To evaluate the clinical and radiological outcomes of these fractures treated through a modified posterior approach with a distal humerus plate.
Material and methodsBetween 2013 and 2015 we performed a retrospective study of these fractures surgically treated in our centre. Inclusion criteria: older than 18 years old, no pathological fractures, follow-up 1 year at least. 23 patients underwent surgery, mean age 45 years old, with an average follow-up of 18 months.
Patient characteristics, aetiology and type of fractures were recorded. The surgery was performed using Gerwin modified posterior approach with a posterolateral distal humerus plate. Clinical results were evaluated using Quick DASH, MEPS, VAS. Radiological results were also evaluated. Complications associated with treatment and radial nerve palsy incidence were recorded as well.
ResultsType of fracture according AO/OTA: six 12-A, seven 12-B, ten 12-C. 23 patients progressed to union.
After one year: QD 6.43, VAS 0.66, MEPS 88.88. No failure of internal fixation. Two superficial infections. 15 excellent results, 5 good, and 3 fair, with no poor results.
ConclusionSurgical fixation of these fractures through a modified posterior approach with a posterolateral plate minimises iatrogenic nerve injury, provides better visualisation of the proximal humerus, provides stable fixation of these injuries and results in high union rates and overall excellent functional results.
Evaluar los resultados clínicos y radiológicos del tratamiento quirúrgico de las fracturas diafisarias extraarticulares de húmero distal tratadas mediante un abordaje posterior modificado con una placa extraarticular preconformada de húmero distal.
Material y métodosRealizamos un estudio retrospectivo entre los años 2013 y 2015 de 23 pacientes mayores de 18 años, 45 años de media, con diagnóstico de fractura extraarticular de húmero distal que fueron intervenidos quirúrgicamente en nuestro centro mediante abordaje posterior modificado de Gerwin y placa extraarticular de húmero distal con seguimiento mínimo de un año y seguimiento medio de 18 meses. Se excluyeron las fracturas patológicas.
Se recogieron los datos demográficos, el tipo de fractura, la lateralidad, el mecanismo de producción y la presencia de parálisis radial. Se evaluó el resultado clínico-funcional con las escalas Quick-Dash (QD), MEPS y EVA, el resultado radiológico y el tiempo hasta la consolidación. Se recogieron la satisfacción (sí o no) y las complicaciones.
ResultadosSeis pacientes presentaban fractura tipo 12-A, 7 tipo 12-B y 10 tipo 12-C.
Todos los pacientes presentaron consolidación al año de la intervención (media 12 semanas). Nueve pacientes presentaron parálisis radial prequirúrgica y uno posquirúrgica. No hubo complicaciones relacionadas con fracasos de material y se observaron 2 infecciones de herida quirúrgica. La puntuación media de las escalas fue la siguiente: QD 6,43, EVA 0,66, MEPS 88,88; 12 resultados fueron considerados como excelentes, 3 como buenos y 3 como suficientes.
ConclusiónLa osteosíntesis de este tipo de fracturas con placa extraarticular empleando el abordaje de Gerwin presenta una tasa de complicaciones muy baja, permite la exploración del nervio radial con una buena exposición proximal del húmero, permite reducción anatómica con montaje rígido y estabilización absoluta de la fractura, dejando libre las articulaciones, obtiene altas tasas de consolidación con excelentes resultados funcionales y una rápida vuelta a la actividad de los pacientes.
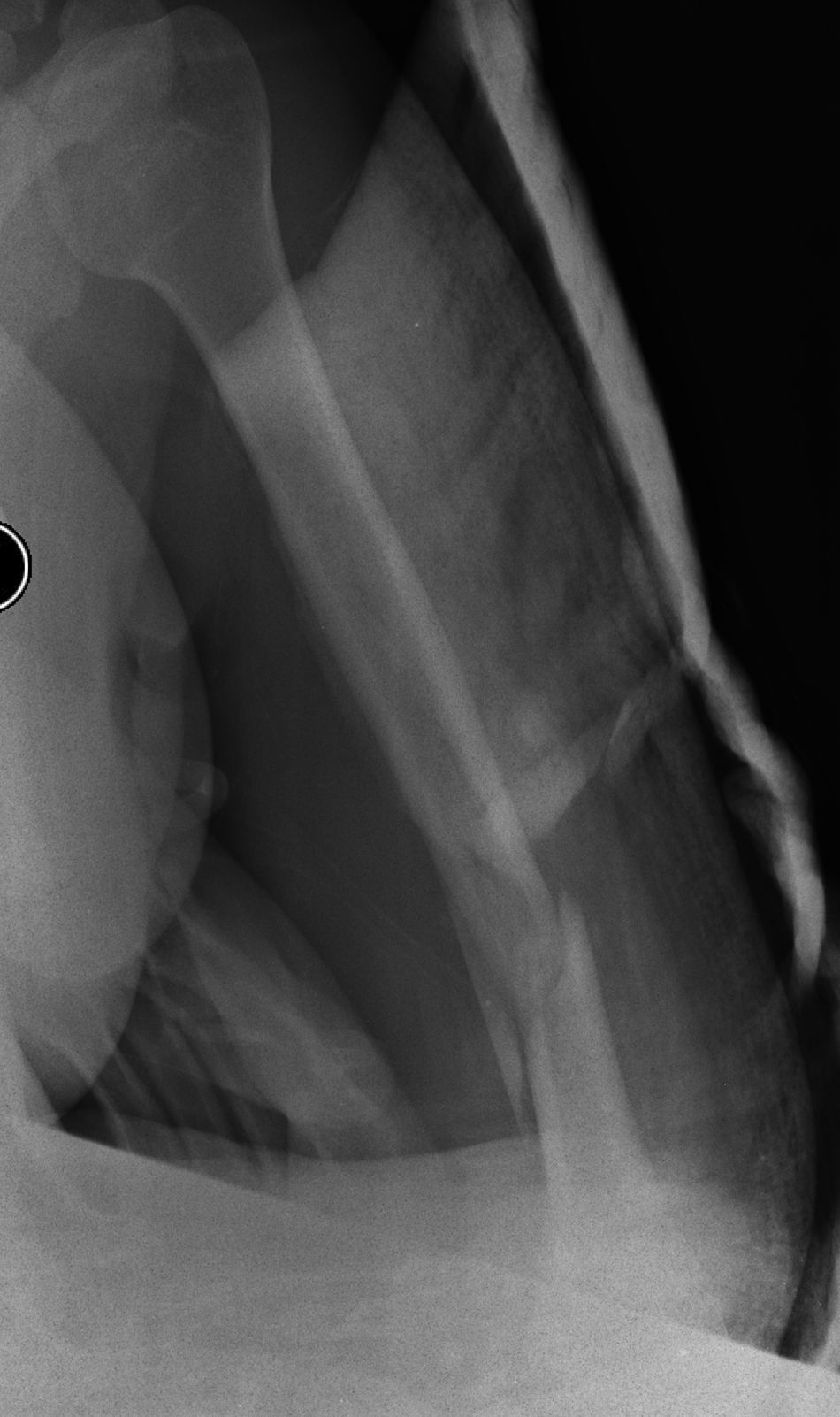
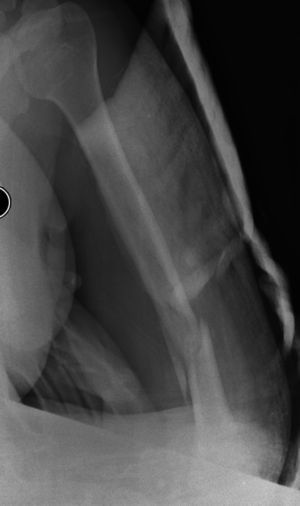
Distal third diaphyseal fractures of the humerus are difficult lesions to treat due to their location close to the joint, which conditions a small distal fragment (Fig. 1). Conventional straight plates are problematic as they only allow for diaphyseal anchorage, and they may be insufficient on occasions. Treatment with intramedullary nails presents the same problem. Soft tissue injuries also present as does association with radial nerve palsy as it passes through the torsion channel. There is no universally recognised treatment for these fractures. Both conservative and surgical treatments have been proposed1 with surgery being preferred by the majority of surgeons today. Surgery may entail osteosynthesis with differently configured plates and intramedullary nailing.2
The Basel study used conservative treatment and obtained high consolidation rates. Some of the problems associated with this treatment are the difficulty of controlling angular deformities and greater rates of non-union, misaligned consolidations and a decrease in articular range of the elbow, principally caused by prolonged immobilisation.1
Surgical treatment of extra-articular distal-third diaphyseal fractures of the humerus provides a more predictable alignment and potentially a more rapid return to daily activity, thanks to the possibility of early rehabilitation and the avoidance of soft tissue problems caused by orthoses.3
Several approaches have been used for this surgery, including trans-tricipal, direct lateral, percutaneous and the modified posterior approach described by Gerwin et al.4 The latter permits excellent humeral exposure, is anatomical and enables exhaustive exploration of the radial nerve.
The proposal of this article was to assess the clinical and radiological outcomes obtained in our centre after surgical intervention of the extra articular distal humerus fractures using a modified posterior approach as described by Gerwin et al., with posterior osteosynthesis using a posterolateral extra articular distal humerus preformed plate.
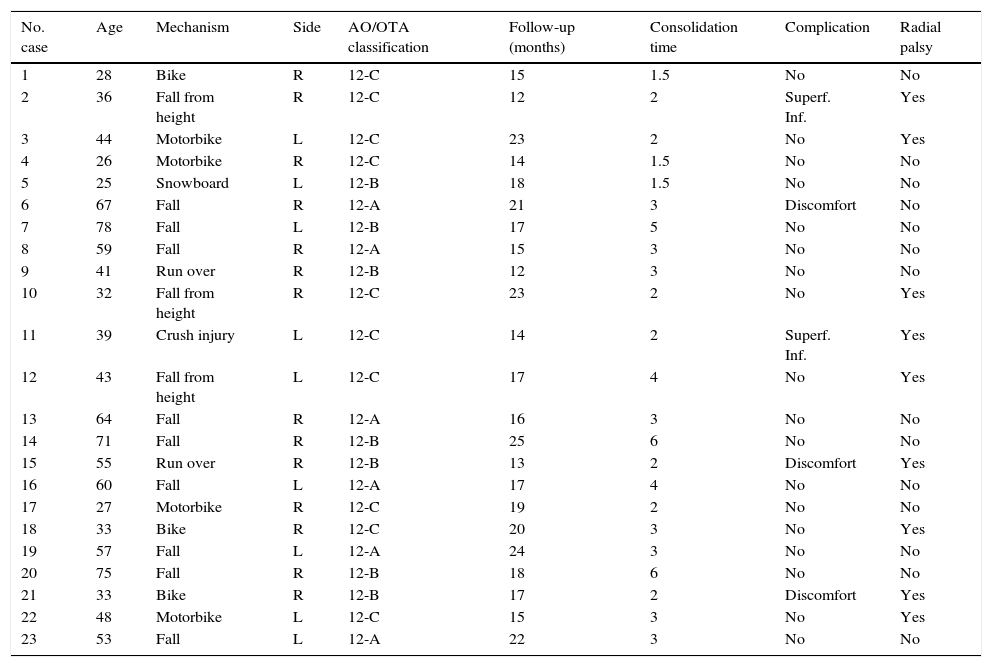
Material and methodWe performed a retrospective study of patients over 18 who had undergone surgery in our centre for extra-articular distal-third diaphyseal fractures of the humerus, 12-, subgroups A, B and C according to the Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association Committee for Coding and Classification (AO/OTA), through a modified posterior Gerwin approach4 and a posterolateral extra articular preformed 3.5mm LCP plate (DePuy Synthes, West Chester, PA, U.S.A.) in its most distal region, between the years 2013 and 2015. These patients had not presented with a pathological fracture and follow-up had been at least one year. After applying these inclusion and exclusion criteria we obtained a total of 23 patients. The group under study comprised 13 women and 10 men, with a mean surgical intervention age of 45; 14 fractures were of the left humerus and 9 of the right, 11 of them in the dominant arm. The causes of the fractures were 9 casual falls, 3 bicycle accidents and 4 motor cycle accidents, 3 falls from a height, 2 road accidents (getting run over), one sports accident (snowboard) and one crush injury. The fracture pattern was classified in accordance with the AO/OTA classification and resulted in: 6 12-A fractures (26%), 7 12-B fractures (30%) and 10 12-C fractures (44%). Mean follow-up was 17.7 months. None of the fractures were open nor derived from vascular injuries. The rate of radial palsy prior to surgery was 39.1% (9 patients).
The result was assessed from a clinical and functional viewpoint, comparing it with the contralateral limb, using the Quick DASH (QD), Mayo Elbow Performance Score (MEPS) and visual analogue scale (VAS). Patient satisfaction with the interventional was gleaned (yes/no). The radiological outcome was also evaluated with regard to whether or not there had been displacement, and the presence or non presence of consolidation was assessed every 1.5, 3, 6 and 12 months and the time during which this took place. Treatment-driven complications were also collected.
Surgical techniqueThe approach described by Gerwin in 1996 or the posterior modified approach was used in all cases.4
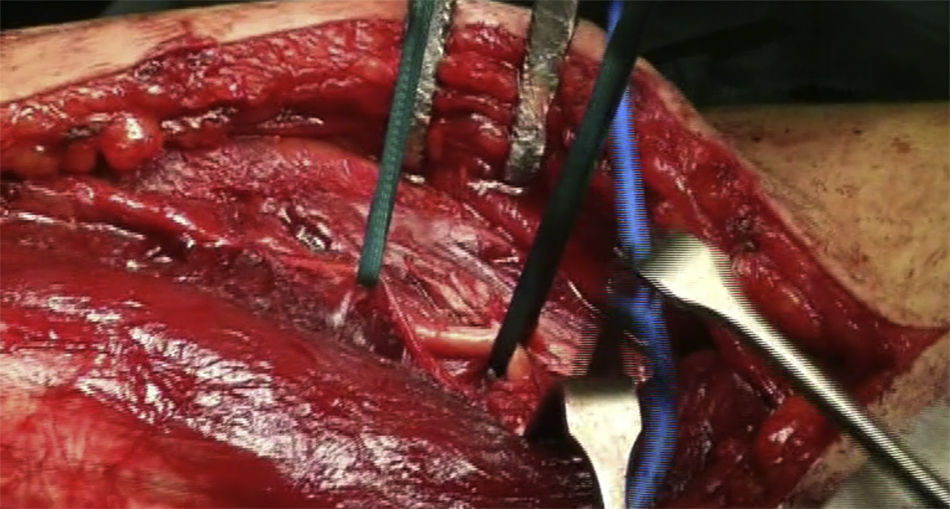
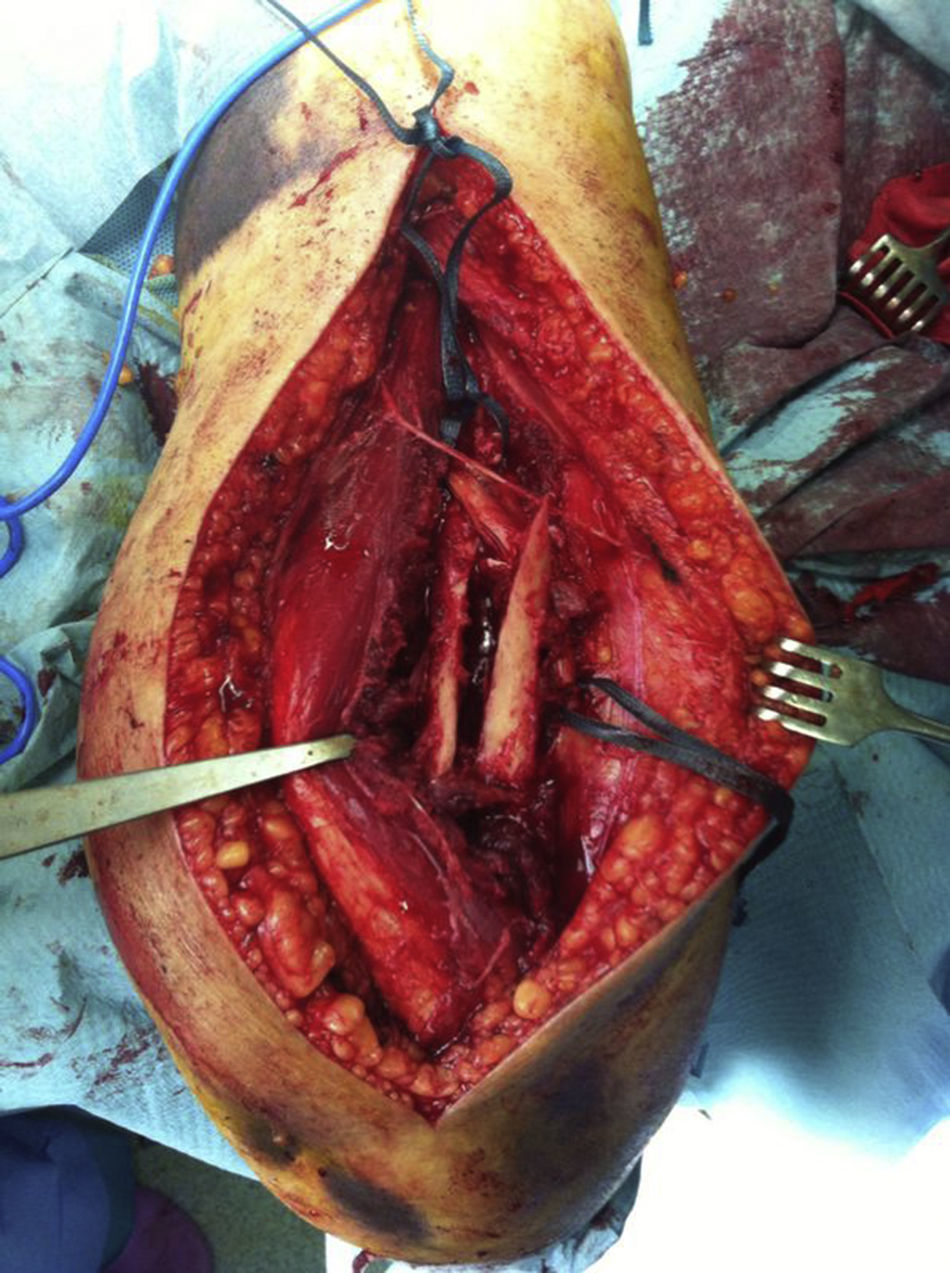
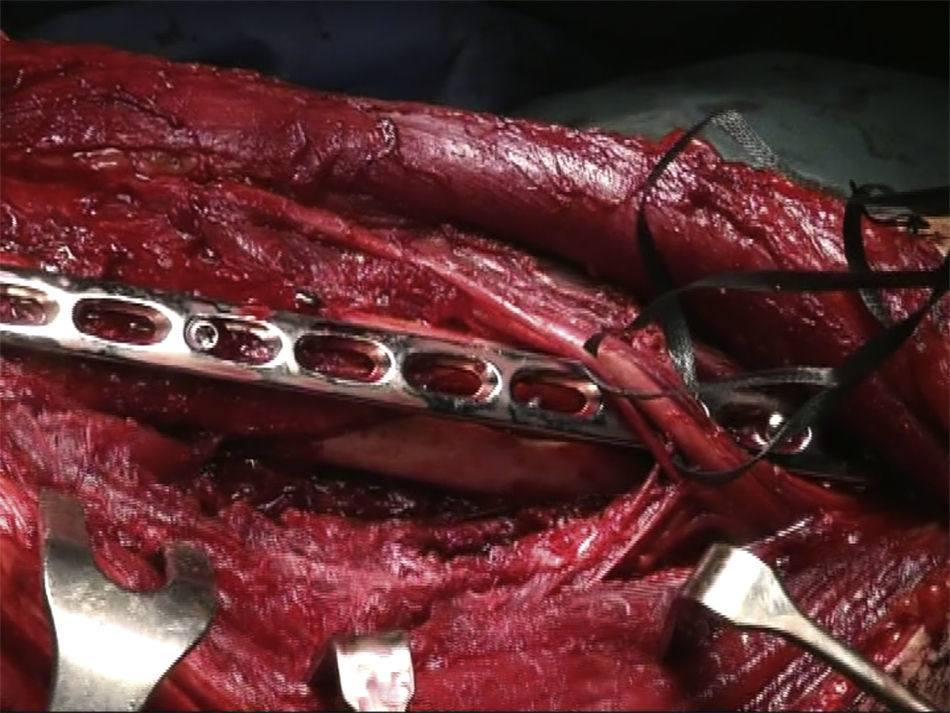
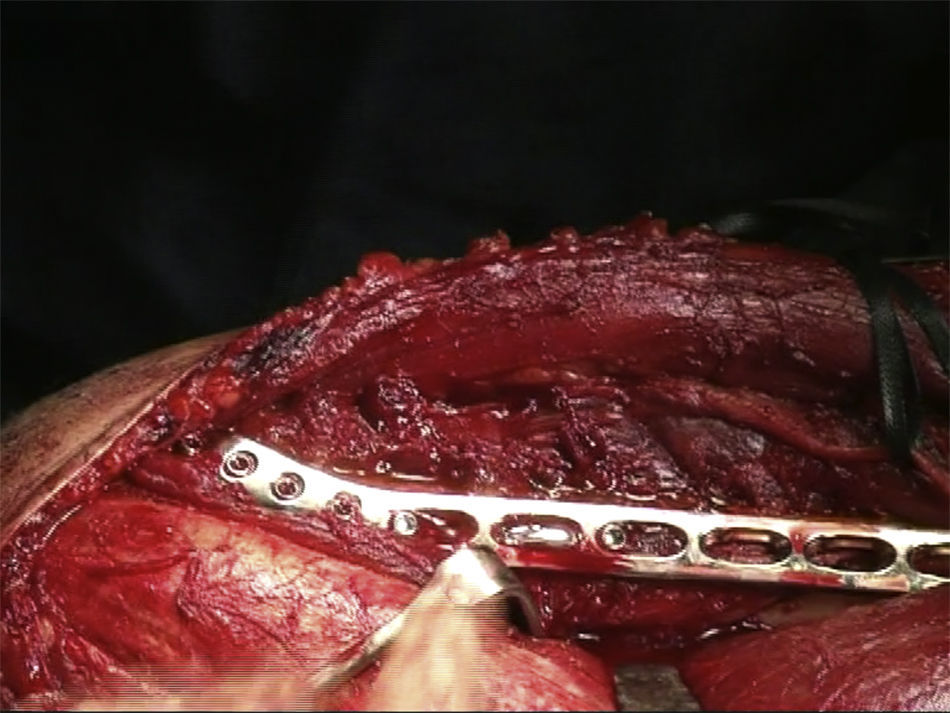
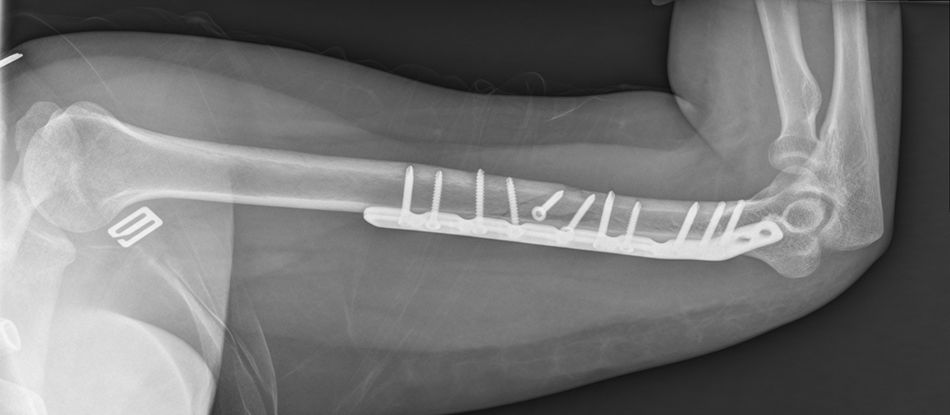
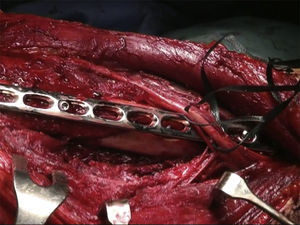
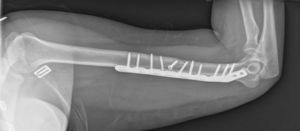
The patient is placed in a lateral decubitus position with the affected limb on a support and the elbow flexed at 90 degrees. A longitudinal incision is made in the posterior region of the arm, the length will depend on how proximal the fracture is, and is prolonged up to the olecranon fossa, but without overunning it (Fig. 2). We first search for the cubital nerve in the region medial and distal to the incision, in order to protect it during the intervention. Afterwards, in the lateral region of the incision, just below the fascia, the external brachial cutaneous branch of the radial nerve is located, as it branches away from the radial nerve once the nerve has overrun the torsion cannel and has been laterally positioned, posterior to the intermuscular septum (Fig. 3). When this branch has been cut, the intermuscular septum is distally cut for total exposure of the nerve, and we continue along it up to the radial nerve. In this way we may examine the nerve to ascertain as to whether it has suffered from any injuries or has been entrapped by the fracture (Fig. 4). Once the radial nerve and fracture have been identified, fracture synthesis is performed through the standard treatment pattern for humerus fractures. Firstly compression interfragmentary osteosynthesis is performed, if the fracture can withstand it. In all cases the 3.5mm LCP extra articular preformed distal humerus plate was used (DePuy Synthes, West Chester, PA, U.S.A.). The plate was centred on the posterior side of the humerus diaphysis and against the posterior cortical surface of the humerus, below the radial nerve (Fig. 5), with distal prolongation positioned in the external pillar (Fig. 6). It is important when positioning the plate to use radioscopy to ensure it is not too long in the distal region, as this may lead to pinching in the joint and subsequent discomfort and pain on extending the elbow. After ensuring that intraoperative radioscopic control was satisfactory, we proceeded to standard closure without immobilisation of the elbow.
After surgery the patient was put in a sling. Physiotherapy with pendulum movements was initiated 24h after surgery, together with active movement of wrist and hand, with no weight bearing and physiotherapy was continued after discharge from hospital (Figs. 7–9).
ResultsAll patients presented with signs of consolidation one year after intervention, with mean time to consolidation of 12 weeks. There were neither secondary displacements nor any material failures; 2 patients presented with superficial infections of the surgical wound which were resolved with intravenous antibiotic treatment and 3 patients had discomfort from the plate which limited their daily activities (Fig. 6). One patient presented with radial palsy after surgery, and this was spontaneously resolved without the need for surgical revision (Table 1).
Patient characteristics.
| No. case | Age | Mechanism | Side | AO/OTA classification | Follow-up (months) | Consolidation time | Complication | Radial palsy |
|---|---|---|---|---|---|---|---|---|
| 1 | 28 | Bike | R | 12-C | 15 | 1.5 | No | No |
| 2 | 36 | Fall from height | R | 12-C | 12 | 2 | Superf. Inf. | Yes |
| 3 | 44 | Motorbike | L | 12-C | 23 | 2 | No | Yes |
| 4 | 26 | Motorbike | R | 12-C | 14 | 1.5 | No | No |
| 5 | 25 | Snowboard | L | 12-B | 18 | 1.5 | No | No |
| 6 | 67 | Fall | R | 12-A | 21 | 3 | Discomfort | No |
| 7 | 78 | Fall | L | 12-B | 17 | 5 | No | No |
| 8 | 59 | Fall | R | 12-A | 15 | 3 | No | No |
| 9 | 41 | Run over | R | 12-B | 12 | 3 | No | No |
| 10 | 32 | Fall from height | R | 12-C | 23 | 2 | No | Yes |
| 11 | 39 | Crush injury | L | 12-C | 14 | 2 | Superf. Inf. | Yes |
| 12 | 43 | Fall from height | L | 12-C | 17 | 4 | No | Yes |
| 13 | 64 | Fall | R | 12-A | 16 | 3 | No | No |
| 14 | 71 | Fall | R | 12-B | 25 | 6 | No | No |
| 15 | 55 | Run over | R | 12-B | 13 | 2 | Discomfort | Yes |
| 16 | 60 | Fall | L | 12-A | 17 | 4 | No | No |
| 17 | 27 | Motorbike | R | 12-C | 19 | 2 | No | No |
| 18 | 33 | Bike | R | 12-C | 20 | 3 | No | Yes |
| 19 | 57 | Fall | L | 12-A | 24 | 3 | No | No |
| 20 | 75 | Fall | R | 12-B | 18 | 6 | No | No |
| 21 | 33 | Bike | R | 12-B | 17 | 2 | Discomfort | Yes |
| 22 | 48 | Motorbike | L | 12-C | 15 | 3 | No | Yes |
| 23 | 53 | Fall | L | 12-A | 22 | 3 | No | No |
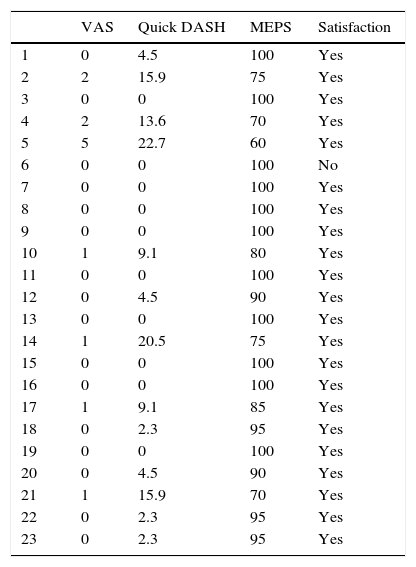
One year later, the mean score in the different clinical scales was: QD of 6.43 (range between 0 and 22.7 points), VAS for pain of 0.66 (range between 0 and 5 points) and MEPS score of 88.88 (range between 60 and 100 points). Results were compared with the contralateral limb, obtaining similar results: QD 6.43 vs 5.72, VAS 0.66 vs 0 and MEPS 88.88 vs 90.33. 12 excellent outcomes were obtained (MEPS, 90–100 points), 3 good (75–89) and 3 fair (60–74), with no poor outcomes. Regarding satisfaction, 22 patients stated they were satisfied with the surgery whilst one patient was not, due to the discomfort caused by the plate (Table 2). To date, no material extractions have been carried out on any of the patient.
Postoperative functional outcome scales.
| VAS | Quick DASH | MEPS | Satisfaction | |
|---|---|---|---|---|
| 1 | 0 | 4.5 | 100 | Yes |
| 2 | 2 | 15.9 | 75 | Yes |
| 3 | 0 | 0 | 100 | Yes |
| 4 | 2 | 13.6 | 70 | Yes |
| 5 | 5 | 22.7 | 60 | Yes |
| 6 | 0 | 0 | 100 | No |
| 7 | 0 | 0 | 100 | Yes |
| 8 | 0 | 0 | 100 | Yes |
| 9 | 0 | 0 | 100 | Yes |
| 10 | 1 | 9.1 | 80 | Yes |
| 11 | 0 | 0 | 100 | Yes |
| 12 | 0 | 4.5 | 90 | Yes |
| 13 | 0 | 0 | 100 | Yes |
| 14 | 1 | 20.5 | 75 | Yes |
| 15 | 0 | 0 | 100 | Yes |
| 16 | 0 | 0 | 100 | Yes |
| 17 | 1 | 9.1 | 85 | Yes |
| 18 | 0 | 2.3 | 95 | Yes |
| 19 | 0 | 0 | 100 | Yes |
| 20 | 0 | 4.5 | 90 | Yes |
| 21 | 1 | 15.9 | 70 | Yes |
| 22 | 0 | 2.3 | 95 | Yes |
| 23 | 0 | 2.3 | 95 | Yes |
Jawa et al. compared conservative treatment through an armlet type brace with surgical treatment through open reduction and internal plate fixation, obtaining greater consolidation rates, a better alignment and better recovery and return to daily activity with surgical treatment. It is true, however, that with the latter there is a risk of iatrogenic radial palsy and infection and therefore reintervention. Other authors state that surgical treatment reduces soft tissue complications compared with conservative treatment.1
One surgical treatment option is intramedullary nailing which is less aggressive on soft tissue, but demanding due to the narrow medullary canal at the most distal region of the humerus diaphysis and the reduced size of the distal fragment. Also, it is not possible with this approach to view the radial nerve to observe whether it has been damaged. For these reasons, osteosynthesis of this type of fracture with a plate provides clear advantages and has been established as the treatment of choice for them.2
Different approaches have been proposed over the years for this type of fracture, from a posterior trans-tricipital approach to a lateral approach, and even percutaneous synthesis, obtaining varied outcomes depending on the series with regard to iatrogenic damage to the radial nerve. In 1996 Gerwin et al., described a posterior approach which had not been much used up until that time. It consisted in finding the lateral brachial cutaneous branch of the radial nerve, and continuing along its length to reach the radial nerve in its proximity to the humerus where the nerve could be explored with little risk of iatrogenesis to itself and the fracture could be synthesised with an excellent exposure of the humerus.4
A great many plates have also been used, many of them with good results in the different studies, but they have always been conditioned by the small distal fragment problem these fractures may entail. Recommendations to increase the stability of the fractures using plates are such that the thickness of the plate has to be at least 3.5mm, and at least 6–8 cortical at each side of the fracture. However, this is complicated since the majority of plates would eventually cause pinching in the olecranon fossa. During the last few years a posterolateral extra articular plate, preformed in its most distal region, has been developed, resulting in it pointing towards the humeral condyle and leaving the olecranon fossa free. This in turn prevents pinching and increases stability and the use of more distal nails.
This study shows that surgical intervention of these fractures through osteosynthesis with preformed posterolateral extra-articular distal humerus plate using the modified posterior approach leads to stable and anatomical reduction, with no iatrogenesis and with respect for the elbow and shoulder joints, early recovery of movement, and very good functional outcome, very few complications and without the need for further surgery in any of our patients to date.
In this study we assess the results from using a single posterolateral 3.5mm plate through a modified posterior approach. Several works have studied the use of a 4.5mm plate for this type of fracture, and even the use of 2 plates, which are also valid especially in comminuted fractures, since they provide stiffer fixation than a single plate.5
Notwithstanding, the rate of consolidation in our study was 100% with a single plate, and therefore with sufficiently rigid fixation, with immediate possibility of mobilisation and with theoretical advantages compared to using 2 plates of lower periostic damage, less muscular dissection, lower blood loss and less time in surgery. It also has advantages over using a single 4.5mm plate due to its low profile and curved morphology in the distal region providing highly distal fracture synthesis capacity with sufficient distal holes to the fracture where the plate is fixed to the bone and stays there even beyond the joint.6
Some authors favour the use of intramedullary nailing in these fractures when they are not highly distal. It is true that with nailing iatrogenic risk is lower than with the surgical approach but with the modified posterior approach the risk of iatrogenesis is minimal. Furthermore, the radial nerve cannot be observed with nailing at the fracture site, unless the site were altered, whereby the theoretical benefit of nailing would be lost.
It is true that several authors prefer not to perform an initial surgical exploration of the nerve, unless the fractures are open, irreducible or reduction is inadequate, where there is associated vascular damage, radial palsy after manipulation of the fracture or untreatable neurogenic pain. If none of these risk factors are present, due to high nerve recovery rates.7 no exploration of the radial nerve would be necessary, unless symptoms were prolonged beyond 16–18 weeks.
However, other authors think that early exploration of the radial nerve prevents posterior muscular atrophy, a compromised recovery of the nerve, and a reduction in the patient's activities during the symptomatic period.8 Not many series define the number of trapped radial nerve cases at the fracture site after examination, but in studies where the radial nerve is reviewed, either initially or following the failure of conservative treatment, this occurs in 10% of cases.7,8
We think that given the high rate of radial palsy and radial nerve trapping at the fracture site (10%) in this type of fracture: 9 patients out of 23 in our study, 7 of whom presented with radial nerve trapping at the fracture site, in patients with more comminute and complex fractures and with good surgical outcomes using plates by this approach, it is necessary to examine the radial nerve, and thereby avoid higher patient discomfort and future revision nerve surgery (Fig. 6).
Another advantage of plate osteosynthesis for this type of fracture compared with nails is its respect for joints. Surgery with nails compromises the gleno-humeral joint. A relatively recent review of Cochrane determines that the only difference between the use of plates or nails in diaphyseal humerus fractures is that with nails there is a higher risk of provoking pinching in the shoulder, leading to greater stiffness of the shoulder and the need to extract material.3
One of the different approaches used for fixing the plate of this type of fracture is the trans-tricipital approach, which has fallen into disuse due to the high rate of postoperative iatrogenic radial palsy it causes and the postoperative reduction in elbow mobility and triceps strength, compared with the modified posterior approach.9
Another fairly well-used approach is the direct lateral approach on the diaphysis. This approach obtains good results according to different authors, both with regard to consolidation of the fracture and iatrogenic radial palsy, but exploration of the radial nerve is more complicated.10
Moreover, from our viewpoint, it is a less convenient approach due to the position of the patient and there is less exposure of the proximal humeral diaphysis in cases of a highly proximal fracture region, compared with the modified posterior approach.
A percutaneous approach has been described in randomised studies with very favourable outcomes, but without the exploration of the radial nerve which we believe to be necessary in this type of fractures.11
We consider that the best surgical approach for this type of fracture is the Gerwin modified posterior approach, because it is anatomical; non iatrogenic; it permits safe exploration of the radial nerve; the position of the patient on the operating table is very comfortable for surgery and anatomical reduction of the fracture may be made with excellent exposure of the proximal diaphysis of the humerus.
Patients should be warned about the risk of reintervention. Different studies have reported up to 15%-20% of reinterventions.1,12 Others reported a lower rate of reintervention in small patient numbers.13-15
In our series none of the patients have had to undergo further surgery to date, and follow-up has been at least one year. There are 3 patients with discomfort caused by the plate, and we have recommended that they do not undergo further surgery, due to the risk of radial nerve damage a new surgical approach in the region could entail. At present none of the 3 have sufficient symptoms for reintervention, since none of their discomfort limits their daily activities. This is in line with recent, very similar studies which obtained very good outcomes without reinterventions and with a very low rate of complications, with the exception of slight discomfort in the elbow.16
The limitations of our study would be the low sample size and the retrospective nature of it. However, since results were good they could be extrapolated to a much larger series.
ConclusionSurgical intervention for this type of fracture through modified posterior approach is highly promising and non iatrogenic. High consolidation rates and generally excellent functional results are obtained with a preformed distal humerus plate; the rate of complications is low and there is rapid recovery of patient activity. Prospective studies are needed with a larger sample size to confirm the results of our study.
Level of evidenceEvidence level IV.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Páramo-Díaz P, Arroyo-Hernández M, Rodríguez Vega V, Aroca-Peinado M, León-Baltasar JL, Caba-Doussoux P. Tratamiento de las fracturas diafisarias extraarticulares de húmero distal por abordaje posterior modificado y placa extraarticular. Rev Esp Cir Ortop Traumatol. 2017;61:404–411.