Pycnodysostosis is a rare autosomal recessive disease caused by a mutation in the cathepsin K enzyme gene, a protease that is expressed primarily in osteoclasts and is responsible for bone matrix degradation. The presentation is usually accompanied by short stature, osteoesclerosis, craniofacial dysmorphia and bone fragility. Some papers provide surgical options for fractures of long bones in this type of patients, but none are presented in European Caucasian patients. The case presented is of a Spanish Caucasian European male with bilateral femoral fracture treated by endomedular nailing.
La picnodisostosis es una rara enfermedad autosómica recesiva causada por una mutación en el gen de la enzima catepsina K, una proteasa que se expresa fundamentalmente en los osteoclastos y que es responsable de la degradación de la matriz ósea. La presentación suele ir acompañada de talla baja, osteoesclerosis, dismorfia craniofacial y fragilidad ósea. Algunos artículos aportan las opciones quirúrgicas para fracturas de huesos largos en este tipo de pacientes pero ninguno se presenta en pacientes de raza caucásica europea. El caso que presentamos es el de un varón español de raza caucásica europea con fractura bilateral de fémur tratada mediante enclavado endomedular.
Pycnodisostosis is a rare autosomal recessive disease caused by a mutation in the cathepsin K enzyme gene,1 a protease that is expressed primarily in osteoclasts and is responsible for bone matrix degradation. The presentation is usually accompanied by short stature osteosclerosis, craniofacial dysmorphia and bone fragility.2 Some papers provide surgical options for fractures of long bones in this type of patients but none are presented in the literature of our environment.3–5 The case presented is of a middle-aged male with bilateral femoral fracture treated by intramedullary nailing.
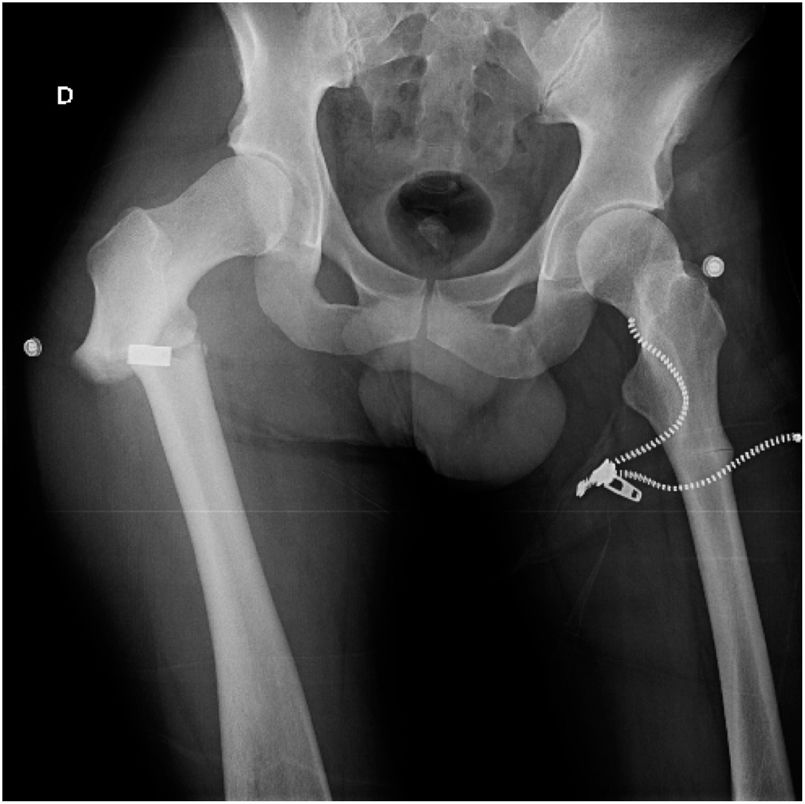
Clinical caseA 38-year-old Caucasian European suffered a fall down a staircase and presented with a subtrochanteric fracture of the right femur with pain and external rotation. On physical examination he presented short statue, small hands and feet and typical facial characteristics. No organomegalia was present nor changes to the blood, as have been described in other cases. The patient had no history of having suffered from any other fracture in the past. Of note is the fact that his brother had presented with multiple fractures throughout his life due to the same disease, and genetic diagnosis was therefore available in both patients since childhood, with no need for further testing to be performed. After the radiologic study a displaced subtrochanteric fracture of the right femur was discovered and a coincidental finding of an incomplete subtrochanteric fracture of the left femur which had not led to pain or any other symptoms in that limb (Fig. 1).
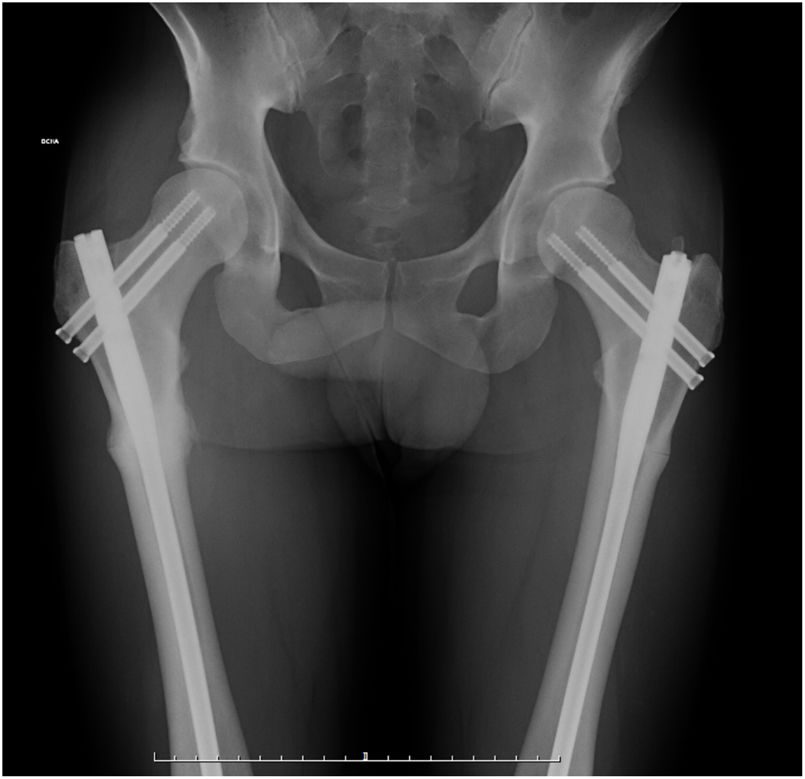
Due to the baseline disease intramedullary nailing was planned initially, in accordance with the literature, bearing in mind the narrowness of the medullary canal and the possibility of having to implant flexible paediatric intramedullary nails as an alternative. Surgery was performed under spinal anaesthesia and beginning with the right femur, which was treated with a 340 × 9 mm Recon nail (Stryker, Portage, Minnesota, U.S.A.), two 85 mm cephalic nails and a 65 mm distal static nail. The left femur was synthesized during the same operation with another 340 × 9 mm recon nail (Stryker, Portage, Minnesota, U.S.A.) and two 80 and 90 mm cephalic nails; in this case no distal nail was used. It is very important to point out that the reaming of both medullary canals was extremely difficult due to the bone hardness, with one of the drills even breaking. No other immediate complications arose nor was there any need for transfusion.
The day after the intervention the patient was able to walk with the help of two crutches. Six months after the accident the patient has returned to work with no complications. The right femur was completely cured whilst the left remained without complete consolidation in some points. One year after the accident total recovery of both fractures was observed and the patient lived a completely normal life (Fig.2). In our case in question there were no complications in either the immediate postoperative period nor subsequently.
DiscussionPycnodisostosis is a rare disease, affecting 0.13/100,000 inhabitants (prevalence of Down’s syndrome is 95/100,000).6 Age range at diagnosis in the literature varied from 9 months to 54 years.1 Most patients had been previously diagnosed with hepatosplenomegalia and/or changes to the blood such as chronic anaemia. The most common complication in this type of patients is delayed bone consolidation. Cases of pseudo osteoarthritis, avascular necrosis, fat embolism and other surgical conditions have also been described.2,7,9
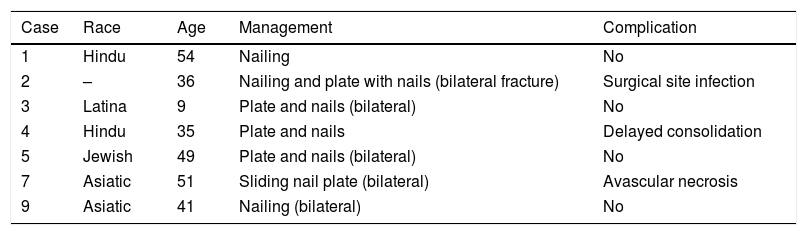
There are other metabolic diseases which can cause atypical femoral fractures, such as imperfect osteogenesis, hypophatasia, X-bound osteoporosis, osteopetrosis, X-linked hypophosphatemia, osteoporosis pseudolioma syndrome.8 Several authors describe the problems they found when inserting an intramedullary nail due to bone sclerosis. Kundu et al.1 reported good results regarding recovery and functionality with the endomedullary nail after two years of follow-up, but found there were similar difficulties to ours with osteosynthesis. Due to these difficulties in 2015 Hasem et al. described a successful case treated with plate and nails in this type of fractures although they assumed it could not be extrapolated to all patients, so they concluded that intramedulallary nailing is the best way to treat this type of fractures in patients with pycnodisostosis.2 Whilst osteopetrosis is associated with a high risk of complications, such as aplastic anaemia or hydrocephalus, patients with pycnodisostosis do not usually undergo these risks. The case presented had a complete clinical recovery eight months after the accident. Although the pycnodisostosis is a very rare disease we should be cautious about it because an atypical femoral fracture pattern in young people should make us suspect a metabolic bone disease. To conclude, in our opinion, in keeping with the literature consulted intramedullary nailing of long bones is a favourable treatment for this type of patients (Table 1).
Summary of cases found in the literature.
| Case | Race | Age | Management | Complication |
|---|---|---|---|---|
| 1 | Hindu | 54 | Nailing | No |
| 2 | – | 36 | Nailing and plate with nails (bilateral fracture) | Surgical site infection |
| 3 | Latina | 9 | Plate and nails (bilateral) | No |
| 4 | Hindu | 35 | Plate and nails | Delayed consolidation |
| 5 | Jewish | 49 | Plate and nails (bilateral) | No |
| 7 | Asiatic | 51 | Sliding nail plate (bilateral) | Avascular necrosis |
| 9 | Asiatic | 41 | Nailing (bilateral) | No |
Please cite this article as: Delgado González A, Morales Viaji JJ, López Díez ME. Fractura bilateral subtrocantérica de fémur debido a una enfermedad rara: la picnodisostosis. Rev Esp Cir Ortop Traumatol. 2021;65:468–470.