To analyse the changes in synovial fluid (SF) in the most common knees joint diseases, and to establish a relationship according to its concentration.
Material and methodsA total of 62 synovial fluids were analysed from knees with, meniscus disease (32), anterior cruciate ligament (ACL) (17) and isolated chondral injury (13). A quantitative and quality study was performed on each sample, which included cytokines IL-1, IL-2, IL-6, IL-10, TNF-α, and growth factors (IGF-1 and TGF-β).
ResultsThe SF environment in the ACL injury was mainly anabolic and inflammatory, with increased levels of IL1, IL6, significant levels of TGF-β (P=.02 and P=.004), IL-10 (P=.046 and P=.047) and significantly decreased levels of TNF-α (P=.02 and P=.004). There was mainly a catabolic environment in chondral and meniscal disease, with a significant increase in TNF-α and a significant decrease in TGF-β (P=.02 and P=.004). The differences were greater in the case of isolated chondral injury.
ConclusionThe changes observed show that, as well as the biomechanical changes, the SF has a negative effect on joint homeostasis, leaving its composition varying depending upon the type of pathology.
Analizar las modificaciones del líquido sinovial (LS) en las afecciones articulares más frecuentes de la rodilla y establecer una relación en función de su concentración.
Material y métodosSe analizaron 62 muestras de LS de rodillas con afección meniscal (32), rotura del ligamento cruzado anterior (LCA) (17) y lesión condral aislada (13). De cada muestra se realizó un estudio cuantitativo y cualitativo de las citocinas (IL-1, IL-2, IL-6, IL-10, TNF-α) y factores de crecimiento (IGF-1, TGF-β).
ResultadosEn la lesión del LCA, el ambiente del LS fue predominantemente anabólico e inflamatorio, con niveles elevados de IL1, IL6, significativos de TGF-β (p=0,02 y p=0,004), IL-10 (p=0,046 y p=0,047) y significativamente disminuidos de TNF-α (p=0,02 y p=0,004). En la afección condral y meniscal, predominó un ambiente catabólico, con elevación significativa del TNF-α y disminución significativa del TGF-β (p=0,02 y p=0,004). Las diferencias fueron mayores en el caso de la lesión condral aislada.
ConclusiónLos cambios observados señalan que en la lesión articular, además de la alteración biomecánica, el LS influye negativamente en la homeostasis articular, variando su composición según el tipo de afección.
Sokoloff1 considered joint cartilage, synovial liquid, synovial membrane and subchondral bone as a functional unit to which other aspects should be added, such as the interchange of oxygen and nutrients and the release of hormones and growth factors. There is growing interest in developing techniques that protect and repair joint cartilage lesions. Epidemiological studies indicate that approximately 6% of adults have a degenerative knee problem, a percentage that increases to 10% for individuals who are older than 65.2
From a biochemical point of view, joint cartilage is a tissue capable of constantly synthesising and degrading the components of the extracellular matrix. The mechanisms of action of growth factors and interleukins (IL) strengthen or inhibit the synthesis of the extracellular matrix components, as well as favouring the action of molecules that degrade cartilage, such as the proteases or their tissue inhibitors.3 The mechanical properties of cartilage vary when alterations in the joint structures occur, such as in anterior cruciate ligament (ACL) section, meniscectomy or tibial plateau resection.4 The synovial liquid (SL) that surrounds the knee joint structures is a dialysed plasma product, secreted by the synovial membrane; under normal conditions, it does not contain coagulation factors, erythrocytes or haemoglobin, but it does present hyaluronate and a lubricating glycoprotein called lubricin, which reduce friction and lubricate the joint.5
With the advances in molecular biology, different patterns for protein and cytokine expression in the SL have gradually been defined and these have been linked with joint degradation. Cytokines are implicated in inflammation and joint damage, which is why their concentration in the SL varies according to the state of the joint. The main intra-articular cytokines involved in joint inflammation are the interleukins (IL)-1, 6 and 8, tumour necrosis factor-α (TNF-α) and granulocyte-macrophage colony stimulating factor (GM-CSF). Likewise, there are other anabolic factors, such as insulin-like growth factor (IGF) and transforming growth factor-β (TGF-β) that are also expressed in the SL and can therefore be analysed. The main effects of growth factors on the chondrocytes are accepted to be stimulating the synthesis of cartilage extracellular matrix and inhibiting protease activation.6
We accept the idea that mediating SL anabolic–catabolic balance changes the environment and the state of the structures that it bathes and we view SL as the natural cartilage lubricant in the diarthrodial joints, which transports the nutritive elements and the joint residues. Based on this idea, we hypothesised that each type of joint disease should modify SL composition in a different way, changing the metabolic balance and provoking a dominance of catabolic factors; the goals of our study were to analyse SL growth factors and SL cytokines in patients with different knee conditions (ACL tear, meniscus lesion or chondropathy) and to establish a relationship according to their concentrations.
Material and methodologyIn a population of patients in a mutual insurance company, after each individual signed an informed consent, we extracted synovial liquid before the knee arthroscopy. All patients were to be operated on for anterior cruciate ligament (ACL) tears, meniscus tears or chondral lesions from tibial plateau fracture, knee osteotomy or joint cleaning.
Table 1 presents the demographic data for the population studied. Knee joint arthrocentesis was performed under sterile conditions, in the operating theatre, with a 10-cm3 syringe. Once the sample was obtained, it was immediately sent to the laboratory, following preservation protocol. To prevent sample handling and contamination, the samples were kept in the same syringes at 4°C, for no more than 72h in the refrigerator.
Population studied.
| Sample | Sex | Age | Condition |
| 1 | Male | 35 | Meniscus |
| 2 | Male | 33 | ACL |
| 3 | Male | 51 | Meniscus |
| 4 | Male | 40 | Meniscus |
| 5 | Male | 48 | Meniscus |
| 6 | Male | 53 | Meniscus |
| 7 | Male | 54 | Meniscus |
| 8 | Male | 45 | Meniscus |
| 9 | Male | 33 | ACL |
| 10 | Male | 33 | ACL |
| 11 | Male | 54 | Meniscus |
| 12 | Male | 34 | ACL |
| 13 | Male | 40 | Chondral |
| 14 | Male | 39 | Chondral |
| 15 | Male | 31 | Chondral |
| 16 | Male | 44 | Chondral |
| 17 | Male | 54 | Chondral |
| 18 | Male | 45 | Meniscus |
| 19 | Female | 58 | Meniscus |
| 20 | Male | 62 | Meniscus |
| 21 | Female | 58 | Meniscus |
| 22 | Male | 51 | Meniscus |
| 23 | Male | 32 | ACL |
| 24 | Male | 51 | Meniscus |
| 25 | Male | 47 | Chondral |
| 26 | Male | 59 | Chondral |
| 27 | Male | 38 | ACL |
| 28 | Male | 39 | Chondral |
| 29 | Male | 51 | Chondral |
| 30 | Male | 58 | Meniscus |
| 31 | Male | 31 | ACL |
| 32 | Male | 60 | Meniscus |
| 33 | Male | 40 | Meniscus |
| 34 | Male | 52 | Meniscus |
| 35 | Female | 30 | ACL |
| 36 | Male | 39 | ACL |
| 37 | Male | 46 | ACL |
| 38 | Male | 36 | Meniscus |
| 39 | Male | 54 | Chondral |
| 40 | Male | 33 | ACL |
| 41 | Male | 43 | Chondral |
| 42 | Male | 39 | ACL |
| 43 | Male | 38 | Meniscus |
| 44 | Male | 40 | Chondral |
| 45 | Male | 43 | Meniscus |
| 46 | Male | 39 | ACL |
| 47 | Male | 38 | Meniscus |
| 48 | Female | 41 | Meniscus |
| 49 | Male | 40 | Meniscus |
| 50 | Male | 30 | Meniscus |
| 51 | Male | 39 | Meniscus |
| 52 | Male | 39 | Meniscus |
| 53 | Male | 45 | ACL |
| 54 | Male | 47 | Meniscus |
| 55 | Male | 61 | Meniscus |
| 56 | Male | 27 | Meniscus |
| 57 | Male | 19 | ACL |
| 58 | Male | 37 | Chondral |
| 59 | Male | 43 | Meniscus |
| 60 | Male | 41 | Meniscus |
| 61 | Male | 22 | ACL |
| 62 | Female | 33 | ACL |
ACL: anterior cruciate ligament.
A total of 62 SL samples were obtained. By knee condition, 32 corresponded to meniscal lesion, 17 were from ACL tear and 13 from chondral lesion as the sole diagnosis. The presence of cytokines (IL-1, IL-2, IL-6, IL-10, TNF-α) and growth factors (IGF-1, TGF-β) were analysed in the SL quantitatively and qualitatively.
We excluded from the study the patients who did not sign the informed consent form, who had any combined knee lesion, presented degenerative alterations, had had previous trauma in either of the two lower limbs, presented varus or valgus angles above 10°, or who had received an operation on the contralateral knee, because of the mechanical overload that might be produced on the study knee.
In the stage of SL reading, each sample was concentrated (1:100) in 5-cm3 tubes (Centricon®, Millipore) for the quantitative and qualitative molecule study. We used the enzyme-linked immunosorbent assay (ELISA) technique to analyse the growth factors (IGF-1, TGF-β) and the cytokines (IL-1, IL-2, IL-6, IL-10, TNF-α) present in the samples (BioLegend® antibody detection kit, San Diego, CA, USA). The SL was incubated with the capture antibodies for 16h, following the supplier's indications, to block and detect the unions specified. Wave detection and plate reading were carried out in Tecan® equipment (Sunrisebasic™, Männedorf, Switzerland) at a wavelength of 540nm. The data obtained were analysed statistically with the SPSS 16.0 program. The descriptive data results were obtained and then statistically significant differences (P=.05) were calculated with the Mann–Whitney U-test.
ResultsThe cytokine analyses varied according to the joint condition. IL-1 levels were higher in the ACL and chondral lesions, compared with the meniscal lesion. However, the differences were not statistically significant (P=.799) (P=.11) (P=.78) (Fig. 1).
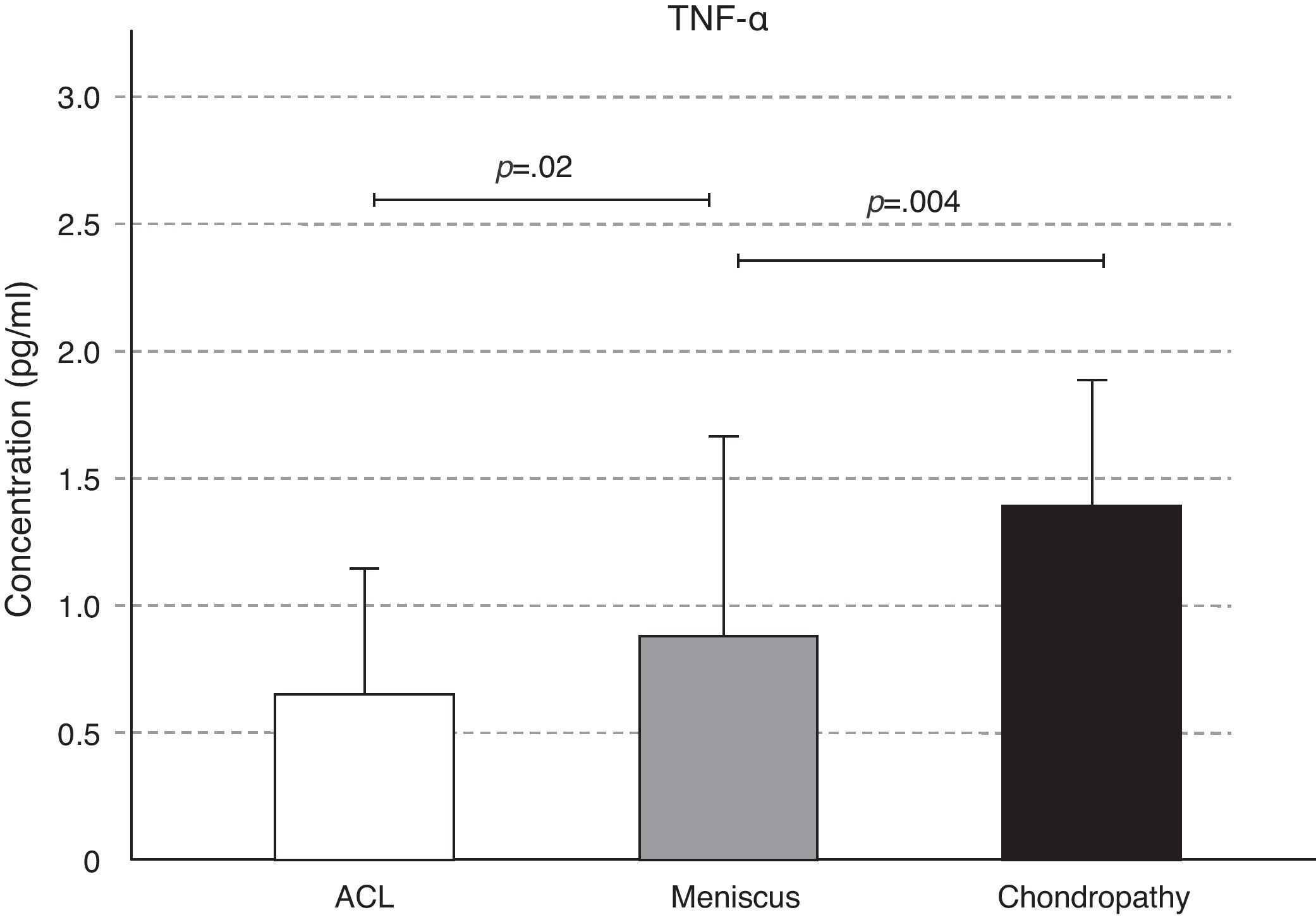
The concentrations of IL-2 and of TNF-α increased in the chondral condition, followed by the meniscal and, lastly, in the ACL lesion; these differences were significant in the case of TNF-α. We observed a significant increase in TNF-α concentration in meniscal lesion SL with respect to that of ACL (P=.02), and of the chondral lesion compared to that of the meniscal (P=.004) (Figs. 2 and 3).
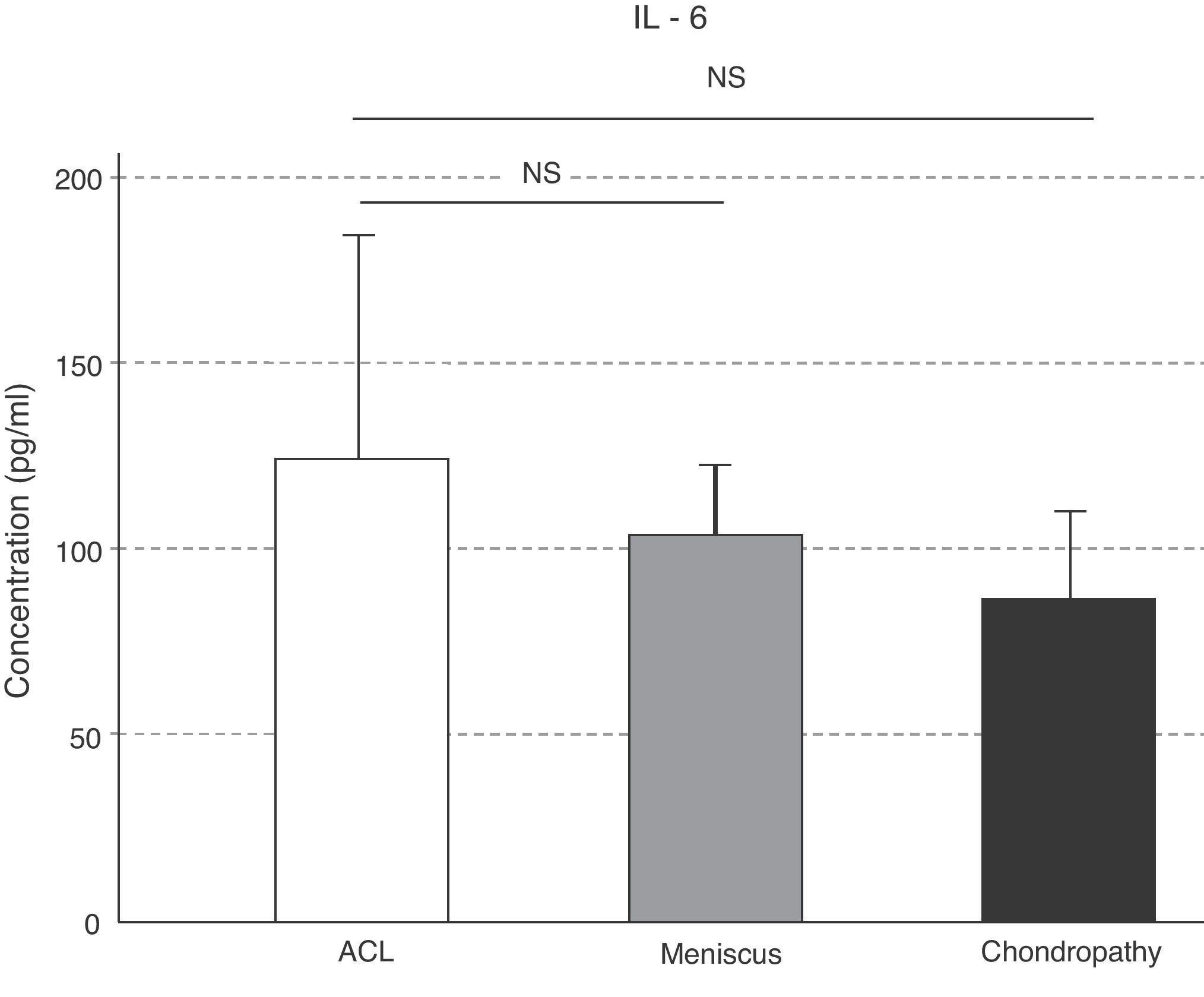
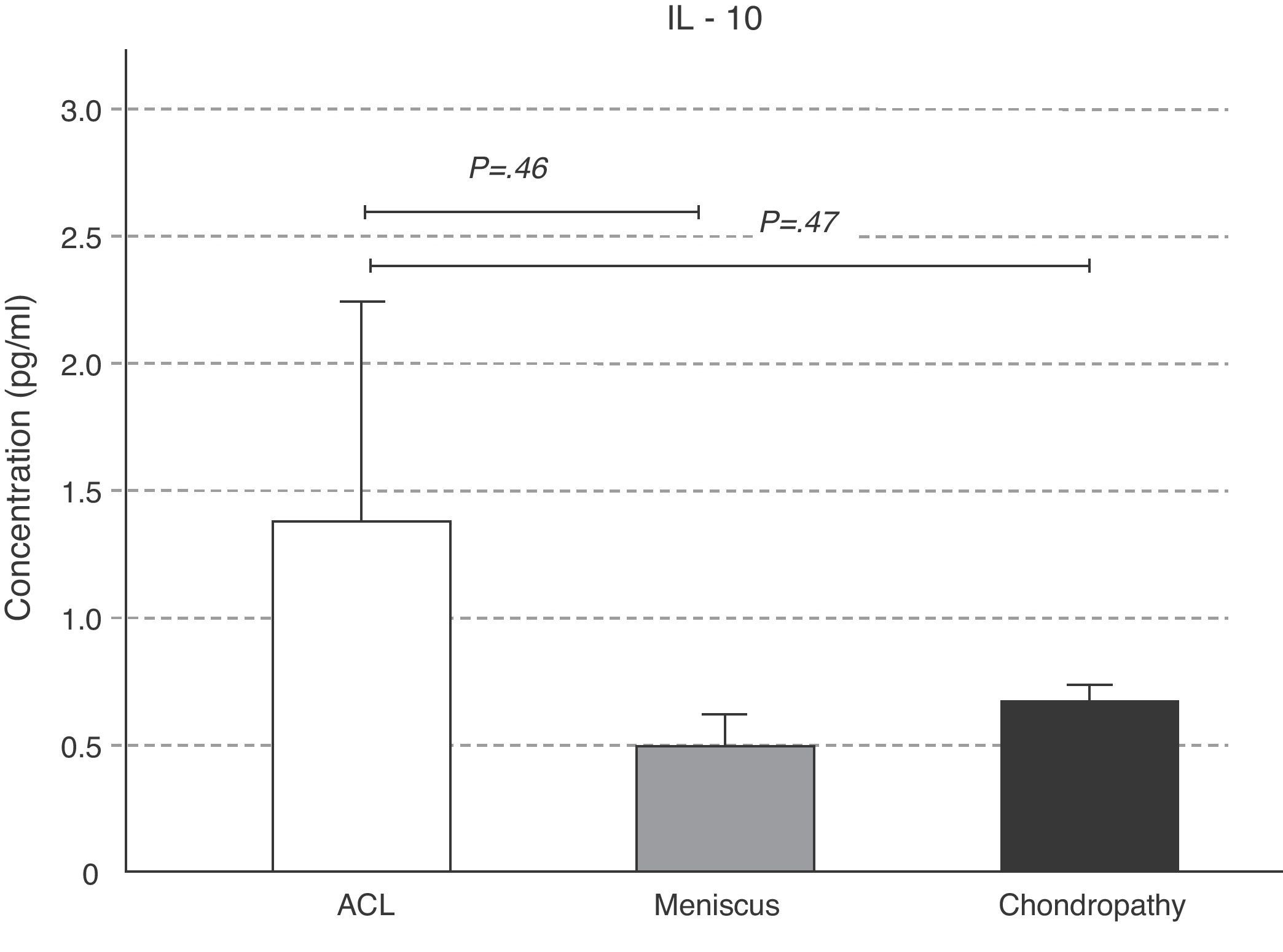
The concentrations of IL-6 behaved like those of IL-10, which were greater in the ACL lesion with respect to the meniscal and chondral conditions; however, these variations were not statistically significant (P>.05) (Fig. 4). The IL-10 levels were significantly greater in the ACL lesion with respect to the meniscal (P=.046) and chondral (P=.047) lesions (Fig. 5).
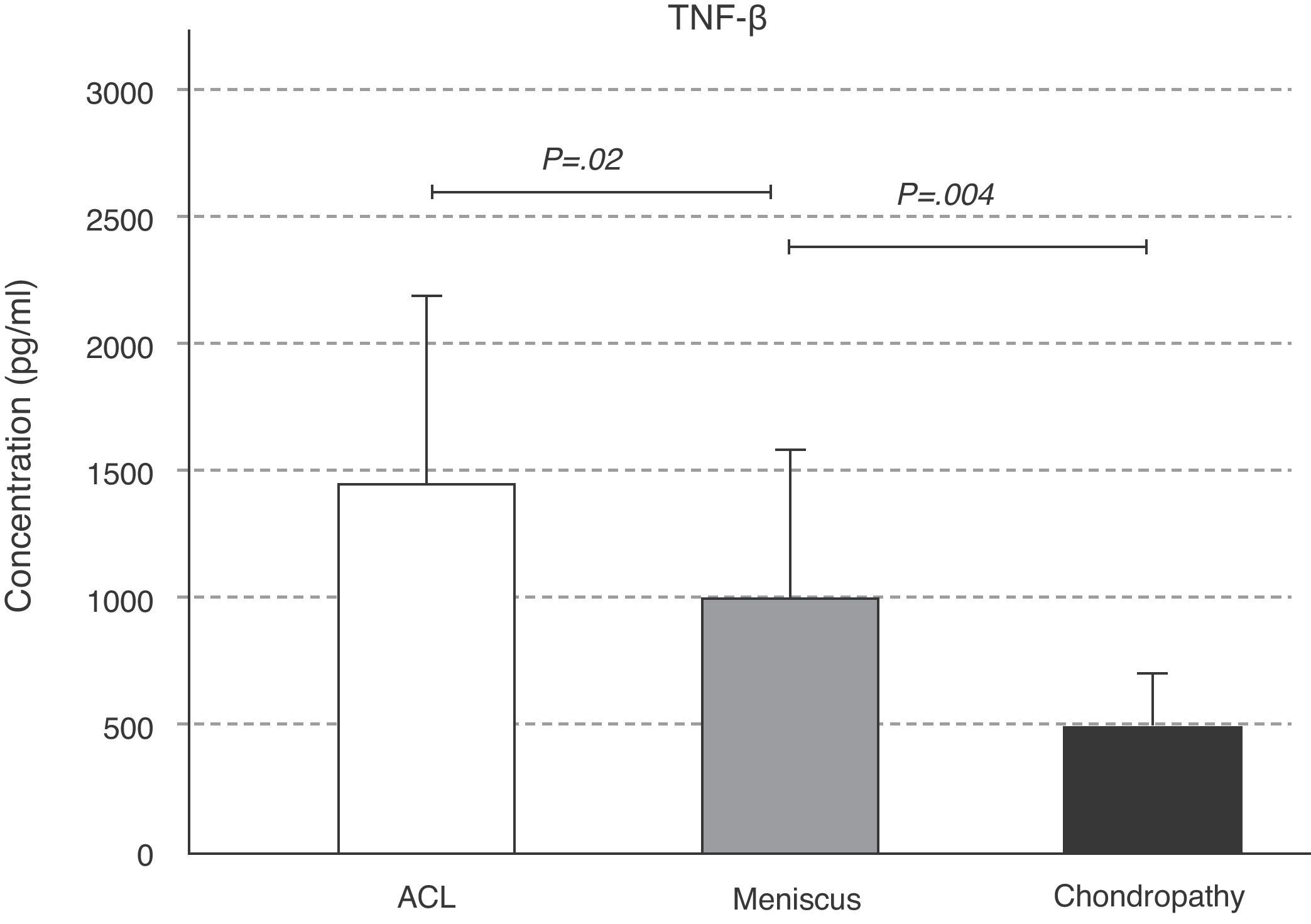
The expression of TGF-β behaved similarly to that of IL-10; a greater amount of TGF-β was found in the ligament condition, followed by that of the meniscal (P=.02) and the chondral (P=.004) conditions (Fig. 6). The slight variation in IGF-1 concentration in the 3 conditions was not significant (Fig. 7).
Consequently, in the ACL condition, the SL microenvironment was principally anabolic and inflammatory, with elevated IL1 and IL6 levels, significant TGF-β and IL-10 levels and significantly decreased TNF-α levels. In the chondral and meniscal conditions, a catabolic environment dominated, one of degeneration; there was a significant TNF-α elevation and significant TGF-β drop. The differences were greater in the case of the isolated chondral lesion.
DiscussionAnalysing synovial liquid has been a procedure for diagnosis of rheumatic conditions. Ropes and Bauer7 detailed the differences in appearance and cell content of pathological SL and related it with different diseases, distinguishing between the inflammatory and non-inflammatory forms of rheumatoid arthritis. Hollander et al.8 set forth the routine use of SL analysis as an aid to diagnosis, documenting the main findings on the liquid in the different forms of arthritis in detail and introducing the term “synovianalysis”. Later on, Shmerling9 classified some diseases with the total and differential white blood cell count. Amiel et al.10 carried out an experimental study on rabbit knees, using a radioactively marked collagen precursor (Proline triad) and found that the nutrient flow, through the synovial liquid, was necessary for the ligaments and menisci. In addition, they found that the amount of nutrients secreted by the SL correlated with the exposition that the ligaments and menisci had to the SL. Based on the idea that the mechanical environment affects development and maturation of the cartilaginous tissue under repair and that the substances secreted by the synoviocytes in the SL affect joint environment (including the cartilage), Vasara et al.11 confirmed the hypothesis that the levels of SL catabolic markers were greater in patients with cartilaginous lesions than in patients with another type of non-cartilaginous knee condition.
It has been shown that, in spite of biomechanical articular repair of the knee,12 evolution toward knee joint degeneration is not prevented. Consequently, the interaction of the anabolic and catabolic SL factors plays a role, in addition to a mechanical cause. Little et al.13 pointed out that the initiation of the focal cartilage degeneration in osteoarthritis was due to regional differences in the response to catabolic cytokines. For their part, Higuchi et al.14 suggested that there had to be a factor added to the biomechanical alteration responsible for the osteoarthritic changes in the knee after the ACL lesion and that the concentration of SL cytokines might be the most important factor in cartilage degradation.
As biomarkers of joint metabolic activity, we focused on IGF-1 and TGF-β, interleukins (IL-1, IL-2, IL-6, IL-10) and TNF-α.
IGF-1 is the principal anabolic factor in SL15 that stimulates the synthesis of proteoglycans, collagen II and integrins, while inhibiting the destruction of the extracellular matrix. In our study, the levels of IGF-1 did not differ significantly according to the type of knee condition. The levels increased slightly in the condition associated with ACL lesions and the chondral condition. In the study by Vasara et al.,11 the IGF-1 levels were also increased in the SL of knees with cartilaginous lesions, in comparison to the control group. This upward regulation of IGF-1 contributes to the production of extracellular matrix and to its remodelling.
It has been shown that TGF-β stimulates the synthesis of proteoglycans in normal cartilage and in human osteoarthritic cartilage culture.16 TGF-β exercises a strong anti-inflammatory action and is involved in the development of fibrosis in chronic inflammation processes. In this study, we found statistical differences with respect to TGF-β levels according to knee condition, with an increase in ACL tears compared to that of meniscus and isolated chondral lesions. This is due to the fact that, in the ACL tear, its vascularisation is affected and, in the cases in which an avulsion is produced, the osseous tissue of the tibial spine is also altered, which provokes bleeding in the joint. Such joint bleeding does not occur in meniscus tears or in superficial chondral lesions. In haemarthrosis, growth factors respond to the type of lesion travel and promote joint repair.
We analysed the interleukins with catabolic action that are the most important or relevant in joint cartilage: IL-1, IL-6 and TNF-α.17 We analysed IL-10 as well, because in the context of inflammation, it regulates the response from the rest of the interleukins.
Produced by the chondrocytes, IL-1 is involved in the destruction of cartilaginous tissue by matrix lysis; it speeds up proteoglycan degradation and reduces the regeneration mechanisms, inhibiting chondrocyte proliferation and proteoglycan synthesis.18 In our study, we confirmed the increase of IL-1 in the 3 pathologies studied, especially in ACL and chondral lesions. As a mediator of inflammation, its levels are elevated in the SL following joint damage. Irie et al.19 indicated this in their study, in which IL-1 concentrations rose in presence of meniscal lesions and with ACL tears.
Overexpression of catabolic factors such as IL-1 and TNF-α seems to affect the aetiopathogenesis of cartilaginous degeneration.20 In general, the levels of inflammatory cytokines increase in osteoarthritic joints.21 This fact was also seen in the study results, with the increase of IL-1 and TNF-α in chondral-type conditions.
IL-2 is needed for establishing cellular immune memory, as well as for recognising foreign autoantigens and antigens. We demonstrated how IL-2 and TNF-α levels followed a similar fluctuation pattern according to the type of joint condition. IL-6, together with IL-1 and TNF-α, are responsible for regulating the acute phase of the inflammatory response.
In the ACL condition, the SL environment was predominantly anabolic and inflammatory, with elevated IL-1 and IL-6 levels and significant levels of TGF-ß (P=.02 and P=.004) and IL-10 (P=.046 and P=.047). Cuellar et al.22 demonstrated that the rise in the cytokines IL-1β, IL-6, TNF-α and monocyte chemotactic protein-1 (MCP-1) correlated positively and in a statistically significant manner with respect to the results of acute knee pain and meniscal lesion, with a sensitivity and specificity of 100%; exceeding the performance of NMR images and comparing it with the standard pattern of intraoperative results. Higuchi et al.14 showed that IL-6 concentration remained high in the SL of the knee with ACL lesion for 50 weeks following the lesion, after which IL-6 concentration dropped.
Tumour necrosis factor-α (TNF-α) and IL-1 are 2 pro-inflammatory cytokines that help to deregulate chondrocyte function and lead to a progressive degradation of the cartilaginous matrix and loss of joint function.23 Although it is true that TNF-α stimulates metalloproteinase (MMP) production and permits cartilage degradation, it is logical to see that we found its greatest concentrations in the chondral lesion, followed by the meniscal (P=.004) and, lastly, the ACL lesion (P=.02).
The expression of SL cytokines and growth factors in the context of ACL lesions represented an inflammatory environment, but one that was anti-catabolic and fibroblast stimulating, as has also been indicated in the literature.19,24,25 Meniscal lesion SL, rich in IL-2 and TNF-α, represented an inflammatory and degenerative joint environment and, lastly, chondral lesion SL showed the greatest concentrations of IL-1, IL-2 and TNF-α and the lowest IL-6 and TGF-β levels. This situation translates to chondrocyte degeneration, loss of collagen fibres and lack of formation stimulus from the fibroblasts. In the chondral lesion, our results were similar to those of Marks and Donaldson,26 who observed that the cytokine profile in the SL of knees with ACL lesions varied according to the degree of cartilage lesion. The increases in the concentration of IL-1β and of TNF-α correlated significantly with the degree of cartilage destruction and with the time elapsed from the initial lesion.26
Consequently, the elevation in cytokines is not the sole cause of joint damage; rather, as has been shown, the cytokines inhibit the synthesis of other proteoglycans, growth factors and collagen II.27 In addition, the alterations in synthesis regulation (anabolic) and reabsorption activity (catabolic) in the synovial liquid provoke deterioration in the structural and functional properties of the cartilage and net loss of cartilaginous matrix components. In fact, there is growing evidence that specific cytokines have a function in joint inflammation and in the physiopathological loss of joint cartilage within the diseased or damaged joints.28
The limitations of this study were those of an experimental in vitro trial, in that we selected the sample used. In vitro techniques make it possible to perform qualitative research under controlled conditions. We chose specific knee conditions so that each sample group would be as homogeneous as possible, and there was no control group because we were not able to obtain informed consent from the patients in the face of performing arthrocentesis in the healthy contralateral knee. With respect to selecting the cytokines studied, we took the biomarkers that have received the most attention in the context of joint inflammation.
Up to now, no study had compared the different joint environments in the most frequent diseases of the knee. In this study, we demonstrated the hypotheses set out and we feel that inflammatory cytokines can be an added risk factor in the development of osteoarthritis and that, in addition, this risk factor varies according to the type of joint lesion.
Future lines of research might focus on the use of growth factors that stimulate formation of hyaline cartilage and the use of genetic therapy as an instrument to neutralise the inhibitors that block inflammatory cytokines (such as IL-1ra), with the final goal of restoring biological joint balance. Homeostatic alteration of synovial liquid is a risk factor added to the functional and biomechanical alterations that the knee suffers when its stabilising structures are altered and is a factor that gets worse with disease evolution.
Level of evidenceLevel of evidence III.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors will declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors must have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank Raúl Esparza and Isabel Zapero for the sample processing.