Lumbar disc hernias are a common cause of spinal surgery. Hernia recurrence is a prevalent complication.
ObjectiveTo analyse the risk factors associated with hernia recurrence in patients undergoing surgery in our institution.
Materials and methodsLumbar microdiscectomies between 2010 and 2014 were analysed, patients with previous surgeries, extraforaminales and foraminal hernias were excluded. Patients with recurrent hernia were the case group and those who showed no recurrence were the control group.
Results177 patients with lumbar microdiscectomy, of whom 30 experienced recurrence (16%), and of these 27 were reoperated. Among the risk factors associated with recurrence, we observed a higher rate of disc height, higher percentage of spinal canal occupied by the hernia and presence of degenerative facet joint changes; we observed no differences in sex, body mass index or age.
DiscussionPrevious studies show increased disc height and young patients as possible factors associated with recurrence.
ConclusionIn our series we found that the higher rate of disc height, the percentage of spinal canal occupied by the hernia and degenerative facet joint changes were associated with hernia recurrence.
Las hernias de disco lumbares son una causa frecuente de cirugía lumbar. La recurrencia herniaria es una complicación prevalente.
ObjetivoAnalizar los factores de riesgo asociados a recurrencia herniaria en pacientes intervenidos por hernia discal lumbar en nuestra institución.
Materiales y métodosSe analizaron en forma retrospectiva una serie de 177 microdiscectomías lumbares entre 2010 y 2014; se excluyeron pacientes con cirugías previas, hernias foraminales y extraforaminales. Los pacientes con recurrencia herniaria constituyeron el grupo de casos y los que no presentaron recurrencia fueron el grupo control; se analizó: sexo, edad, índice de masa corporal, nivel, degeneración facetaria, altura discal y protrusión discal.
ResultadosHubo 177 pacientes con microdiscectomía lumbar, de los cuales 30 (16%) presentaron recurrencia herniaria; de ellos, 27 fueron reoperados. Entre los factores de riesgo asociados a recurrencia observamos mayor índice de altura discal, mayor porcentaje de canal ocupado por la hernia y mayor presencia de cambios degenerativos facetarios; no observamos diferencias en cuanto al sexo, índice de masa corporal y edad.
DiscusiónEstudios previos muestran el aumento de altura discal y pacientes jóvenes como posibles factores asociados a recidiva.
ConclusiónEn nuestra serie encontramos que el mayor índice de altura discal, el porcentaje de canal ocupado por la hernia y los cambios degenerativos facetarios se asociaron a recurrencia herniaria.
Lumbar disc hernia is a common spinal pathology, and is the main cause of spinal surgery.1 It is more prevalent in men than in women (2:1 ratio) between the ages of 30 and 50, with the levels most frequently affected being L4-L5 and L5-S1. Its physiopathology is unknown but it is known that intrinsic factors present (hereditary, developmental and degenerative) as do extrinsic factors (nutrition, pressure, trauma, etc.).2
Lumbar microdisectomy continues to be one of the most commonly used surgical procedure in U.S.A., with a good outcome rate in 90–95%.3,4
Among the most prevalent complications (5–-15%)6–8 are the recurrence of the discal hernia (defined as new herniation at this level, then an equal or greater symptomatic interval at 6 months5).
It has not been clearly demonstrated whether previous degenerative changes, disc height or herniated disc volume are factors which predispose the development of a new hernia after carrying out a microdisectomy.9–11
The main objective of this study was to compare the factors associated with lumbar disc recurrence in patients who had undergone surgery for disc recurrence (cases) vs patients with microdisectomy with no recurrence (control group). The secondary objective was to analyse the intraoperative and postoperative complications and the rate of re-intervention in patients operated on for herniated disc.
Material and methodsStudy sampleA retrospective study of 177 patients with disc herniation who underwent surgery in our centre between January 2010 and December 2014.
Patients aged 18 or over were included, with a diagnosis of central lumbar or posterolateral disc hernia, who had undergone surgery with simple microdiscectomy, with a minimum follow-up of one year.
Patients who had undergone previous surgery on the lumbar region, or associated procedures such as fixation, or decompression at more than one level were excluded. Foraminal and extraforaminal hernias were excluded. Patients with radicular compression at the expense of osseous components (facet hypertrophy) who required partial foraminotomy and facetectomy were also excluded.
Surgical techniqueAll operations were carried out by the surgical team in our centre. In all cases a simple microdiscectomy was performed. This study was conducted by physicians trained in spine conditions who had not participated in the operations.
Surgical technique: with the patient under general anaesthesia, they were positioned in ventral decubitus position on the radiolucent operating table. Presurgical and intrasurgical level marking with radioscopy was made. Unilateral laminotomy and precise removal of the ligament flavum was performed. Partial facetectomy was not performed, since this could have changed stability. Under magnified vision, we proceeded to remove the herniated fragment, preserving the content inside the disc. Standard intradiscal discectomy was not performed on any patient although the presence of free fragments in the posterior third of the disc space was explored. When a free fragment was present, it was removed.
The rate of relapses and further operations was analysed descriptively as were those of infections and the need for arthrodesis. Age, gender and body mass index (BMI) were analysed.
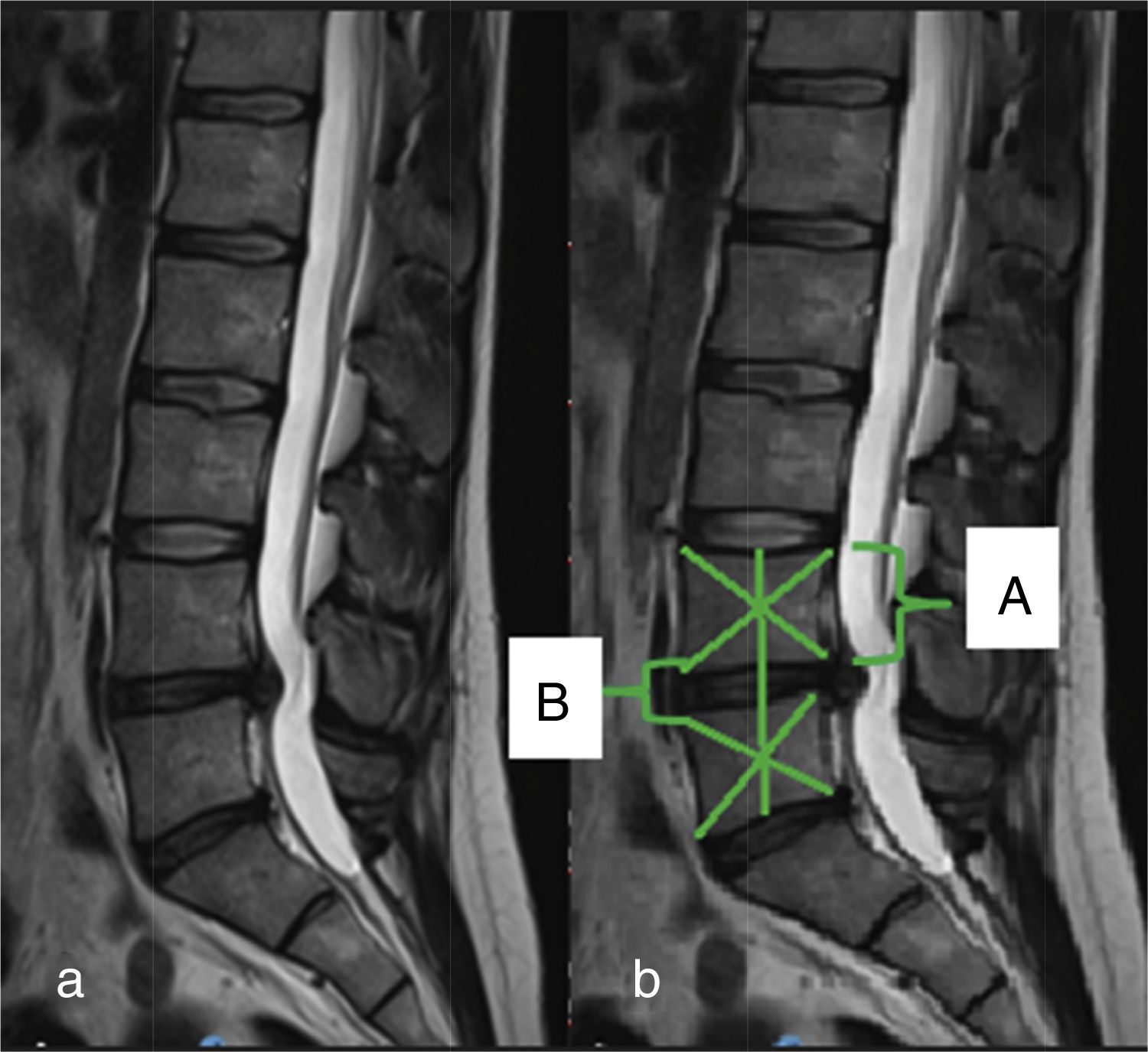
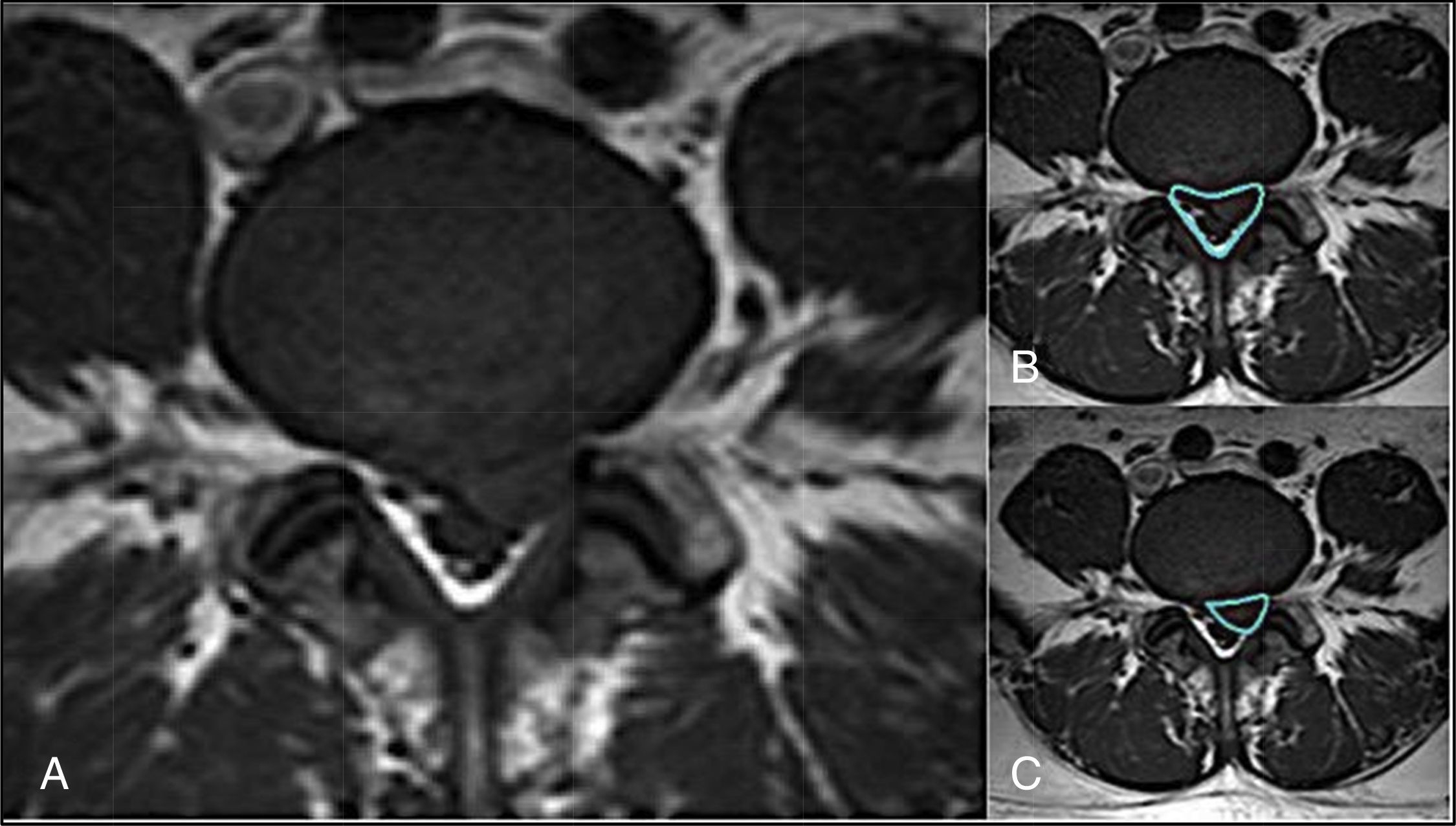
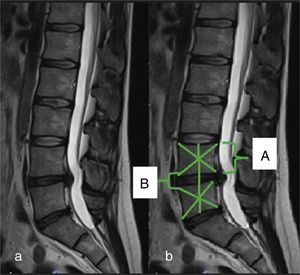
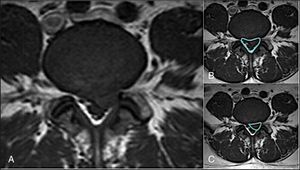
Qualitative analysisThe nuclear magnetic resonance imaging was analysed prior to surgical intervention in all cases. The level and type of discal hernia was analysed, the degree of discal degeneration through the Pfirrmann classification in sagittal T2 slices.12 Lumbar facet joint degeneration in magnetic resonance were analysed according to the Grogan classification.13 Grade 1: uniformly thinned cartilage completely covers the joint surfaces. Grade 2: the cartilage totally covers the joint surface, but there are irregular regions of erosion. Grade 3: the cartilage does not completely cover the joint surface and there are areas of bone exposure. Grade 4: only “streaks” of cartilage are noticeable in the joint. Facet degeneration changes are considered to be present in grades 2, 3 and 4, and to be normal in grade 1. The presence of changes in the intervertebral discs were analysed according to the Modic classification,14 the extension of the herniated disc in T1 and T2 with differentiation between protrusion, extrusion and sequestration15 in accordance with the Masaryk et al. method,16 the disc height index using the Mochida et al.17 method (Fig. 1) and the canal percentage occupied by the herniated disc in T2 axial slices of the affected level (Fig. 2). A comparison of the factors mentioned between the patients who did not present a relapse was subsequently carried out (group 1, control) and the patients who presented with relapses (group 2, cases).
Male patient aged 34 with a central lumbar disc hernia at L4-L5. Measurement of the percentage of the disc height at hernia level with respect to the superjacent vertebra: (a) sagittal slice from magnetic resonance imaging; (b) measurement of sagittal disc height and upper vertebral body. Disc height index (B/A×100).
Male patient aged 25, who presented with an L4-L5 posterolateral hernia. Measurement of the spinal canal percentage occupied by the disc extrusion: (A) axial magnetic resonance at protrusion level; (B) measurement of the spinal canal diameter; (C) measurement of the hernia diameter.
The Surgimap version 2.2.1 programme was used for magnetic resonance measurements.
Statistical analysisCategorical variables are described as relative and absolute frequencies (percentages). Quantitative variables are described as means and their standard deviation or as medians and interquartile ranges, in accordance with distribution. Comparisons of categorical variables between groups was performed using the Chi-square test or the Fisher exact test, in accordance with the assumptions. Comparisons of quantitative variables were performed using the student's t-test or with Wilcoxon rank-sum (Mann–Whitney) test, in accordance with the assumptions.
The value of p<0.05 was considered to be statistically significant. For data analysis the software STATA v14 (Texas, U.S.A.) was used.
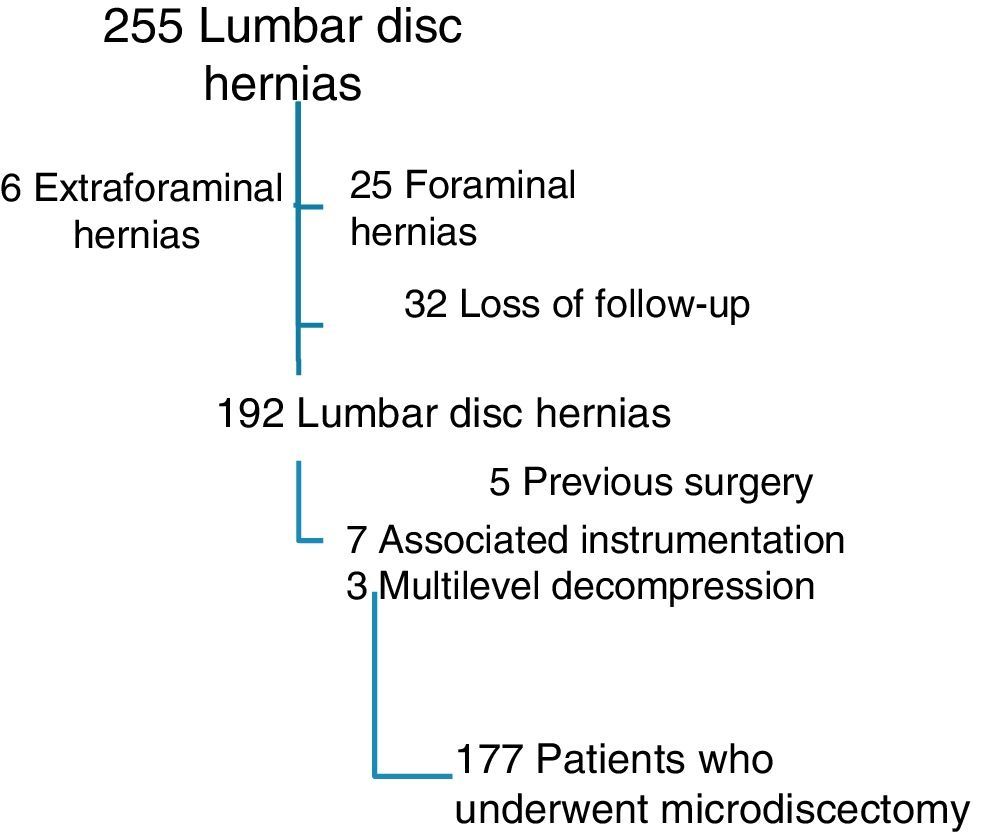
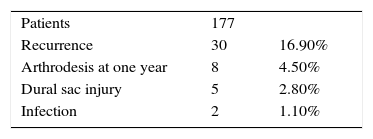
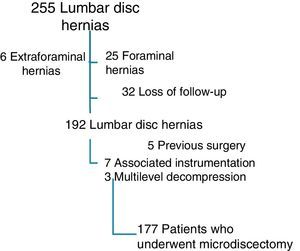
Results255 patients were analysed, 32 of whom were lost to follow-up or who did not complete the year of follow-up; 25 patients presented with foraminal hernias and 6 with extraforaminal hernias, 5 had undergone surgery before, 7 presented with associated instrumentation and 3 required more than one level of decompression (Fig. 3).
The final study sample comprised 177 patients, of whom 110 were male and 67 female, with an average age of 49.5 years and an average follow-up of 18.2 months (Fig. 3).
Thirty patients presented with relapses (16.9%), 27 of whom underwent further operations (6 months±10 days). In the group of re-operated patients, 19 required re-discectomy and 8 re-discectomy plus intersomatic arthrodesis. Finally, 3 patients with relapses did not require surgery and were treated with periradicular block injections.
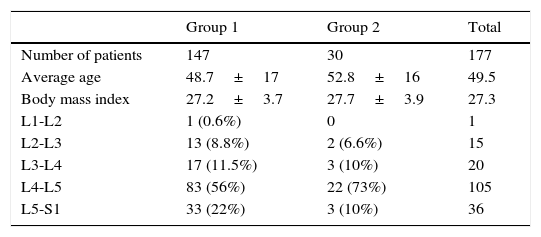
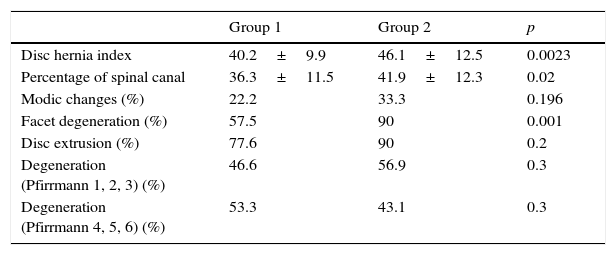
Age, gender and body mass indexThere were no significant differences with regards to age (p=0.16), male/female (p=0.9) and BMI (p=0.46) in both groups, and these variables therefore had no relationship in our study (Table 1).
Disc height indexThe comparative analysis of the disc height index with respect to the upper vertebra demonstrated significant differences between both groups. The average disc height index in group 1 was 40.2% (SD 9.95), and in group 2 was 46.1% (SD 12.49) (p=0.0023).
Percentage of disc occupancy of the spinal canalThe percentage of the spinal canal occupancy by the disc was significantly greater in group 2 (41.89 [SD 12.3]) compared with group 1 (36.3 [SD 11.5]) (p=0.02).
With regards to the presence of disc extrusion, 112 patients of group 1 (77.6%) and 27 patients of group2 (90%) presented with disc extrusion; 22 patients (15%) from group1 presented with sequestration and 11 patients (7.5%) presented with protrusion; 2 patients of group 2 (6%) presented with protrusion and one (3%) patient presented with sequestration. No significant differences were observed between the groups (p=0.2).
Comparison of degenerative changes at facet levelSignificant differences were observed with regards to the presence of facet degenerative changes between the groups under study, with higher percentages of compromise in patients with recurrence (90%) compared with the control group (57.5%) (p<0.001). The group with recurrence were also observed to suffer from higher levels of facet degeneration (grade1: 3 patients [10%]; grade 2: 7 patients [23%]; grade 3: 11 patients [36%], grade 4: 9 patients [30%]) compared with the group without recurrence (grade 1: 62 patients [42,5%], grade 2: 59 patients [40%], grade 3: 19 patients [13%], grade 4: 7 patients [4,7%]). In the group with recurrence grades 3 and 4 were the most prevalent compared with the control group control, where grades 1 and 2 were most common (p<0.001).
Comparison of the extent of disc degeneration (Modic, Pfirrmann)With regard to the presence of Modic changes no significant differences were observed between the groups (p=0.19).
We did not observe significant differences between disc changes with regards to the Pfirrmann classification (p=0.3) (Table 2).
Comparison of factors related to a disc hernia.
| Group 1 | Group 2 | p | |
|---|---|---|---|
| Disc hernia index | 40.2±9.9 | 46.1±12.5 | 0.0023 |
| Percentage of spinal canal | 36.3±11.5 | 41.9±12.3 | 0.02 |
| Modic changes (%) | 22.2 | 33.3 | 0.196 |
| Facet degeneration (%) | 57.5 | 90 | 0.001 |
| Disc extrusion (%) | 77.6 | 90 | 0.2 |
| Degeneration (Pfirrmann 1, 2, 3) (%) | 46.6 | 56.9 | 0.3 |
| Degeneration (Pfirrmann 4, 5, 6) (%) | 53.3 | 43.1 | 0.3 |
Table 3 mentions the intra and postoperative complications in the series.
DiscussionMicrodiscectomy continues to be the gold standard for lumbar disc hernia when it does not respond to conservative treatment. In our series the rate of reoperation was 15.3% (27 patients). Kim et al.18 in a series of 12,816 patients who were operated on for lumbar disc hernia with microdiscectomy found that the rate of reoperation was 13.7%.
Martin et al.19 reported a reoperation rate of 19% in non fusion surgery in patients operated on for lumbar disc hernia and of 24% in fusion surgery (arthrodesis) in a series of 24,882 patients. Lebow et al.,20 in a prospective study, analysed the rate of recurrence at 2 years in lumbar microdiscectomies, and observed a rate of 25% recurrence by magnetic resonance, the majority of which were asymptomatic. In our series we analyse clinical recurrence, so real incidence of hernia recurrence is sub-estimated.
Many factors associated with recurrence in patients with lumbar disc hernia have been described, including demographic factors (age, gender, tobacco habit, BMI), morphological characteristics of the disc (size, location, type of hernia), degenerative changes and surgical characteristics (type of approach, volume removed and ring defect).
By analysing demographic factors Suk et al.5 observed that the male gender, youth and a tobacco habit were risk factors related with recurrence. Furthermore, Keskimäki et al.21 observed that patients under 50 presented with a higher risk of recurrence. There was also a greater risk of recurrence in obese patients. As described in the work by Meredith et al.,22 where the rate or recurrence was analysed in 75 patients (group recurrence: BMI 33.6±5.1 vs group without recurrence: BMI 26.9±3.9). In our series we did not observe any significant differences regarding age, gender and BMI.
With regards to our comparative analysis between patients with good results and patients who were re-operated on, we found statistically significant differences between both groups with respect to the disc height index (46.1 in the group with recurrence vs 40.2 in the control group), the percentage of canal occupation (42 in the recurrence group vs 36.3 in the control group) and facet degeneration (89.2 in recurrence group vs 57.5 in the control group).
Dora et al.,11 in their retrospective comparative analysis of 60 patients, did not observe any differences with regards to the disc protrusion percentage in the spinal canal and recurrence, but they found a greater degree of recurrence of hernia in patients with lower degenerative changes and higher disc height (Pfirrmann 1–3). In contrast, Cinotti et al.23 made a prospective study of 76 patients (group study: 26/control group: 50) and observed a higher rate of recurrence in patients with discs with advanced degenerative changes. The strength of the said study is that it is a controlled prospective study but presents heterogeneity in the group as it presents patients with associated stenosis or epidural healing. In our series, however, we observe significant differences with regard to the changes described by Pfirrmann; the results of which could be due to the sample size of our study.
Kim et al.24 analysed the recurrence factors of disc hernia in relation to radiological parameters (disc degeneration, disc height and range of sagittal mobility) at L4-L5. There was a higher incidence of discs with grades III, IV and V degeneration compared with grades I, II and VI (DHI<0.15). Furthermore, there was a significant difference on comparing group disc height with recurrence (0.37±0.09) vs the group with no recurrence (0.29±0.09). Similar results were obtained in our study where significant differences were observed between the recurrence group (0.46±0.1) and the control group (0.4±0.09) with regard to disc height index.
With regard to Modic changes, the presence of the Modic 1 change has been connected to poor postoperative outcome, as has the persistence of lumbar pain.25 However, Ohtori et al.26 concluded that there was no relationship between postoperative results and the presence of Modic type changes1 in patients who had undergone microdiscectomy, and there is therefore some controversy in the literature. In our study, we did not observe any relationship between Modic changes and disc recurrence. Probably there is a need for greater casuistic analysis to establish a possible relationship.
With regard to the relationship between degenerative facet changes and the higher risk of recurrence, no articles have been found in the literature which mention said possible association. The presence of facet liquid and degenerative changes with segmental instability have been related,27,28 but the relationship between recurrence and facet degeneration has not been clearly established. In our series, when comparative analysis was made, we found there were significant differences, with a higher percentage of degenerative changes and a higher level of degeneration in the recurrence group compared with the control group. However, we cannot establish a direct causal relationship. Further study is needed for an in-depth analysis of this possible relationship.
We also observed a higher rate of re-operation, more than half within the first postoperative year. This demonstrates the relevance for stricter control during the first year of surgery.
We should mention the limitations of our study. Firstly, the retrospective analysis based on clinical history data and magnetic resonance outcomes are limiting. We are unaware of the real rate of recurrent hernia incidence, since we analysed the clinical recurrence of patients who required a new resonance due to the presence of clinical symptoms. It is probable that the some hernia recurrence was not clinically obvious and was therefore not included in the study.
ConclusionRecurrence in patients who have undergone lumbar microdiscectomy is a common complication. In our series the most important factors associated with recurrence were: initial disc height, percentage of disc material in the canal and degenerative fact joint change.
Further studies are required for a precise establishment of the factors associated with recurrence in patients with lumbar disc hernia.
Level of evidenceEvidence level III.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have adhered to the protocols of their centre of work on patient data publication.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Camino Willhuber G, Kido G, Mereles M, Bassani J, Petracchi M, Elizondo C, et al. Factores asociados a recidiva de hernia de disco lumbar luego de una microdiscectomía. Rev Esp Cir Ortop Traumatol. 2017;61:397–403.