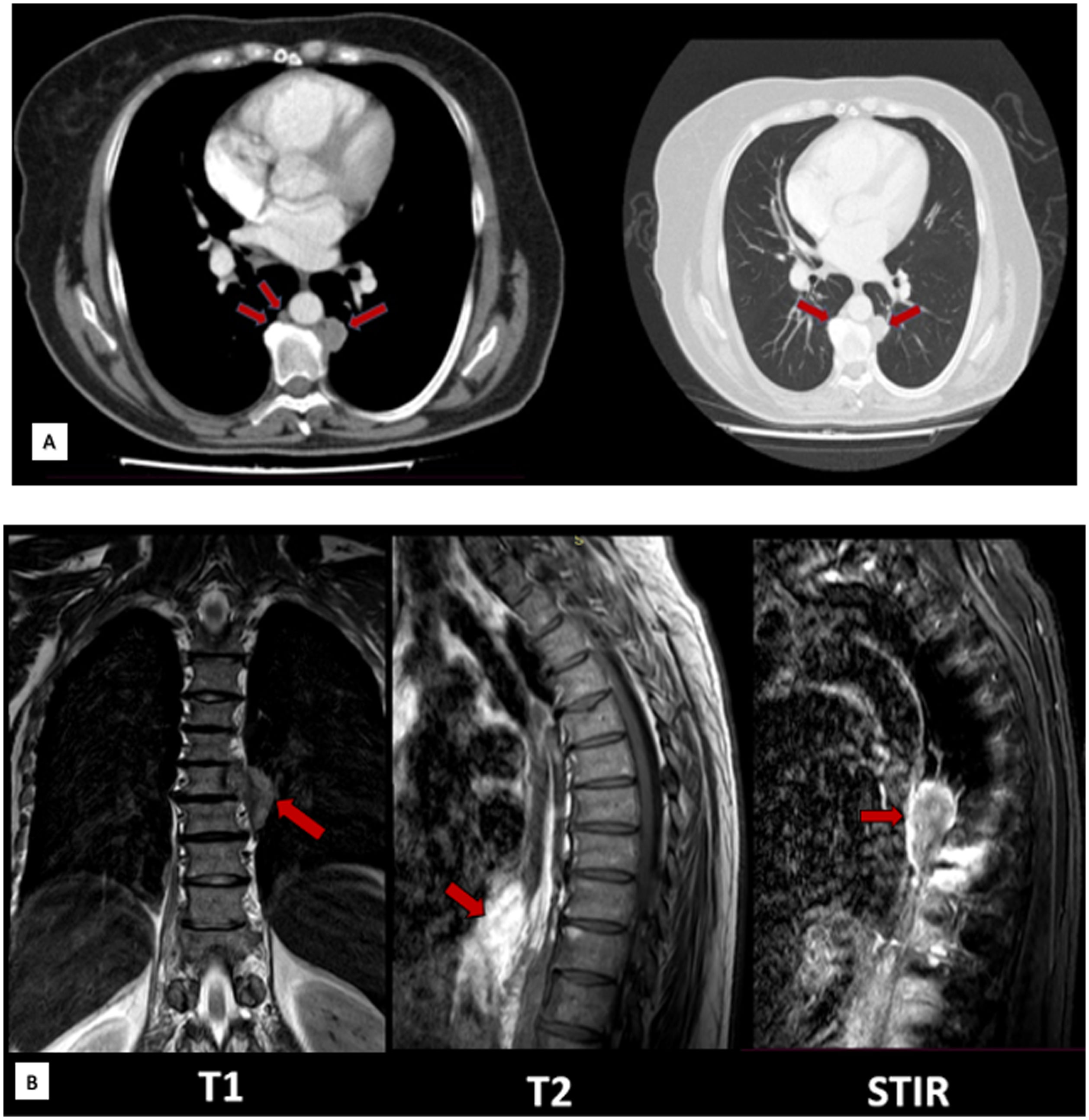
Given the histological findings provided by the patient, it was decided to carry out extension studies for the lymphoproliferative syndrome, the results of which showed a bone marrow biopsy without alterations and staging studies that only in the thorax documented a paravertebral mass (Fig. 3), which was better characterized with magnetic resonance imaging (Fig. 3). After that, the patient was scheduled for a biopsy by thoracic surgery, which documented a mass in the upper segment of the left lower lobe of the lung with a necrotic appearance (abscessed vs. caseating vs. tumorous).
Paravertebral masses documented on imaging. (A) Contrasted chest CT: arrows indicate paravertebral soft tissue thickening, with a nodular lesion with soft tissue density of 18 × 18 mm, partially surrounding the aorta, prevertebral masses in T9, T11, and T12 in the mediastinal (left) and pulmonary (right) window, with nonspecific features. (B) Contrast MRI of the dorsal spine: hypodense bone marrow infiltrative lesions (arrows) in T1 and hypertensive with enhancement in T2 and STIR, involving the vertebral bodies T7, T10, T11, T12, and L1.
Due to a previous history of osteomyelitis in the right forearm, the patient was evaluated by orthopedics and plastic surgery, who requested extension studies due to fever during the hospital stay, as well as the elevation of acute phase reactants, with resonance findings of the forearm. Bone cultures showed that along with the mass, the patient had infectious osteomyelitis due to Escherichia coli, for which he was treated with ertapenem, after which he experienced clinical improvement.
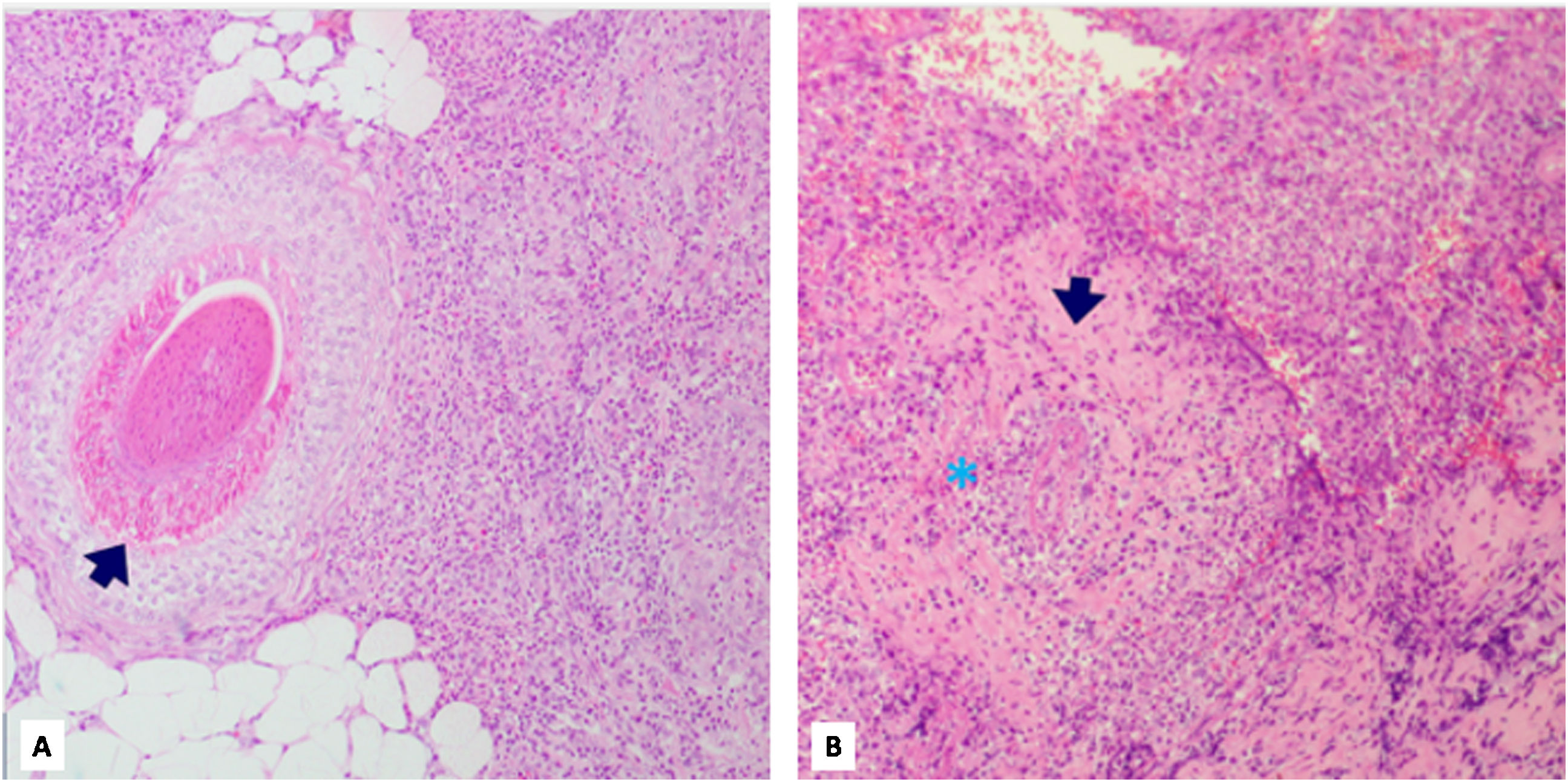
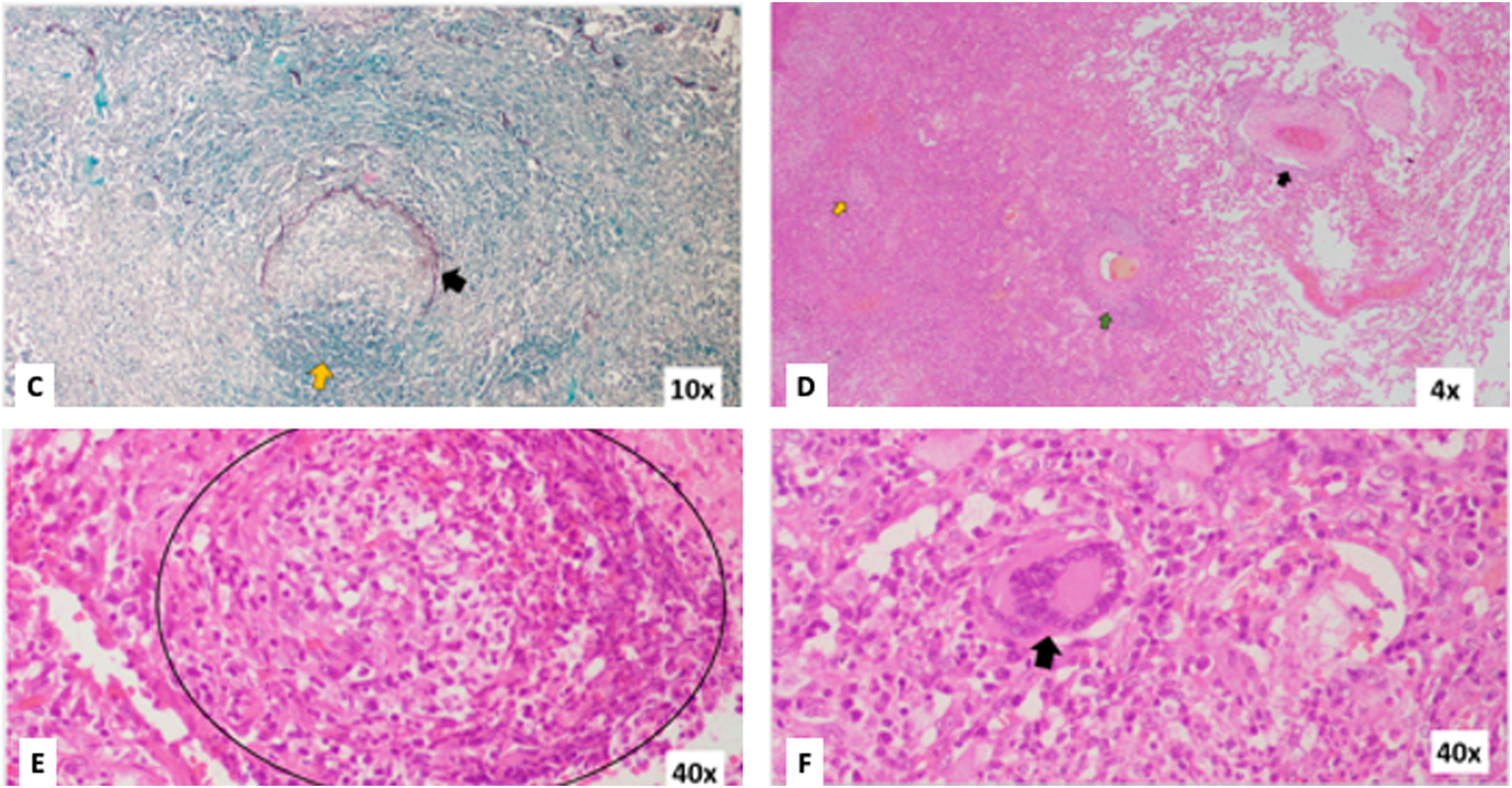
During the month of hospital stay and despite antibiotic treatment for osteomyelitis, the lesion on the right forearm worsened. The patient showed patergia phenomenon (clinical worsening after washing and debridement for osteomyelitis) and peripheral edema with purplish borders, suggesting the differential diagnosis of pyoderma gangrenosum (Fig. 1B). As a result, skin biopsies were repeated and showed a granulomatous inflammatory infiltrate with multinucleated giant cells in a mixed background of lymphocytes, plasmacytes, eosinophils, and neutrophils with abscess formation, with no signs of neoplasia on immunohistochemistry or clonality and EBER FISH studies (Fig. 4). On the other hand, lung biopsies documented granulomatous inflammation and necrotizing vasculitis (Fig. 5). In both cases, microbiological studies were negative for common germs, fungi, and typical and atypical mycobacteria.
Skin biopsies. (A) Hematoxylin/eosin stain. 4×. The arrow shows a deep dermal vessel involved by a mixed inflammatory infiltrate with a predominance of neutrophilic polymorphonuclear neutrophils (PMN) and fibrinoid wall damage. (B) Hematoxylin/eosin stain. 10×. A vessel totally compromised by a mixed inflammatory infiltrate, especially PMN, and with fibrinoid damage of the wall (arrow and asterisks).
Lung biopsies. (C) Elastic staining. 10×. Arrow shows vascular walls with partial destruction of their wall by a polymorphonuclear–neutrophilic–dominated inflammatory infiltrate; a crescent image of the elastic layer remains. (D) Hematoxylin/eosin stain. 4×. On the right, normal lung parenchyma is observed, with a preserved vessel (black arrow). On the left, there is a dense inflammatory infiltrate that destroys the pulmonary parenchyma, with the involvement of vascular structures (green arrow) and granuloma formation (yellow arrow). (E) Hematoxylin/eosin stain. 40×. The circle shows true granuloma formation with histiocytes, polymorphonuclear neutrophils, plasmacytes, and lymphocytes. (F) Hematoxylin/eosin staining. 40×. The arrow shows a multinucleated giant cell in granulomas.
The above, together with the lesions on physical examination, raised the suspicion of an autoimmune-inflammatory etiology as a differential diagnosis; so, antibodies were requested since it was thought that an ANCA vasculitis could be present; of these antibodies, the antiproteinase 3 (anti-PR3) antibodies were positive (13.3 mg/dl). In the absence of hematolymphoid neoplasia, in addition to negative microbiological studies and histological findings associated with anti-PR3, it was considered a granulomatosis with polyangiitis, with lesions similar to pyoderma gangrenosum. Management was initiated with prednisolone at a dose of 1 mg/kg/day, methotrexate 15 mg/week, and the antibiotic course for osteomyelitis was completed. The patient had a favorable in-hospital evolution, so she was discharged with a multidisciplinary outpatient follow-up. At follow-up after 6 months, improvement of skin lesions and resolution of constitutional symptoms were satisfactory with methotrexate (15 mg/week) and prednisolone (15 mg/day) treatment (Fig. 1C).
DiscussionThe patient had a course similar to that described in pyoderma gangrenosum, with an insidious appearance of nodules and subsequent ulceration. In 15%–30% of patients, pathergia4,5 has been described, consisting of the appearance or exacerbation of lesions on trauma sites,2,6 which was notorious in the patient’s right forearm, where she had undergone multiple operations. Among the histopathological findings described in the literature, the presence of perivascular neutrophilic and lymphocytic infiltrate with predominantly neutrophilic dermal edema6 stands out, similar to what was documented in the biopsies of the patient, who also had a significant granulomatous component.
Debut with cutaneous manifestations in GPA is infrequent. A retrospective case series in the United States identified a prevalence of cutaneous involvement ranging from 4.4% to 40%, being more frequent in the generalized forms of the disease.7 Likewise, a Spanish retrospective case series identified 39 patients with GPA, of whom 53.85% presented cutaneous manifestations; more than 50% of these also had pulmonary involvement, as was the case in our patient.8
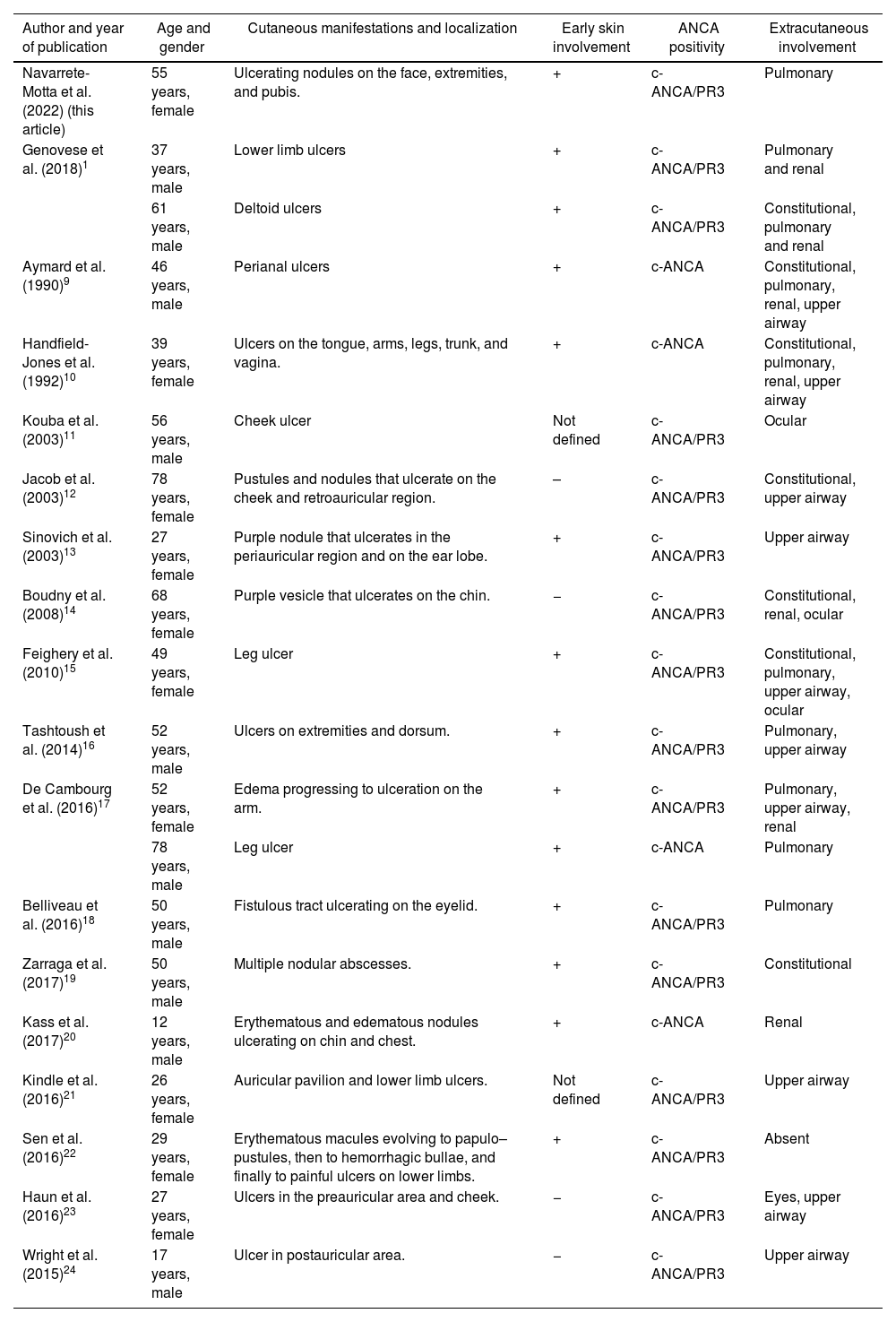
The presence of pyoderma gangrenosum-like lesions in patients with GPA has been reported in up to 10% of patients with cutaneous manifestations of vasculitis, being the fourth most frequent cutaneous manifestation.8 In a case series, 29 patients with ulcerative lesions similar to pyoderma gangrenosum associated with GPA were identified. In most cases, the initial lesions were nodules or pustules that progressed to ulcerative lesions. In all patients in whom ANCA were measured, the result showed anti-PR3 antibodies or a cytoplasmic pattern by immunofluorescence, as did our patient. Table 1 summarizes the cases reported to date of GPA with ANCA positivity associated with pyoderma gangrenosum-like lesions. Cutaneous involvement is usually early and extracutaneous manifestations are frequent, at the expense of constitutional symptoms and pulmonary involvement mainly.
Reported cases of GPA with ANCA and pyoderma gangrenosum-like lesions.
| Author and year of publication | Age and gender | Cutaneous manifestations and localization | Early skin involvement | ANCA positivity | Extracutaneous involvement |
|---|---|---|---|---|---|
| Navarrete-Motta et al. (2022) (this article) | 55 years, female | Ulcerating nodules on the face, extremities, and pubis. | + | c-ANCA/PR3 | Pulmonary |
| Genovese et al. (2018)1 | 37 years, male | Lower limb ulcers | + | c-ANCA/PR3 | Pulmonary and renal |
| 61 years, male | Deltoid ulcers | + | c-ANCA/PR3 | Constitutional, pulmonary and renal | |
| Aymard et al. (1990)9 | 46 years, male | Perianal ulcers | + | c-ANCA | Constitutional, pulmonary, renal, upper airway |
| Handfield-Jones et al. (1992)10 | 39 years, female | Ulcers on the tongue, arms, legs, trunk, and vagina. | + | c-ANCA | Constitutional, pulmonary, renal, upper airway |
| Kouba et al. (2003)11 | 56 years, male | Cheek ulcer | Not defined | c-ANCA/PR3 | Ocular |
| Jacob et al. (2003)12 | 78 years, female | Pustules and nodules that ulcerate on the cheek and retroauricular region. | – | c-ANCA/PR3 | Constitutional, upper airway |
| Sinovich et al. (2003)13 | 27 years, female | Purple nodule that ulcerates in the periauricular region and on the ear lobe. | + | c-ANCA/PR3 | Upper airway |
| Boudny et al. (2008)14 | 68 years, female | Purple vesicle that ulcerates on the chin. | − | c-ANCA/PR3 | Constitutional, renal, ocular |
| Feighery et al. (2010)15 | 49 years, female | Leg ulcer | + | c-ANCA/PR3 | Constitutional, pulmonary, upper airway, ocular |
| Tashtoush et al. (2014)16 | 52 years, male | Ulcers on extremities and dorsum. | + | c-ANCA/PR3 | Pulmonary, upper airway |
| De Cambourg et al. (2016)17 | 52 years, female | Edema progressing to ulceration on the arm. | + | c-ANCA/PR3 | Pulmonary, upper airway, renal |
| 78 years, male | Leg ulcer | + | c-ANCA | Pulmonary | |
| Belliveau et al. (2016)18 | 50 years, male | Fistulous tract ulcerating on the eyelid. | + | c-ANCA/PR3 | Pulmonary |
| Zarraga et al. (2017)19 | 50 years, male | Multiple nodular abscesses. | + | c-ANCA/PR3 | Constitutional |
| Kass et al. (2017)20 | 12 years, male | Erythematous and edematous nodules ulcerating on chin and chest. | + | c-ANCA | Renal |
| Kindle et al. (2016)21 | 26 years, female | Auricular pavilion and lower limb ulcers. | Not defined | c-ANCA/PR3 | Upper airway |
| Sen et al. (2016)22 | 29 years, female | Erythematous macules evolving to papulo–pustules, then to hemorrhagic bullae, and finally to painful ulcers on lower limbs. | + | c-ANCA/PR3 | Absent |
| Haun et al. (2016)23 | 27 years, female | Ulcers in the preauricular area and cheek. | − | c-ANCA/PR3 | Eyes, upper airway |
| Wright et al. (2015)24 | 17 years, male | Ulcer in postauricular area. | − | c-ANCA/PR3 | Upper airway |
The diagnosis of vasculitis can be a real challenge for the clinician. In the correct clinical context, the presence of skin lesions should be an alarm signal to look for concomitant systemic diseases. In these cases, systemic involvement, serological studies, and the type of inflammation documented on histopathology allow differentiation between the two entities. Likewise, multidisciplinary management is essential to carry out an adequate treatment that allows success with fewer sequelae, as occurred in this patient.
Ethical considerationsThe images and clinical data published have the written consent signed by the patient, which is in the possession of the authors. The authors declare that this article does not contain personal information that could identify the patients. In addition, the writing and the working images were approved by the institutional ethics committee.
FundingThe authors declare that they have not received funding for conducting this work.
Conflict of interestsThe authors declare that they have no conflict of interest in this work.