Corticosteroid injection is an effective treatment for trigger digits but the pain during the injection is an ever-present side effect. Since the palmar skin has a high density of sensitive receptors, injecting through dorsal skin could be less painful. Our aim was to assess whether a dorsal technique through the dorsal web is safe for extra-sheath injection of trigger fingers and thumb.
Material and methodThis is an anatomical study in sixteen cadaveric hands. An injection through the dorsal web was performed on each digit. After careful resection of the palmar skin, the distance between the needle and the main anatomical structures was measured. The risk of major injury was considered high when the mean distance from the needle to the neurovascular bundle was below one millimeter.
ResultsThe mean distance from the needle to the neurovascular bundle was 1.77 mm. Two neurovascular injuries in 112 injections were observed, one nerve and one artery. The safest digit was the thumb while the most dangerous was the index finger. At the ring finger, the technique was safer when it was carried out from the dorso-radial.
ConclusionsA subcutaneous injection near the flexor tendon sheath can be carried out through the dorsal web with a low, but present, risk of neurovascular injury. It could be useful for injection in the treatment of trigger finger and trigger thumb but it should be assessed in a clinical study.
La infiltración corticoidea es efectiva en el tratamiento de los dedos en resorte aunque el dolor percibido por el paciente durante la inyección es un efecto secundario siempre presente. La piel dorsal tiene una menor densidad de receptores nociceptivos por lo que la infiltración desde el dorso podría ser menos dolorosa. El objetivo de este trabajo fue evaluar si una técnica de infiltración a través de la piel dorsal es segura en el tratamiento de esta patología.
Material y métodoEstudio anatómico en 16 manos de cadáver. Se realizó una infiltración a través de la piel dorsal de la comisura digital en cada dedo. Se resecó la piel palmar y se midió la distancia entre la aguja y las principales estructuras anatómicas. El riesgo de lesión iatrogénica se consideró alto cuando la distancia media entre la aguja y alguna estructura neurovascular fue inferior a un milímetro.
ResultadosLa distancia media desde la aguja hasta la estructura neurovascular más cercana fue 1,77 milímetros. Se observaron dos lesiones iatrogénicas en 112 inyecciones, un nervio y una arteria. El dedo más seguro fue el pulgar y el menos seguro fue el índice. En el dedo anular, la técnica fue más segura cuando se realizó desde el lado dorso-radial.
ConclusionesLa técnica de infiltración a través de la piel dorsal de la comisura digital puede realizarse con un riesgo de lesión iatrogénica bajo aunque presente. Esta técnica podría utilizarse en el tratamiento del pulgar y de los dedos en resorte aunque esto debe corroborarse en un estudio clínico.
Digital flexor tendon stenosing tenosynovitis, spring finger or trigger finger, is one of the most common causes of pain and disability in the hand, affecting 2.6% of non-diabetic adults and up to 10% of patients with insulin-dependent diabetes mellitus.1,2
The goal of treatment is to restore smooth and painless sliding of the tendons by achieving full range of motion of the affected finger.3 Most trigger fingers can be treated non-surgically by corticosteroid infiltration, with a success rate varying from 45% to 92% according to the number of injections,4–7 and a low complication rate.8
Different techniques have been described for infiltration, but palmar injection over the metacarpal head is the most commonly used.8,9 As an alternative to the palmar technique, a mid-axial injection technique has been published at the level of the proximal phalanx, obtaining similar clinical results.9,10 The main side effect of these techniques is the pain perceived by the patient since palmar skin has a high density of sensory receptors.6,11 On the other hand, a paper has previously been published describing an injection technique into the synovial sheath and through the dorsal skin with similar effectiveness to that described for other techniques.12
Some studies have shown that infiltration deposited outside the synovial sheath, at a subcutaneous level, is as effective as intra-sheath injection and also reduces the risk of tendon damage, and therefore it would not be necessary to locate the infiltration inside the tendon sheath.13,14
This is an anatomical cadaver study to assess whether extra-synovial or subcutaneous injection through the dorsal web is safe in the treatment of trigger thumb and finger. The purpose of the paper was to quantify the risk of injury to a major anatomical structure (nerve or artery) during dorsal infiltration and to establish the safest route (radial or ulnar) for the middle and ring fingers.
Material and methodSixteen cadaverous upper extremities were used, 10 female and 6 male, all white Caucasians. The mean age was 81 years (range, 70–96). The specimens had no history of trauma, surgery, or regional pathology that would affect the results obtained in the study.
One of the investigators performed an infiltration through the dorsal web in each finger using a 2 ml syringe (BD Discardit™ II, Becton Dickinson S.A., Spain) and a 25 G needle (SurGuard2, Terumo®, Terumo Medical Corporation, U.S.A.) as they would in their usual clinical practice. The needle path was fixed using an instantaneous adhesive (La Gotita® 2 ml, Fenedur S.A., Montevideo, Uruguay) to prevent a change in its tract during manipulation of the limb.
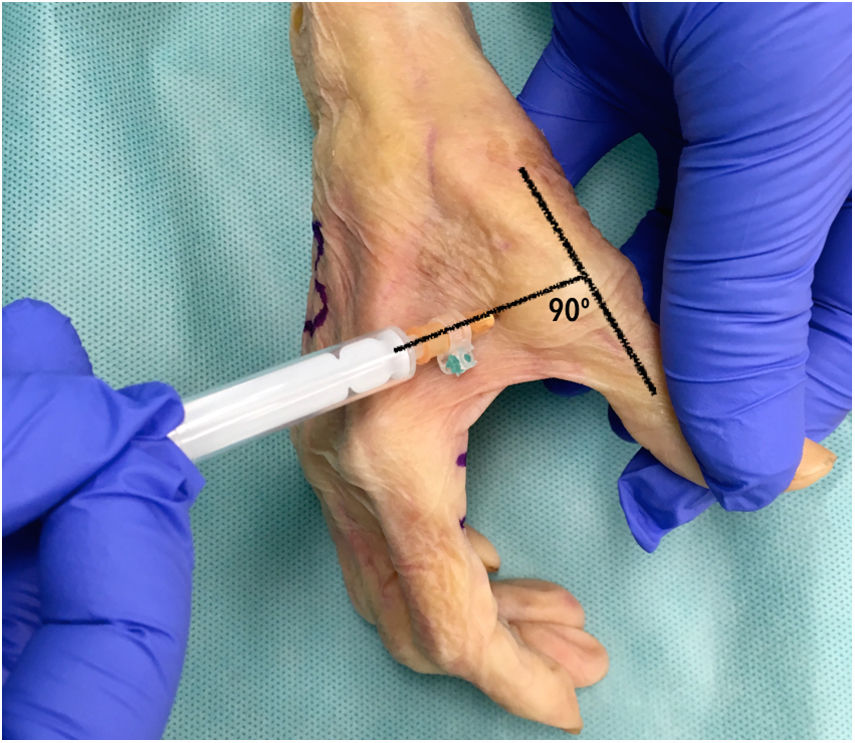
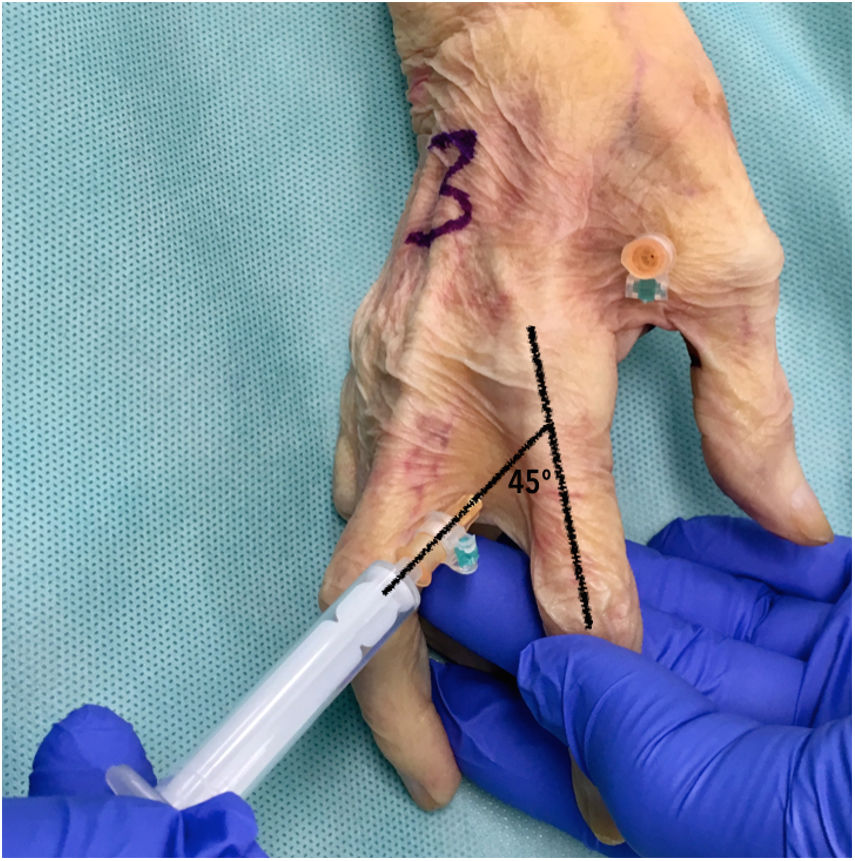
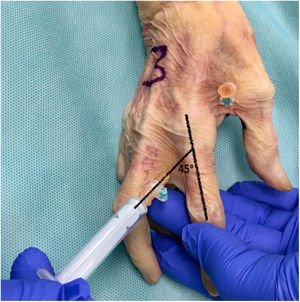
A dorsal ulnar injection was performed in each thumb at the level of the metacarpophalangeal joint keeping the thumb in maximum abduction and directing the needle towards the subcutaneous cellular tissue at the level of the first metacarpal head at a 90° angle to the thumb axis (Fig. 1). For each middle finger, the puncture was performed by keeping the metacarpophalangeal joint slightly flexed (approximately 30°) and directing the needle towards the subcutaneous cell tissue at the head of the metacarpal at a 45° angle to the finger axis (Fig. 2). One ulnar dorsal injection was performed in each index finger, one ulnar dorsal and one radial dorsal injection in each middle and ring finger, and one radial dorsal injection in each little finger.
The technique was not performed from the radial side of the thumb or from the ulnar side of the little finger because it is not a digital commissure. In the case of the index finger, the puncture was not made from the radial side (first commissure) because being a wider and deeper commissure, we considered it would be more difficult for the investigator to orientate the needle during infiltration.
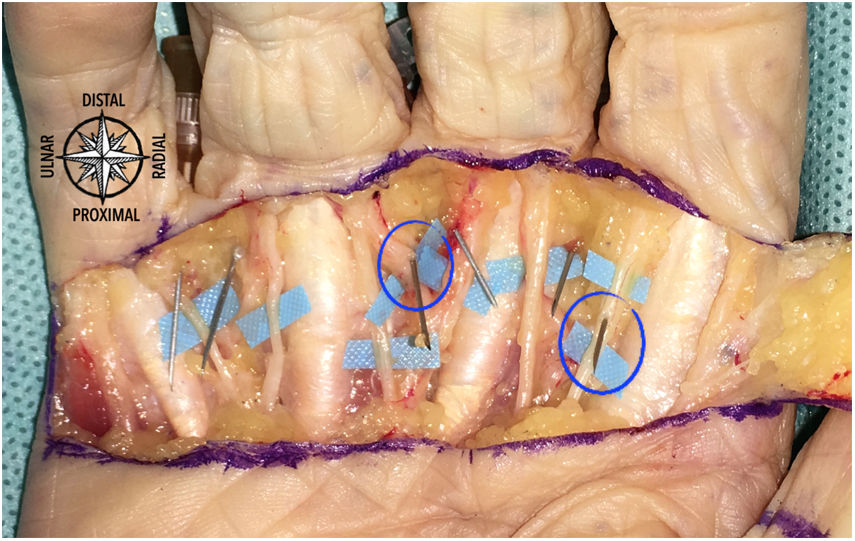
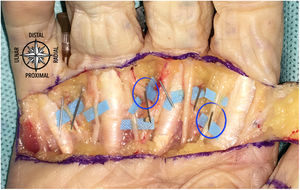
In order to evaluate the exact location of the needle, the palmar skin was carefully resected using 4.5× optical magnifying glasses. In the thumb, a rectangle of skin was resected exposing the entire A1 pulley and the radial and ulnar digital neurovascular bundle. In the middle fingers, a skin area between the mid-palmar crease and the digital palmar crease was resected exposing the A1 pulley and the commissural and digital neurovascular bundle. The resected skin area was arbitrarily selected as it was considered sufficient to expose the anatomical structures at risk but without noticeably modifying the original anatomy.
A major injury was defined as one which, if it occurred in vivo, could have clinical impact such as a nerve or arterial injury. We also recorded other injuries that would have little or no clinical impact if they occurred in vivo, such as puncture of the flexor tendon, pulley or the intrinsic musculature.
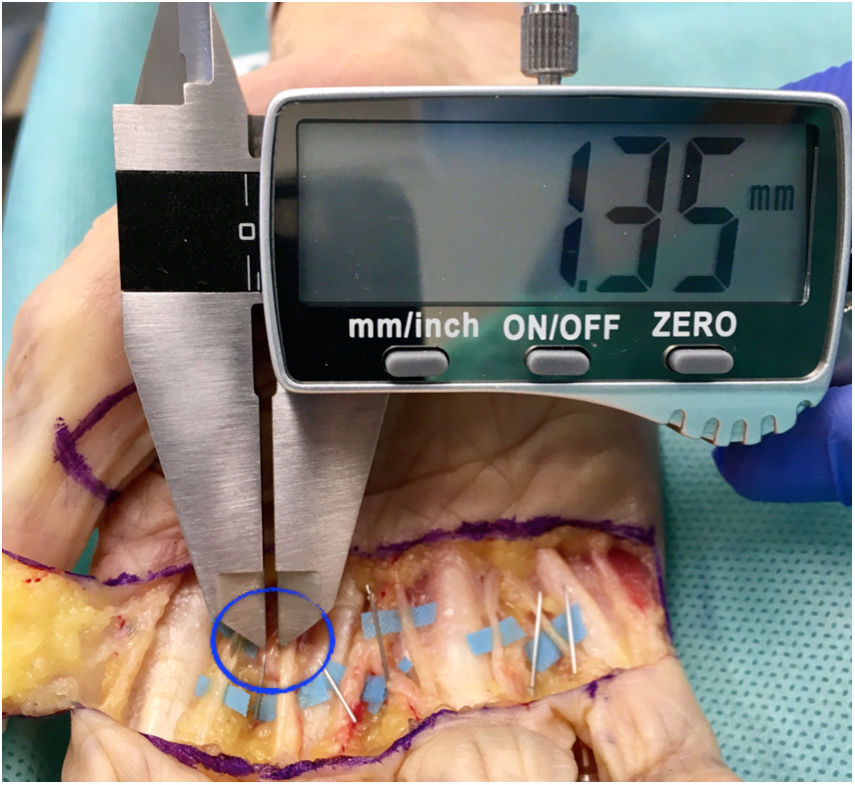
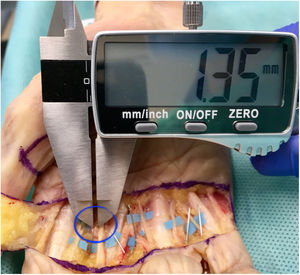
To estimate the risk of injury, the distance between the closest point of the needle to the adjacent anatomical structure was measured in millimetres using a digital calibrator (Tacklife DC02® Mitutoyo, resolution of .01 mm and accuracy of ±.03 mm, Kanagawa, Japan). Two of the investigators measured each infiltration on 3 occasions (Fig. 3).
The Kolmogorov-Smirnov test was used to check the normality of the data. The degree of agreement of the measurements made by each investigator was checked by calculating the intraclass correlation coefficient. The result for the first investigator was .9984 (95% confidence interval [CI95%] .9978–.9989) and for the second investigator .9992 (95% CI .9989–.9995), concluding that intra-observer agreement was excellent.15 The mean of the measurements of each investigator was taken and the degree of inter-observer agreement was assessed using the Lin concordance correlation coefficient, obtaining an excellent degree of agreement (.9991 with 95% CI .9987–.9994), and therefore the mean of the measurements was taken as the final measure in each puncture.
The risk of neurovascular injury was considered high when the mean distance between the needle and any of the neurovascular bundles was less than 1 mm.
All data were analysed using Microsoft Excel 2011 (for Mac, version 14.6.0 2010 © Microsoft Corporation, U.S.A.), StatPlus (for Mac, version V6 2016©, AnalystSoft Inc., U.S.A.) and R Core Team 2019 (version 3.6.2; Bell Laboratories, U.S.A.).
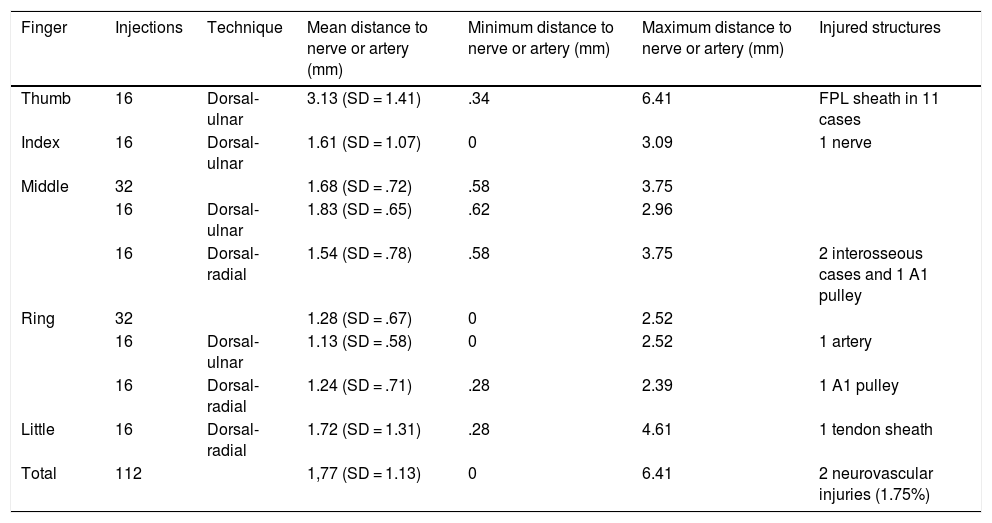
ResultsThe mean distance between the needle and the nearest point of one of the neurovascular bundles was 1.77 mm (95% CI 1.56–1.98). Two injuries were observed in 112 infiltrations (1.78%). In addition, 16 minor injuries were seen (14.28%) (Fig. 4). The results obtained in each finger are shown in Table 1.
- •
Thumb: the mean distance between the needle and the neurovascular bundle was 3.13 mm (95% CI 2.44–3.83). No neurovascular injuries were identified. The flexor pollicis longus sheath was punctured in 11 out of 16 infiltrations (68.7%).
- •
Index: the mean distance between the needle and neurovascular bundle was 1.61 mm (95% CI 1.09–2.13). A neurovascular injury, a digital nerve, occurred (6.25% of the injections). No other injuries were identified.
- •
Middle finger: the mean distance between the needle and neurovascular bundle was 1.68 mm (95%CI 1.43–1.94). The distance from dorsal-ulnar was 1.83 mm (95%CI 1.51–2.15) and from dorsal-radial was 1.54 mm (95% CI 1.16–1.92). No neurovascular injuries were identified. Puncture to the interosseous musculature was identified in 2 cases and to the A1 pulley in one case (9.37% of the infiltrations), all from dorsal-radial.
- •
Ring finger: the mean distance between the needle and neurovascular bundle was 1.28 mm (95% CI 1.05–1.51). The distance from dorsal-ulnar was 1.13 mm (95% CI .83–1.41) and from dorsal-radial was 1.43 mm (95% CI 1.08–1.79). A neurovascular injury was identified, a digital artery from dorsal-ulnar (3.12% of injections). The A1 pulley was also punctured in one case (3.12%).
- •
Little finger: mean distance was 1.72 mm (95% CI 1.08–2.37). No neurovascular injuries were identified. The flexor tendon sheath was injured in one case (6.25% of infiltrations).
Results observed in each finger.
| Finger | Injections | Technique | Mean distance to nerve or artery (mm) | Minimum distance to nerve or artery (mm) | Maximum distance to nerve or artery (mm) | Injured structures |
|---|---|---|---|---|---|---|
| Thumb | 16 | Dorsal-ulnar | 3.13 (SD = 1.41) | .34 | 6.41 | FPL sheath in 11 cases |
| Index | 16 | Dorsal-ulnar | 1.61 (SD = 1.07) | 0 | 3.09 | 1 nerve |
| Middle | 32 | 1.68 (SD = .72) | .58 | 3.75 | ||
| 16 | Dorsal-ulnar | 1.83 (SD = .65) | .62 | 2.96 | ||
| 16 | Dorsal-radial | 1.54 (SD = .78) | .58 | 3.75 | 2 interosseous cases and 1 A1 pulley | |
| Ring | 32 | 1.28 (SD = .67) | 0 | 2.52 | ||
| 16 | Dorsal-ulnar | 1.13 (SD = .58) | 0 | 2.52 | 1 artery | |
| 16 | Dorsal-radial | 1.24 (SD = .71) | .28 | 2.39 | 1 A1 pulley | |
| Little | 16 | Dorsal-radial | 1.72 (SD = 1.31) | .28 | 4.61 | 1 tendon sheath |
| Total | 112 | 1,77 (SD = 1.13) | 0 | 6.41 | 2 neurovascular injuries (1.75%) |
SD: standard deviation; FPL: flexor pollicis longus.
According to the results obtained, the average distance between the closest neurovascular bundle and the needle was more than 1 mm in all the fingers. The digit where the infiltration was most safe was the thumb with a mean distance of more than 3 mm, while the injection was less safe in the ring finger with a mean distance between the needle and neurovascular bundle of 1.28 mm.
Two injuries were observed in 112 injections, one in the index finger (digital nerve) and one in the ring finger (digital artery), both in the same hand of the same specimen. We believe that feedback with the patient during infiltration in clinical practice could help to prevent these injuries, as the patient may feel discomfort when the needle is near the neurovascular bundle and this would allow us to slightly modify the needle tract. This should be evaluated in a clinical research study.
In the middle finger, the 3 minor injuries occurred when infiltration was performed from dorsal-radial, and therefore we could recommend the dorsal-ulnar injection technique for this finger. In the ring finger, an artery was injured during an infiltration from dorsal-ulnar, and therefore we could recommend the dorsal-radial injection technique for this finger.
Corticosteroid infiltration is an effective and efficient treatment for flexor tendon stenosing tenosynovitis,4,8,16 but pain during injection is an ever-present side effect.
Ten percent of patients are very afraid of infiltration, and needle phobia, characterised by an intense and persistent fear of injections, affects approximately 2% of the general population.17 Anaesthetic creams, cooling sprays, lidocaine spray, or verbal distraction have been used to reduce the pain and anxiety associated with infiltrations. Vibratory stimulation concomitant with the puncture has also recently proved ineffective in reducing the pain associated with trigger finger infiltrations.18,19
According to several authors, palmar skin has a greater density of sensory receptors than dorsal skin, making it more sensitive to infiltration through it.6,9,11,20,21 The visual analogue pain score (0–100) during infiltration of a trigger finger through volar skin is 53 points, although there are few studies published in the literature.9,17,18,22
This statement has recently been questioned in some studies publishing that the pain perceived when performing a digital anaesthetic block through palmar skin is no greater than through dorsal skin. There is no consensus on the optimal technique.23,24
Some studies have shown that corticoid infiltration into the synovial sheath of the flexor tendons is not necessary, with similar results obtained with subcutaneous injection performed using the palmar technique.13,14 We believe that an infiltration deposited outside the tendon sheath and performed through the dorsal web could be an equally effective but less painful alternative to classic palmar infiltration in the treatment of flexor tendon stenosing tenosynovitis, although this should be evaluated in a clinical study.
This study has some limitations. The number of specimens was relatively low and, being an anatomical study, it has the usual limitations of this type of study. The sample has low variability (all the specimens were elderly and all were white) and, depending on the preservation and age of the specimen, the extremities could have had some anatomical abnormality such as atrophy of the intrinsic musculature.
A single investigator carried out all the infiltrations while two different investigators, belonging to the same team, carried out the measurements. Despite checking the adequate intra- and interobserver agreement of the different measurements, this aspect could be perceived as a bias.
It would be advisable to replicate the study in different populations (countries, continents, ethnic groups) in order to check whether or not similar results are obtained in terms of measurements and thus assess their external validity.
Based on the results obtained, we consider that subcutaneous corticoid infiltration near the flexor tendon sheath using a technique through the dorsal skin can be performed with a low but present risk of neurovascular injury. This technique could be used in the treatment of trigger thumb and finger, although this must be corroborated in a clinical study.
Level of evidenceLevel of evidence V.
FundingThis research study was funded by the Foundation of the Medical Association of Las Palmas (Grant: XXIV Edition R+E Grants - 2019).
Conflict of interestsThe authors have no conflict of interests to declare.
To the Research Unit of the Complejo Hospitalario Universitario Insular - Materno Infantil de Gran Canaria for their collaboration in the statistical analysis of the study.
Please cite this article as: Jiménez I, Garcés GL, Caballero-Martel J, Medina J. Infiltración comisural dorsal en el tratamiento del pulgar y los dedos en resorte. Estudio anatómico. Rev Esp Cir Ortop Traumatol. 2020. https://doi.org/10.1016/j.recot.2020.02.002