To identify those clinical characteristic and arthroscopic findings in patients with knee arthrosis that are associated with worsening of the disease and subsequent total knee arthroplasty (TKA).
MethodA retrospective, descriptive study was conducted on 78 consecutive patients (88 knees) who underwent knee arthroscopy for arthrosis. The study included 44 women and 34 men, with a mean age of 58.9 years (range: 37–78 years). After a mean follow-up of 50.4 months (range: 12–96 months), those patients who progressed towards TKA were identified. A logistic regression model was applied to recognize the factors associated with deterioration of the arthrosis, with consequent progression towards a TKA.
ResultsTwenty-four out of the 88 knees progressed towards a TKA (27.3%) within a mean time of 13.5 months after arthroscopy (range: 13–29 months). The clinical characteristics that showed a significant association with poor progression of the arthrosis were: female gender (0.02) and Ahlbäck 2 (P=.04). Arthroscopic finding that proved significant correlation with worsening of the arthrosis towards TKA were: meniscal tears of the posterior horn (P=.02), meniscectomies above 60% (P=.03), and 2nd degree chondral lesions in loading areas of the medial femoral condyle (P=.02).
ConclusionThe variables associated with a greater chance of progressing towards a TKA after a knee arthroscopy due to arthrosis in this study were, female gender, grade 2 radiographic arthrosis, posterior horn meniscal lesions, meniscectomies over 60%, and chondral lesions in loading area of the medial femoral condyle.
Identificar los hallazgos artroscópicos y las características clínicas de los pacientes con artrosis de rodilla sometidos a lavado articular artroscópico, que se correlacionaron con una mala evolución de su enfermedad y su consecuente conversión a artroplastia total de rodilla (ATR).
MétodoEstudio retrospectivo-descriptivo de una serie de 78 pacientes (88 rodillas) sometidos a artroscopia de rodilla por artrosis. Cuarenta y cuatro mujeres y 34 varones, con promedio de edad de 58,9 años (rango: 37-78) en el momento de la artroscopia, ingresaron al estudio. Tras un seguimiento promedio de 50,4 meses (rango: 12-96) se identificaron aquellos pacientes que evolucionaron a una ATR. Para el análisis estadístico se utilizó un modelo de regresión logística para identificar aquellos elementos asociados a la evolución hacía una ATR.
ResultadosEn el seguimiento, a 24 rodillas se les implantó una ATR (27,3%) a los 13,5 meses de promedio (rango:13-29). Las características clínicas de los pacientes que mostraron una asociación estadísticamente significativa hacia una mala evolución fueron: el género femenino (0,02) y clasificación de Ahlbäck 2 (p=0,04). Los hallazgos artroscópicos asociados significativamente a evolución hacia ATR fueron lesiones meniscales mediales y laterales en cuerno posterior (p=0,02), cuando se realizó una meniscectomia mayor o igual a un 60% (p=0,03) y la presencia de lesiones condrales grado 2 en la zona de carga de cóndilo femoral medial (p=0,01).
ConclusiónEn este grupo estudiado, las variables asociadas a una mayor posibilidad de terminar en una ATR tras una artroscopia de lavado articular fueron del género femenino, artrosis radiológica grado 2, lesiones meniscales en cuerno posterior, meniscectomia mayor al 60% y lesiones condrales en cóndilo femoral medial grado 2 en zona de carga.
Knee arthrosis (or osteoarthritis) is a common condition in the population aged over 50 years and is regarded as the second most common cause of disability worldwide, after cardiovascular diseases.1–4
There are various forms of surgical treatment available when medical treatment for knee pain secondary to osteoarthritis fails. These include arthroscopic procedures (joint lavage and cleaning), aligning osteotomies (tibial or femoral) and joint arthroplasties (unicompartmental, patellofemoral and total).4–10
Arthroscopic joint lavage is a minimally invasive technique which, in addition to visualization of the joint, also enables the performance of various therapeutic procedures. Nevertheless, the role of arthroscopy in the treatment of osteoarthritis is controversial due to the different results reported in the literature, which contains a wide variability of outcomes. Thus, there is currently no consensus regarding the benefits offered by this surgical procedure in knee osteoarthritis. This is due, among other variables, to the fact that it does not change the course of the underlying degenerative disease.5–10 Moreover, it is difficult to compare the results published in the literature due to their different study designs (sample size, procedure performed: joint lavage, debridement, chondroplasty) and patient characteristics (age, body mass index [BMI], activity, degree of osteoarthritis, location of lesions).9,10
The aim of this study was to identify the arthroscopic findings and clinical characteristics of patients with knee osteoarthritis, which correlated with a poor outcome of their disease and subsequent conversion to total knee arthroplasty (TKA).
Materials and methodsThis was a retrospective and descriptive study of a consecutive series of 78 patients (88 knees) who underwent knee arthroscopy due to osteoarthritis. The inclusion criteria were: patients with clinical and radiographic diagnosis of knee osteoarthritis of grades I-III in the Ahlbäck classification and a short evolution of symptoms (less than 12 months). The exclusion criteria were: patients with grade IV in the Ahlbäck classification, desaxations in limbs (varus, valgus, antecurvatum, recurvatum), associated ligamentous lesions and inflammatory joint diseases. At the time of the arthroscopy, 44 females and 34 males, with a mean age of 58.9 years (range: 37–78 years), were included in the study.
We evaluated patients retrospectively through their Lysholm score and postoperative subjective score in the IKDC (International Knee Documentation Committee) scale. We classified our Lysholm results into excellent (95–100), good (85–94) and moderate (<84).
From the clinical data of patients we recorded the BMI and the radiographic degree of arthrosis using the Ahlbäck classification.11 Regarding intraoperative findings, we described location, extent and treatment of meniscal lesions, as well as the location, grade and treatment of chondral lesions.
After a mean follow-up period of 50.4 months (range: 12–96 months) we identified those patients whose treatment progressed to TKA.
In the statistical analysis, we used a logistic regression model in order to identify those elements associated with evolution to TKA.
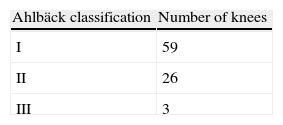
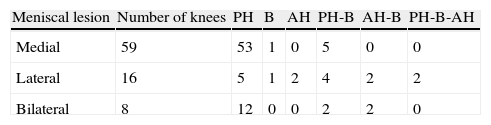
ResultsTable 1 describes the Ahlbäck classification of patients. A total of 83 knees presented meniscal lesions. Table 2 describes the location of meniscal lesions.
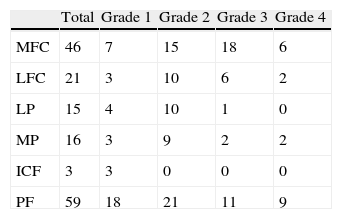
A total of 59 knees presented focal chondral lesions associated to arthritic disease. Table 3 describes the location and extent of these lesions. The mean BMI was 28.3 (range: 24.8–31.3).
Distribution of chondral lesions and their grade.
| Total | Grade 1 | Grade 2 | Grade 3 | Grade 4 | |
| MFC | 46 | 7 | 15 | 18 | 6 |
| LFC | 21 | 3 | 10 | 6 | 2 |
| LP | 15 | 4 | 10 | 1 | 0 |
| MP | 16 | 3 | 9 | 2 | 2 |
| ICF | 3 | 3 | 0 | 0 | 0 |
| PF | 59 | 18 | 21 | 11 | 9 |
ICF: intercondylar fossa; LFC: lateral femoral condyle; LP: lateral plate; MFC: medial femoral condyle; MP: medial plate; PF: patellofemoral.
Out of the total knees, 24 evolved to TKA (27.3%) after a mean period of 13.5 months (range: 13–29 months). The indication to perform prosthetic replacement was the persistence of pain symptoms which caused patients to stop practicing sports and even interfered with activities of daily living.
The median scores obtained postoperatively for patients who did not require TKA were: Lysholm 70 points (IQR [interquartile range]: 40–78 points) and IKDC 68 points (IQR: 60–78 points), whereas the median for patients requiring TKA were: Lysholm 46 points (IQR: 30–56 points) and IKDC 48 points (IQR: 50–58 points). We observed statistical significance between the groups, both for the Lysholm (P=.02) and for the IKDC (P=.03).
The clinical characteristics of patients who showed a statistically significant association towards a poor evolution were female gender (P=.02) and grade II in the Ahlbäck classification (P=.04).
The arthroscopic findings with a significant association with evolution to TKA were medial and lateral meniscal lesions in the posterior horn (P=.02), performing a meniscectomy greater than or equal to 60% (P=.03) and the presence of grade 2 chondral lesions in the load area of the medial femoral condyle (P=.01).
DiscussionIn our study we observed that 27.3% of our patients progressed to TKA after a mean period of 13.5 months following knee arthroscopy. The main indication for conversion to TKA was pain, which was reflected in the functional values presented by patients.
There is currently no consensus regarding the role played by knee arthroscopy in the treatment of osteoarthritis of this joint, and this remains a controversial issue, widely discussed in expert meetings.12,13 Despite numerous studies showing the contribution of knee arthroscopy in patients with osteoarthritis and with a variability of results both in favour and against this treatment, it is difficult to reach a definitive conclusion, since, in general, the study groups tend to be diverse in terms of age, degree of osteoarthritis, associated lesions, etc.10
In a randomized clinical trial of 180 patients with knee osteoarthritis, Mosley et al.10 compared joint lavage versus joint debridement versus placebo and found no statistically significant differences between the groups analyzed. It is worth mentioning that the extensive criticism received by this study included the rating scale employed, which was the Knee Specific Pain Scale, which was not validated until recently, thus providing an interpretation of results that could be different when compared with validated scales in literature. Kirkley et al.14 conducted a randomized clinical trial of 86 patients with knee osteoarthritis, comparing arthroscopic treatment plus medical therapy (drugs and rehabilitation) versus medical treatment alone (drugs including paracetamol, NSAIDs and intraarticular injection of hyaluronic acid, and rehabilitation including physiotherapy). These authors obtained similar results, observing no statistically significant differences between the groups after 2 years of follow-up. The rating scale used by this group was the WOMAC scale. Nevertheless, other studies have reported symptomatic improvement in patients with osteoarthritis undergoing arthroscopy. Edelson et al.7 found decreased pain in 23 patients (29 knees) undergoing short-term joint lavage. In the analysis of their results they used the Special Surgery Knee Score, Knee Society Pain Score and visual analogue scale for pain assessment.
Although the relationship between knee osteoarthritis and arthroscopy has been studied extensively, there has been little emphasis on the reasons behind treatment failure and the main factors related to this negative outcome. After a systematic review of the literature regarding the predictors of progression in knee osteoarthritis, Chapple et al.15 concluded that there are few confirmable variables with a significant association with a worse outcome. In a retrospective study of patients over 65 years undergoing knee arthroscopy, Johanson et al.16 found that 10.2% of patients required a TKA after 1 year of follow-up. In a retrospective study of 73 patients with a mean age of 58 years undergoing knee arthroscopy with Kellgren-Lawrence grade 3 or 4 osteoarthritis, Steadman et al.17 found a 62% rate of conversion to TKA after 4.4 years.
According to our results, the clinical characteristics which showed a statistically significant association with a poor outcome after performing knee arthroscopy were female gender and grade II Ahlbäck classification. The arthroscopic findings significantly associated with progression towards TKA were medial and lateral meniscal lesions in the posterior horn, conducting meniscectomy greater than or equal to 60% and the presence of grade 2 chondral lesions in the load zone of the medial femoral condyle.
The literature is relatively conclusive when reporting that the presence of meniscectomies and chondral injuries are factors which influence the functionality of the joint over time.16–18 In a retrospective study of 156 patients with grade 2 Kellgren-Lawrence medial knee osteoarthritis undergoing knee arthroscopy, Spahn et al.18 evaluated the association of clinical and intraoperative poor prognosis factors. They identified the following factors which had a greater association with osteoarthritis of over 2 years evolution: obesity, smoking, presence of medial tibial osteophytes, joint space less than 5mm, absence of synovitis, crystal deposits and meniscectomy. Compared with our study, these authors found similar results regarding the presence of meniscal lesions and subsequent meniscectomy. In a retrospective study of 116 patients (128 knees) undergoing TKA, Riddle et al.19 found that the factors associated with progression of their condition were a history of previous surgery in the affected knee, the presence of flexion contracture in the knee and pain associated with persistent joint effusion.
While the literature recognizes that patients with knee osteoarthritis who suffer obesity have a more symptomatic or severe osteoarthritis,20–23 the variable of obesity was not associated with a worse prognosis in our study. Sridhar et al.21 suggested that obesity itself is a factor of poor prognosis and that, in addition, it has a direct influence on the functional outcome after conducting TKA.
We believe that the treatment performed was adequate for the group of patients who did not undergo TKA and their postoperative functional scores support this belief. Nevertheless, a comparison with the preoperative period could not be established, since preoperative values were not available.
Among the weaknesses of our study we can include it being a retrospective series and, therefore, not having preoperative functional values. In addition, pain was not analyzed by any scale before performing TKA.
ConclusionIn patients with knee osteoarthritis undergoing arthroscopic joint lavage, the variables associated with a greater chance of progressing to TKA include female gender, grade 2 radiographic osteoarthritis, meniscal lesions in the posterior horn, meniscectomy over 60% and grade 2 chondral lesions in the load zone of the medial femoral condyle.
Level of evidenceLevel of evidence iv.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation adhered to the ethical guidelines of the Committee on Responsible Human Experimentation, as well as the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that this work does not reflect any patient data.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Figueroa D, Calvo R, Villalón I, Tuca MJ, Vaisman A, Valdés M. Factores clínicos y hallazgos en la artroscopia de pacientes con artrosis de rodilla que favorecen la conversión a artroplastia total. Rev Esp Cir Ortop Traumatol. 2013;57:263–7.