To describe the characteristics and evolution of deep surgical site infection following thoracolumbar instrumented spinal surgery (DSITIS) in our centre over a period of ten years.
Material and methodDescriptive retrospective study. Patient data (epidemiological/health status), surgical data, infection characteristics/presentation, isolated microorganisms, required surgical debridements, implant removal and major complications linked to infection were evaluated.
ResultsWe included 110 patients (80 females). Median follow-up after infection diagnosis was 3.6 years. Adolescent idiopathic scoliosis, adult deformity and degenerative lumbar stenosis were the most frequent aetiologies. Sixty-two percent of the patients had at least one clinical feature that made them prone to infection. Infection presentation was early (0–3 months from first surgery) in 60.4% of the cases, delayed (3–24 months) in 11.7%, and late (more than 24months) in 27%. All patients were treated by surgical debridement. Twenty-five percent needed more than one surgical debridement. Implants were removed in 46% of the patients (71% in the first surgical debridement). The most frequent isolated microorganisms were coagulase-negative Staphylococcus, Propionibacterium acnes and Enterococcus. Major complications appeared in 15% of the patients, and 88% of them required major surgeries.
ConclusionsLate DSITIS is more frequent than previously reported. Skin microorganisms predominate among the DSITIS culprits. DSIITS produce a high rate of major complications that usually require major surgery for treatment.
Describir las características y la evolución de la infección profunda en cirugía instrumentada de raquis toracolumbar (IPCITL) en nuestro centro en un periodo de 10años.
Material y métodoEstudio descriptivo retrospectivo. Se analizan datos del paciente (epidemiológicos/salud), datos operatorios, presentación de la infección, gérmenes cultivados, limpiezas quirúrgicas requeridas, extracción de los implantes y complicaciones significativas derivadas de la infección.
ResultadosSe revisan 110 pacientes (80mujeres). El seguimiento medio tras el diagnóstico de infección fue de 3,6años. Etiologías más frecuentes: escoliosis idiopática del adolescente, deformidad del adulto y estenosis lumbar degenerativa. El 62% de pacientes presentaban algún dato clínico que les hacía proclives a la infección. La aparición de la infección fue precoz (0-3meses de la cirugía primaria) en el 60,4% de los casos, retardada (3-24meses) en el 11,7% y tardía (más de 24meses) en el 27%. Todos los pacientes fueron tratados mediante limpieza quirúrgica. El 25% necesitaron más de una limpieza. Se extrajeron los implantes en el 46% de los pacientes (en el 71% de ellos en la primera limpieza). Los gérmenes aislados con mayor frecuencia fueron Staphylococcus coagulasa-negativo, Propionibacterium acnes y Enterococcus. Hubo complicaciones significativas derivadas de la IPCITL en el 15% de casos. El 88% de ellas precisaron cirugías complejas para su tratamiento.
ConclusionesLas IPCITL tardías son más frecuentes de lo esperado según la literatura. En IPCITL globalmente predominan gérmenes cutáneos. Las IPCITL provocan una alta tasa de complicaciones, que habitualmente requieren tratamiento mediante cirugías complejas.
Deep infection in thoracolumbar instrumented spinal surgery (DITLIS) is considered a major complication with long-term morbi-mortality that has not yet been fully defined. Infections cause longer hospital stays, greater economic costs, worse clinical outcomes that significantly alter patients’ quality of life, and, in some series, are associated with mortality rates in excess of 10%.1–3
Treatment objectives for spinal infection3 are to cure the infection and attain a stable, pain-free spine. Treatment strategies to achieve these aims must contemplate the patient's comorbidities, the causal germ, and a combination of medical and surgical treatment.
A distinction is made between two kinds of infections, depending on whether the involvement is above (superficial) or below (deep) the fascia. Deep infections pose the most clinical and therapeutic problems.4,5
At present, there is abundant bibliography that addresses spinal infection, but said literature is heterogeneous.2 Studies typically include few cases, with a short follow-up after diagnosis of the infection, and often both superficial and deep infection coexist, as well as instrumented and non-instrumented surgeries.
The objective of this study is to describe the characteristics and evolution of DITLIS in a single centre over a 10-year period.
Material and methodRetrospective, descriptive study in which a cohort consisting of all the patients who underwent surgery with a diagnosis of deep infection in thoracolumbar instrumented spinal surgery (DITLIS) from January 2006 until December 2015. In all cases, the primary surgery was performed at our hospital. Patients whose primary diagnosis was spondylodiscitis, infections deemed superficial, and infections in which the primary surgery had been performed at another centre were excluded.
The diagnosis of infection was made on the basis of the Infectious Diseases of America (IDSA)6 and/or Centers for Disease Control and Prevention (CDC) criteria7: appearance of purulent fluid in an incision or cavity, presence of fistula, evidence of an abscess on imaging studies or revision surgery, isolation of microorganism in two or more intraoperative cultures, infection according to the surgeon's criterion based on preoperative and intraoperative data (fever, flushing, loosening of instrumentation, etc.). Deep infection is understood as infection underlying the fascia.4,5
The following were evaluated:
- 1)
Epidemiological, clinical, and operative data: age at the time of the primary surgery, gender, anaesthetic risk (ASA), body mass index (BMI), preoperative albumin levels, smoking, modified frailty index (MFI),8 aetiological diagnosis of the primary surgery, surgical approach, fused levels, duration of the primary surgery, and persistent exudate of the surgical wound in the primary surgery. The diagnostic value of the bone scan with gallium-67 was evaluated (when it was available).
- 2)
Presentation of the infection: both the form of presentation (serous/purulent exudate, fistula, local inflammation, fever, abscess, sepsis) as well as the time of appearance with respect to the primary surgery. Following Zimmerli and Ochsner's criteria,9 early infections were defined as those that appeared within the first 3 months of the primary surgery; delayed infections were those that appeared between 3 and 24 months of the primary surgery, and late infections were those that appeared more than 24 months of the primary surgery.
- 3)
The surgical treatment performed, evaluating the number of surgical/debridements required for each patient and whether or not implant extraction was necessary.
Patients with early infection underwent deep debridement, abundant lavage, retention of implants (unless they had clearly loosened), and large-calibre drains were maintained until there was little output. When evolution was not satisfactory (persistence of exudate, fever, etc.), a new cleansing was carried out. In delayed infections, the implant was removed, or not, depending on the existing fusion mass. In late infections in the which it is easier for there to be a good block arthrodesis, the most usual course of action was to remove the implants during the first cleaning.
- 4)
Germs isolated in the samples that were taken during the surgery (at least 3 samples per patient).
- 5)
Significant complications10 (those that altered the expected clinical course with the surgery and had repercussions on the patient's health/life) secondary to the infection, and the treatment surgical that said complications required.
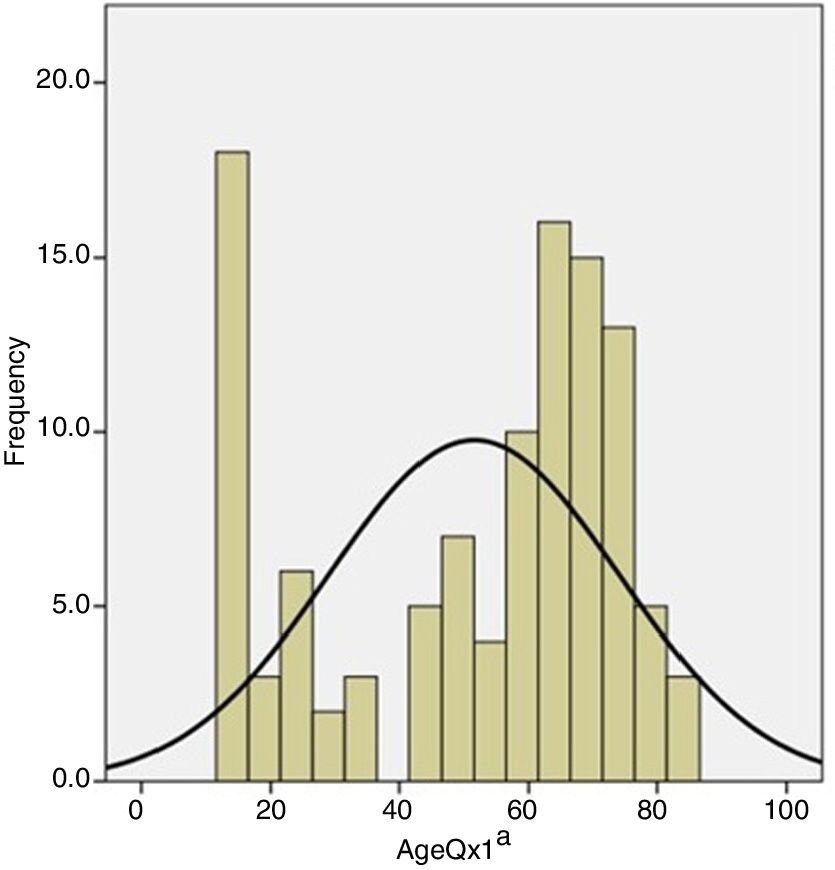
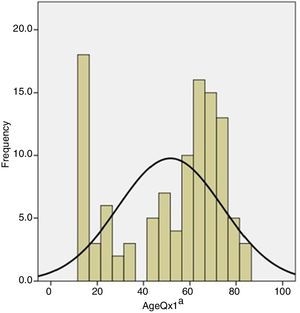
One hundred and ten (110) patients (80 females and 30 males) were evaluated, with a mean age at the time of the primary surgery of 52 years (14–82). More than a quarter (26%) of the individuals were over the age of 70 years at the time of the primary surgery, but the mode of age of the sample was 16 years (Fig. 1).
The mean follow-up following diagnosis of infection was 43.5±31.7 months. The follow-up exceeded 2 years in 68 patients (61.8%), 3 years in 54 patients (49.08%), and more than 5 years in 26 patients (23.63%).
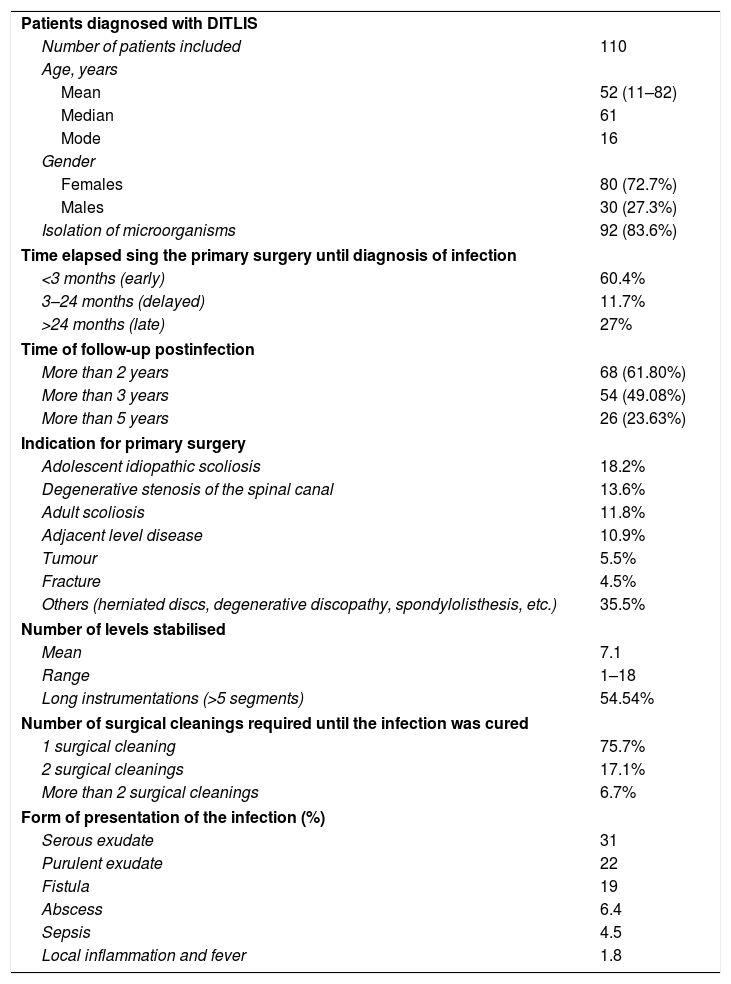
Twenty-one percent (21%) of the patients presented ASA anaesthetic risk I; 47% had an ASA anaesthetic risk II; 30% were classified as ASA III, and 2%, ASA IV. The mean BMI was 28.6 (11.11–45.47); 24.54% of the sample were overweight (BMI between 25 and 30) and 44.54% were obese (BMI >30). Preoperative albumin levels (data were available for 72 patients) were 4.33 (only two patients had albumin levels of less than 3g and the rest were higher). More than one fifth (21%) of the subjects were smokers. The clinical data corresponding to the patients included in this revision are summarised in Table 1.
Clinical data of study sample.
| Patients diagnosed with DITLIS | |
| Number of patients included | 110 |
| Age, years | |
| Mean | 52 (11–82) |
| Median | 61 |
| Mode | 16 |
| Gender | |
| Females | 80 (72.7%) |
| Males | 30 (27.3%) |
| Isolation of microorganisms | 92 (83.6%) |
| Time elapsed sing the primary surgery until diagnosis of infection | |
| <3 months (early) | 60.4% |
| 3–24 months (delayed) | 11.7% |
| >24 months (late) | 27% |
| Time of follow-up postinfection | |
| More than 2 years | 68 (61.80%) |
| More than 3 years | 54 (49.08%) |
| More than 5 years | 26 (23.63%) |
| Indication for primary surgery | |
| Adolescent idiopathic scoliosis | 18.2% |
| Degenerative stenosis of the spinal canal | 13.6% |
| Adult scoliosis | 11.8% |
| Adjacent level disease | 10.9% |
| Tumour | 5.5% |
| Fracture | 4.5% |
| Others (herniated discs, degenerative discopathy, spondylolisthesis, etc.) | 35.5% |
| Number of levels stabilised | |
| Mean | 7.1 |
| Range | 1–18 |
| Long instrumentations (>5 segments) | 54.54% |
| Number of surgical cleanings required until the infection was cured | |
| 1 surgical cleaning | 75.7% |
| 2 surgical cleanings | 17.1% |
| More than 2 surgical cleanings | 6.7% |
| Form of presentation of the infection (%) | |
| Serous exudate | 31 |
| Purulent exudate | 22 |
| Fistula | 19 |
| Abscess | 6.4 |
| Sepsis | 4.5 |
| Local inflammation and fever | 1.8 |
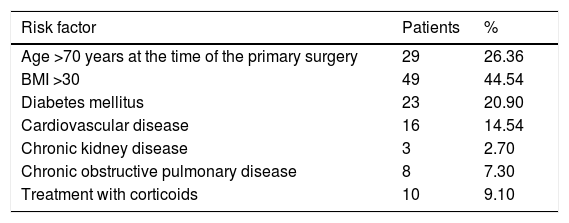
At least one risk factor3 for developing DITLIS was present in 62.72% of the patients (Table 2).
Risk factors for presenting surgical infection following instrumented thoracolumbar spinal surgery.
| Risk factor | Patients | % |
|---|---|---|
| Age >70 years at the time of the primary surgery | 29 | 26.36 |
| BMI >30 | 49 | 44.54 |
| Diabetes mellitus | 23 | 20.90 |
| Cardiovascular disease | 16 | 14.54 |
| Chronic kidney disease | 3 | 2.70 |
| Chronic obstructive pulmonary disease | 8 | 7.30 |
| Treatment with corticoids | 10 | 9.10 |
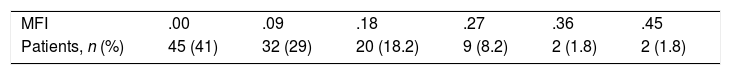
The mean MFI8 score was .1 (.00–.45). In 41% of cases, it was of .00; .09 in 29%; .18 in 18.2%; .27 in 8.2%; .36 in 1.8%, and .45 in 1.8% (Table 3).
The most common aetiological diagnoses were adolescent idiopathic scoliosis (20 cases), degenerative stenosis of the spinal canal (15 cases), adult scoliosis (13 cases), and adjacent level disease (12 cases). Most (90%) of the surgeries were performed using a posterior approach and 10% were performed via a double approach. None of the interventions carried out using an anterior approach became infected. The mean surgical time was 5.5h (1.60–19).
The mean levels fused was 7.1 (1–18). In 60 patients (54.54%), long instrumentations were performed (more than 5 levels), and in 57%, a sacroiliac arthrodesis was performed.
More than half (55%) of the patients who underwent surgery for DITLIS presented persistent (7–15 days) serous/bloody exudate of the surgical wound during admission for the primary surgery.
A preoperative scintigraphy was performed with gallium-67 in 25 patients and was positive for infection in only 11 (40% sensitivity).
Presentation of infectionForm of presentation. More than half (53%) of the infections presented as a serous or purulent exudate; 19% presented in the form of a fistula; 6.4% as an abscess; 4.5% as sepsis, and other presentations (local inflammation, fever, pain) occurred in lower percentages.
Time of presentation with respect to the primary surgery. The infection was acute/early in 67 patients (60.9%), delayed in 13 patients (11.7%), and late in 30 patients (27.2%).
The aetiology of late infection was adolescent idiopathic scoliosis in 14 cases (46.7%), degenerative stenosis of the lumbar spine in 5 (16.7%), neuromuscular scoliosis in 4 (13.33%), and others (adult scoliosis, adjacent level disease, fracture, hyperkyphosis, etc.) in 7 cases (23.33%). The mean time of presentation of late infection with respect to the primary surgery was 32.73 months (25.1–146.2). Of the 30 cases of late infection, 14 (46.67%) presented in the form of a fistula. Late infections presented in younger patients (aged 36 years vs. 60.76 years; p<.000) and with a lower MFI score (.066 vs. .1155; p<.000) than the acute infections.
Surgical treatment of infectionA single surgical cleaning was needed for 76.36% of the patients; 17.27% required two surgeries, and 6.36% needed more than two.
In 51 patients (46%), the implants were removed (in 71% of the cases during the first; in 25.5% during the second, and in 3.9%, during the third surgical cleaning).
Spinal implants were removed in 14 of the 67 patients with early infection; in 10 of the 13 with delayed infection, and in 27 of the 30 with late infection. Thus, there is a statistically significant difference (p<.000) in the percentage of extractions performed in early-delayed-late infections (more in late and delayed infections).
If we exclude the late infections (in which implants are removed at the outset)11 and refer solely to the other two groups (early and delayed), we have seen that the sooner the surgical cleaning is performed, the greater the likelihood is of being able to retain the implants definitively (p<.000). In this way, in the patients in whom the implants ended up having to be removed, 182.1±219.54 days had elapsed between the primary surgery and the first surgical cleaning, whereas in the patients in whom they did not have to be removed, 35.1±58.2 days had transpired.
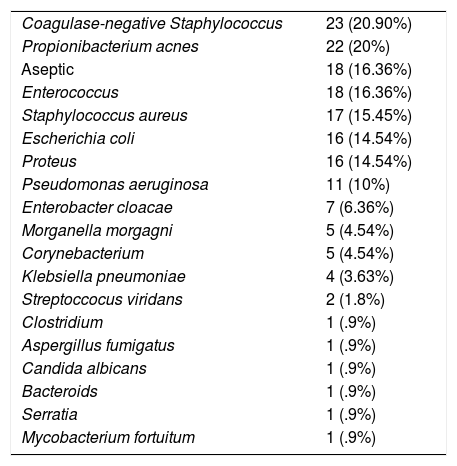
Germs isolatedThe germs most commonly isolated from the intraoperative samples taken during the first surgical cleaning were the usual skin germs (coagulase-negative Staphylococcus in 21% of the patients, Propionibacterium acnes in 20% of the subjects). In 16.3% of the cases, no microorganism was isolated. In the samples obtained during the first surgical surgery cleaning, 13 cases (11.81%) 3 or more germs were isolated. Table 4 is a list of the germs isolated in the first surgical cleaning.
Germs isolated during the first surgical cleaning.
| Coagulase-negative Staphylococcus | 23 (20.90%) |
| Propionibacterium acnes | 22 (20%) |
| Aseptic | 18 (16.36%) |
| Enterococcus | 18 (16.36%) |
| Staphylococcus aureus | 17 (15.45%) |
| Escherichia coli | 16 (14.54%) |
| Proteus | 16 (14.54%) |
| Pseudomonas aeruginosa | 11 (10%) |
| Enterobacter cloacae | 7 (6.36%) |
| Morganella morgagni | 5 (4.54%) |
| Corynebacterium | 5 (4.54%) |
| Klebsiella pneumoniae | 4 (3.63%) |
| Streptoccocus viridans | 2 (1.8%) |
| Clostridium | 1 (.9%) |
| Aspergillus fumigatus | 1 (.9%) |
| Candida albicans | 1 (.9%) |
| Bacteroids | 1 (.9%) |
| Serratia | 1 (.9%) |
| Mycobacterium fortuitum | 1 (.9%) |
In the cases in which a second cleaning was needed (n=26), it was impossible to isolate microorganisms in 11.5% of the individuals. When a germ was cultivate, the most commonly isolated germs were Escherichia coli (8 cases) and Enterococcus (7 cases). In half of the patients in which a second surgical cleaning, the microorganism isolated was the same as the one isolated during the first cleaning, but in the other 50%, new microorganisms were detected that had not grown in the first cultures (“superinfection” detected in 50% of the second cleanings).
Serious secondary complications of the infectionSeventeen study participants (15%) presented complications secondary to the infection during follow-up. Said complications consisted of loss of correction and imbalance in 10 cases, non-union in 6 cases, and one case of sacral pressure sore.
Most of them (88%; 15/17) necessitated complex surgeries (osteotomies, dual approaches, etc.) to treat said. Three patients died due to infection-related causes.
DiscussionThe infection rate in surgery of spine, as well as the risk factors for developing an infection, are amply reported in the literature and are not the aim of the present work. It is well-known that both the incidence and the risk factors vary depending on the series and on how the infection is defined.12
From a descriptive point of view, we have observed that in our series, 44% of the patients were obese; 21% were smokers, and 21% were diabetic. In more than half, long instrumentations had been performed with a mean surgical time of more than 5h. In a systematic review of the literature2 that includes more than 2000 patients, prolonged surgical time, diabetes, smoking, previous existence of infection, surgical aggressiveness, and a high BMI have been identified as risk factors for infection (with strong evidence).13,14
The individual's surgical risk, assessed by means of the ASA and MFI scales, have been associated in the literature2,8,14 with a risk for complications/infection. In our patients, both the ASA, as well as the MFI scores were low. This is likely to be due to the fact that, given that most were elective surgeries with a fair degree of surgical aggressiveness, we do not generally complete them in individuals with a poor clinical situation at baseline.
Old age (more than 70 years) is considered to be a risk factor for infection.2,3 In our series, more than 25% of the patients were older than 70 years of age at the time of the primary surgery. However, we have observed that the mode of age at the time of the primary surgery in our infected patients is 16 years. This fact is undoubtedly related to the high percentage of adolescent idiopathic scoliosis (20 cases out of the total of 110 infections). This is an important point to comment on in this review. In this series, late infection accounts for 27% of the total cases of infections — a figure that is higher than the one published in the literature.3,11,15 Typically, they are patients who undergo surgery for a spinal deformity (mostly adolescents, but also adults) with long instrumentations (they provide a good “breeding ground” for microorganisms) and that have prolonged postoperative follow-ups after the primary surgery. Thus, in follow-ups of the deformity that surpass 2 years, we can find infections that generally manifest as fistulae that are associated with germs of the usual skin flora that cause non-aggressive infections and that can account for more than one fourth of all infections in spinal surgery. The remaining infections (acute and delayed) do correlate with older age and worse preoperative general patient status. We believe that we must be alert to this kind of late infection in deformity, specifically inform the patient of their possibility in patients requiring long instrumentations of spine, and follow-up on these individuals for longer periods of time in order to detect their presence.
The role of prolonged exudate in the surgical wound during the postoperative period following the primary surgery has not been clearly defined in the literature as a possible risk factor for infection, although in it has been indicated as such in some series2 with a low level of evidence. More than half (55%) of our patients presented it. The truth is that the most common presentation of infection in our series has been serous/purulent exudate, and typically in late infections, fistulisation to the skin.
One of the limitations of this study is that its retrospective nature has not made it possible for us to comprehensively collect data regarding the presence of pain as a symptom of infection, but we have the sense that, as reported in the literature,16 persistent, continuous pain in the area of infection that fails to resolve with the use of analgesics is a very common symptom, and that, in the case of late infections, it disappears radically once the instrumentation is removed. We believe that insidious pain should cause us to consider the presence of a possible underlying infection.
In our series, the sensitivity of gallium-67 scintigraphy for the diagnosis of infection was very low. There are reports in the literature16 that point towards a 90% sensitivity of scintigraphy for the diagnosis of bone infection, but the truth is that said literature refers largely to the diagnosis of primary spondylodiscitis and not to the diagnosis of infection in instrumented surgery of spine, and even less, to the diagnosis of late infection provoked by germs with extremely low virulence. F-18 FDG PET/CT is probably more valuable than scintigraphy for diagnosis infection in instrumented spinal surgery.17
We have adopted Zimmerli and Ochsner's classification9 because it is widely acknowledged in prosthetic surgery and because, in the case of spinal surgery, we can consider two years to be a suitable timeframe to think that a good block arthrodesis has been achieved that would enable the instrumentation to be explanted without jeopardising stability. Nonetheless, it is well-known that block grafts are dynamic and, despite seen a good intraoperative posterior graft when extracting the implants, the patient may lose correction18 after removing the instrumentation. In the infections that were not late (prior to 24 months of the primary surgery), we recommend that surgical cleaning be undertaken as early as possible, given that, as in the literature,19 we have observed that the sooner it is performed, the greater the possibility is of being able to conserve the implants, thereby minimising the risk of instability and fostering union. Clearly, whether to remove or exchange the instrumentation or not is a decision that must be made on a case-by-case basis, depending on the block arthrodesis, time of evolution, the detritus found during surgery, and the surgeon's clinical expertise.
Overall, without distinguishing the time of appearance of the infection, we have observed that the germs that were most often isolated in the intraoperative samples were microorganisms of the regular skin flora (coagulase-negative Staphylococcus in 21% of the patients, P. acnes in 20%), although much of the literature points to Staphylococcus aureus as the most common infectious germ.2,3,10
The most recent literature15 corroborates our finding. Insofar as the patients who needed a second surgical cleaning (indicative of poor evolution) are concerned, half of the cases in which different germs grew in the samples taken during this second cleaning compared to the ones cultured in the first cleaning (superinfection); this is an aspect that we have not found in the literature.
There are reports in the literature3,5,20,21 of deep infection in instrumented surgery of spine being associated with more complications, a high percentage of non-union, more revision surgeries, worse quality of life, and has a mortality rate that can surpass 10%. These data are in line with what was seen in our patients; the most serious complications that required more aggressive surgeries occur above all, albeit not exclusively, in adults.
While this revision presents the limitations that are typical of retrospective studies and makes no reference whatsoever to the antibiotherapy used, it has a mean follow-up since the time of diagnosis of prolonged infection, reveals the high percentage of late infections among all the infections, the secondary complications of these infections, and the need for very aggressive revision surgeries. Furthermore, what is most striking is the information about the germs most often cultured (usual flora of the skin) and with respect to the presence of superinfection in the cases of poor evolution following surgical cleaning.
ConclusionsThe number of late infections (as of 2 years) in instrumented surgery of spine accounts for an elevated percentage of all infections. Above all, they occur in long instrumentations in deformities; they most often manifest as a fistula to skin; they arise from germs from the usual skin flora, and the possibility of them developing should be reported to the patient when advising them about the primary surgery, particularly in adolescent idiopathic scoliosis.
In early/delayed infections, surgical cleaning makes it possible to conserve the implants more often when the cleaning is done earlier.
In our series, scintigraphy has exhibited very low sensitivity for diagnosing infection.
Considering the whole of the infections, the regular skin germs are the most common infectious agents.
Infection in thoracolumbar instrumented spinal surgery entails a high percentage of complications, which in almost 90% of cases, require complex revision surgeries.
Level of evidenceLevel of evidence III.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: de la Hera B, Sanchez-Mariscal F, Gomez-Rice A, Ruano Soriano E, Vázquez-Vecilla I, Zúñiga L, et al. Infección quirúrgica profunda en cirugía instrumentada de raquis toracolumbar. Diez años de experiencia. Rev Esp Cir Ortop Traumatol. 2019;63:300–306.