Most of the studies available in the literature related to the treatment of femoroacetabular impingement (FAA) with surgical hip dislocation (CLD) come from Europe and North America. This study describes the short-term results of the LQC technique for treating PFA in a cohort of Colombian patients.
Patients and methodsWe retrospectively analysed 42 cases of PFA treated with LQC from 2006 to 2018. The same orthopaedic surgeon performed all surgeries. Clinical outcome was assessed using the Merle d’Aubigné scores, while radiological assessment was performed using the Tönnis score.
ResultsFifteen women and 25 men were included in the study, with a mean age of 36.3 years. Two patients had bilateral symptomatic involvement. Of the 42 cases, there were 13 cam type, 11 pincer type and 18 mixed. Preoperatively, 31 hips were classified as poor and moderate, and 11 as good according to the Merle d’Aubigné scale. The preoperative Tönnis radiological classification showed grade 0 in half of the cases. The mean duration of follow-up was 24 months (12–37). The final postoperative Merle d’Aubigné scores classified 7 cases as poor or moderate, and 35 as good to excellent (p < 0.05). The postoperative Tönnis score showed no significant variation. As complications, one patient had heterotopic ossification, and three had trochanteric nonunion requiring refixation.
ConclusionOur results suggest that the LQC technique for the treatment of patients with PFA shows satisfactory short-term results with a low complication rate. To our knowledge, this is the first report of results of the surgical procedure for hip dislocation in our region.
La mayoría de los estudios disponibles en la literatura relacionados con el tratamiento del pinzamiento femoroacetabular (PFA) con luxación quirúrgica de cadera (LQC) provienen de Europa y América del Norte. Este estudio describe los resultados a corto plazo de la técnica de LQC para tratar el PFA en una cohorte de pacientes colombianos.
Pacientes y métodosAnalizamos retrospectivamente 42 casos de PFA tratados con LQC desde el año 2006 al 2018. El mismo cirujano ortopédico realizó todas las cirugías. El resultado clínico se evaluó utilizando las puntuaciones de Merle d’Aubigné, mientras que la evaluación radiológica se realizó con la puntuación de Tönnis.
ResultadosSe incluyeron 15 mujeres y 25 varones en el estudio, con una edad promedio de 36,3 años. Dos pacientes presentaron afectación sintomática bilateral. De los 42 casos, hubo 13 de tipo cam, 11 tipo pincer y 18 mixtos. Preoperatoriamente, 31 caderas se clasificaron como pobres y moderadas y 11 como buenas según la escala Merle d’Aubigné. La clasificación radiológica Tönnis prequirúrgica mostró grado 0 en la mitad de los casos. La duración media del seguimiento fue de 24 meses (12–37). Las últimas puntuaciones postoperatorias de Merle d’Aubigné clasificaron 7 casos como pobres o moderados y 35 como buenos y excelentes (p < 0,05). La puntuación postoperatoria de Tönnis no mostró variaciones significativas. Como complicaciones, un paciente presentó osificación heterotópica y 3 tuvieron no unión trocantérica que requirió refijación.
ConclusiónNuestros resultados sugieren que la técnica LQC para el tratamiento de pacientes con PFA muestra resultados satisfactorios a corto plazo con una baja tasa de complicaciones. Hasta donde sabemos, este es el primer informe de resultados del procedimiento quirúrgico de luxación de cadera en nuestra región.
Femoracetabular impingement (FAI) is defined as an abnormal contact between the femur and the acetabulum during normal range of movement caused by anatomical changes in any of these structures. The change in structural relationships within the hip joint produces permanent joint pain with osteoarthritis (OA) as the principal cause of pain and stiffness in the hip in patients under 50 years of age.1–6
Several aetiologies have been proposed for FAI, including genetic factors, a history of paediatric hip disease, contact sports and previous ship fracture.2 Medical symptoms may vary, but patients mostly refer to an onset of constant spontaneous groin pain accompanied by occasional pain in the gluteus, sacroiliac or tronchanteric areas with stiffness. Onset may less frequently be rapid after a minor initial trauma event.5,7
There are 2 different types of FAI depending on the pathomechanics involved. The cam and pincer types may be found in isolated form or combined. The cam type FAI consists in abnormal morphology of the femoral head-neck union, which includes a reduction in the femoral head-neck relationship, asphericity of the femoral head and retroversion of the femoral neck which causes irregular shearing forces in the acetabular cartilage. Pincer FAI is related to an abnormal acetablar morphology and includes the projection of the anterosuperior acetabular edge, acetabular retroversion, acetabular protrusion and coxa profunda, which entail direct contact between the acetabular edge and the femoral head and neck union.1,2,5,7,8
After diagnosis, a conservative symptomatic FAI approach may be first line treatment. However, when symptoms persist after several months, and there are morphological changes demonstrated by diagnostic images, surgical intervention is the next therapeutic step. Surgical intervention seeks to restore intraarticular mechanics by reducing abnormal contact between the femoral head-neck union and the acetabulum, repairing the chondral and labral lesions. Although it is unclear whether intervention is able to delay the progression of the coxofemoral osteoarthritis, the aim of surgical treatment is to detain or delay its appearance, thus avoiding the need for total hip arthroplasty (THA).1–5,7,9,10
Although several surgical techniques have been proposed for the treatment of FAI, such as hip arthroscopy, SHD or mini-open osteoplasty, open SHD described by Ganz et al. in 2001,11 continues to be the gold standard intervention.3,12,13 SHD leads to complete viewing of the hip, providing access without restrictions to joint anomalies, without compromising the blood supply to the femoral head. This technique has been shown to have excellent medium to long-term results in reduction symptoms and slowing down the progression of OA.4,5,9,12,14,15
In the systematic review by Yeung et al., 2014,16 it was proven that the majority of studies available in the literature relating to FAI treatment originate from Europe and North America and that some demographic differences could condition the findings of the surgical treatment.16 The aim of this study was to improve global evidence on short-term results of SHD for treatment of FAI with results obtained from a Colombian cohort.
Materials and methodsPatientsWe conducted a descriptive, retrospective assessment of consecutive patients who had undergone surgical treatment for femoracetabular impingement with a surgical hip dislocation technique from 2006 until 2018 in our hospital, by the same orthopaedic hip surgeon. The hospital ethics committee approved the study. Demographic details, surgical notes and follow-up data of patients were compiled from medical records following prior informed consent by the patients, their tutors or legal guardians.
Surgery was indicated in patients with hip pain who had not responded to conservative non-surgical treatment and who had clinical symptoms and radiologic findings of FAI. The exclusion criteria for this procedure included patients with a history of congenital or acquired diseases of the hip which were not FAI (Legg-Calvé-Perthes, hip dysplasia, fractures or epiphysiolysis), those with a history of hip surgery and OA (Tönnis III and IV).
The type of FAI was classified as pincer, cam or mixed, in keeping with their distinctive appearance in the radiographies or during surgery. Radiologic assessment also included assessment of femoral or acceptable cartilage lesions, labral tears and the presence of femoral or acetabular deformities.
Initial assessment included preoperative measurements of the range of movement, pain and walking, assessed through the Merle d'Aubigné17 scale score. Based on this score, patients’ hips were functionally classified according to categories of the modified Merle d’Aubigné-Postel Score18,19 as: bad (score < 13), OK (score 13 o 14), good (score 15 a 17) and excellent (score 18). Preoperative stratification was also performed for OA with the Tönnis classification.20,21
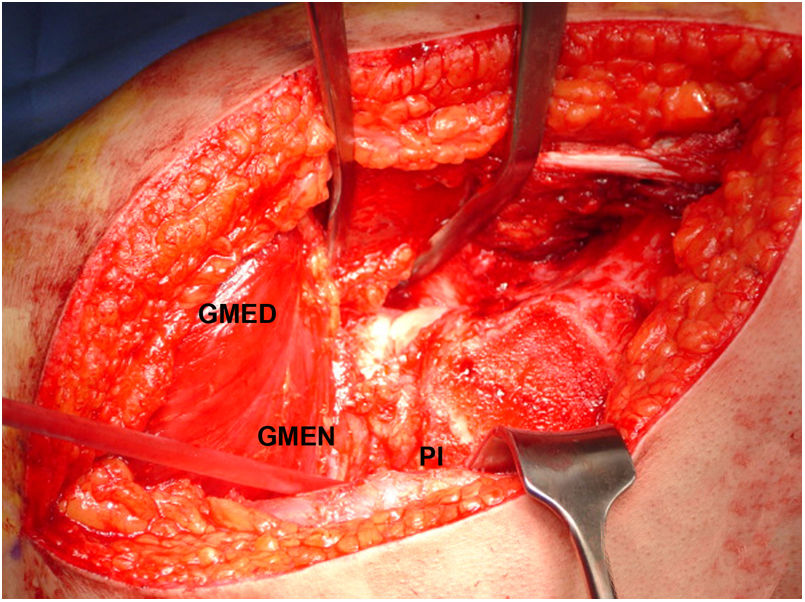
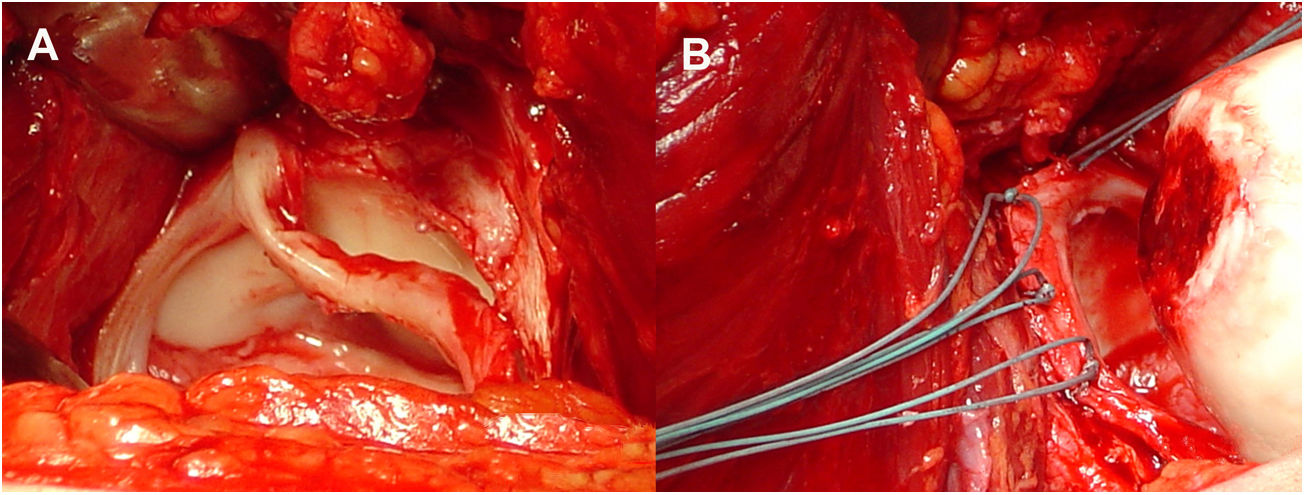
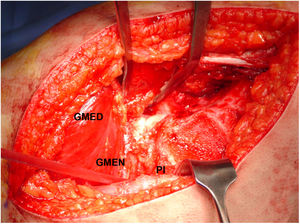
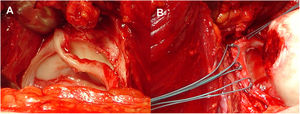
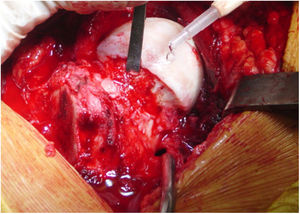
Surgical proceduresThe same senior orthopaedic hip surgeon performed all operations. Controlled surgical dislocation of the hip for the treatment of FAI is a technique previously described by Ganz et al. and other authors.8,11,22,23 The patient is placed in the lateral position, incision in the skin is performed laterally and focus is on the greater trochanter, following the femur axis. An inverted trochanteric inversion osteotomy is then performed. The gluteus minimus is moved across the gap with the pyriform muscle to the capsule (Fig. 1). After this, complete exposure of the joint is achieved through capsulotomy in Z throughout the length of the acetabular insertion. The hip is dislocated to allow complete examination of the acetabulum, assessing the status of the labrum and articular cartilage, as well as all the surfaces of the femoral head. When there is a pincer type FAI a resection acetabuloplasty is performed, sutured and labral tears remodelled (Fig. 2), unstable cartilage is resected and the denuded bone is perforated.
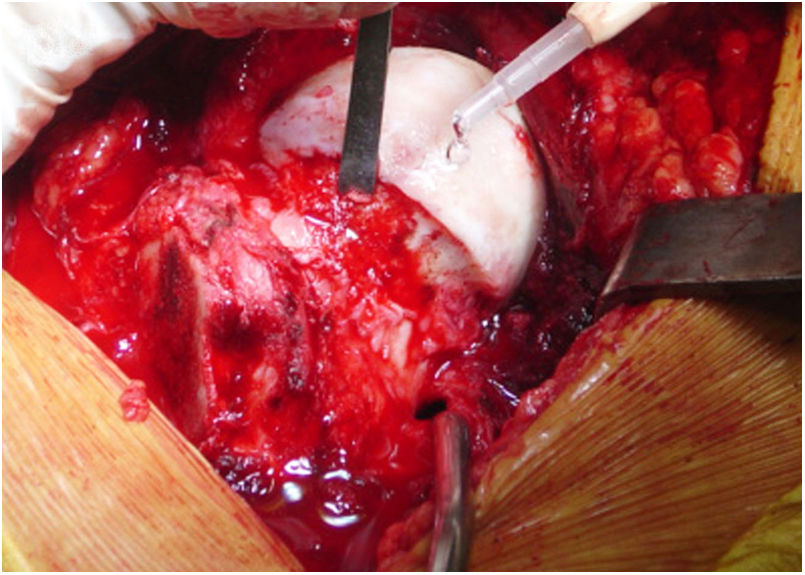
Also, in the case of a cam type FAI, both bone and cartilage are resected (Fig. 3). The hip is then reduced, verifying the absence of friction in the normal range of movement. A retinacular flap of soft tissue of the neck and the protection of external rotator muscles preserve the blood supply to the femoral head. After this capsulorraphy is performed and the greater trochanter is repositioned and attached with three 3.5 mm cortical nails.
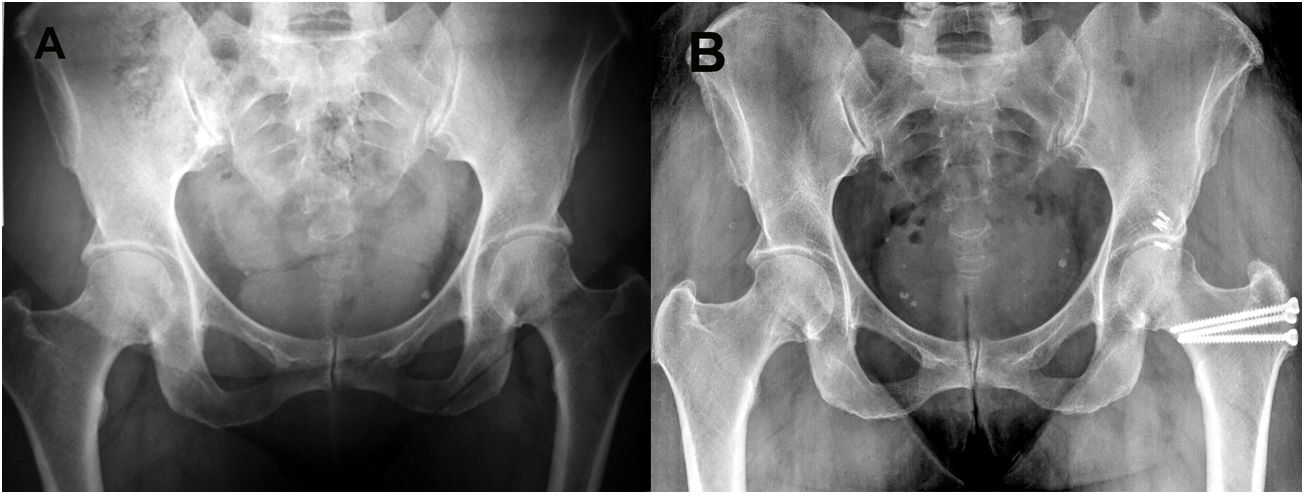
Follow-up began from the date of the procedure to the last postoperative assessment recorded in the medical records. All patients had at least one year of follow up. In the final review, the presence of critical clinical findings was assessed. Hip radiographies were used to calculate the Tönnis classification and to assess the presence of non-union or ossification. The measurements from the d'Aubigné scale were taken during follow-ups. They also assessed complications such as avascular necrosis (AVN), non trochanteric union or the need for THA (Figs. 4 and 5).
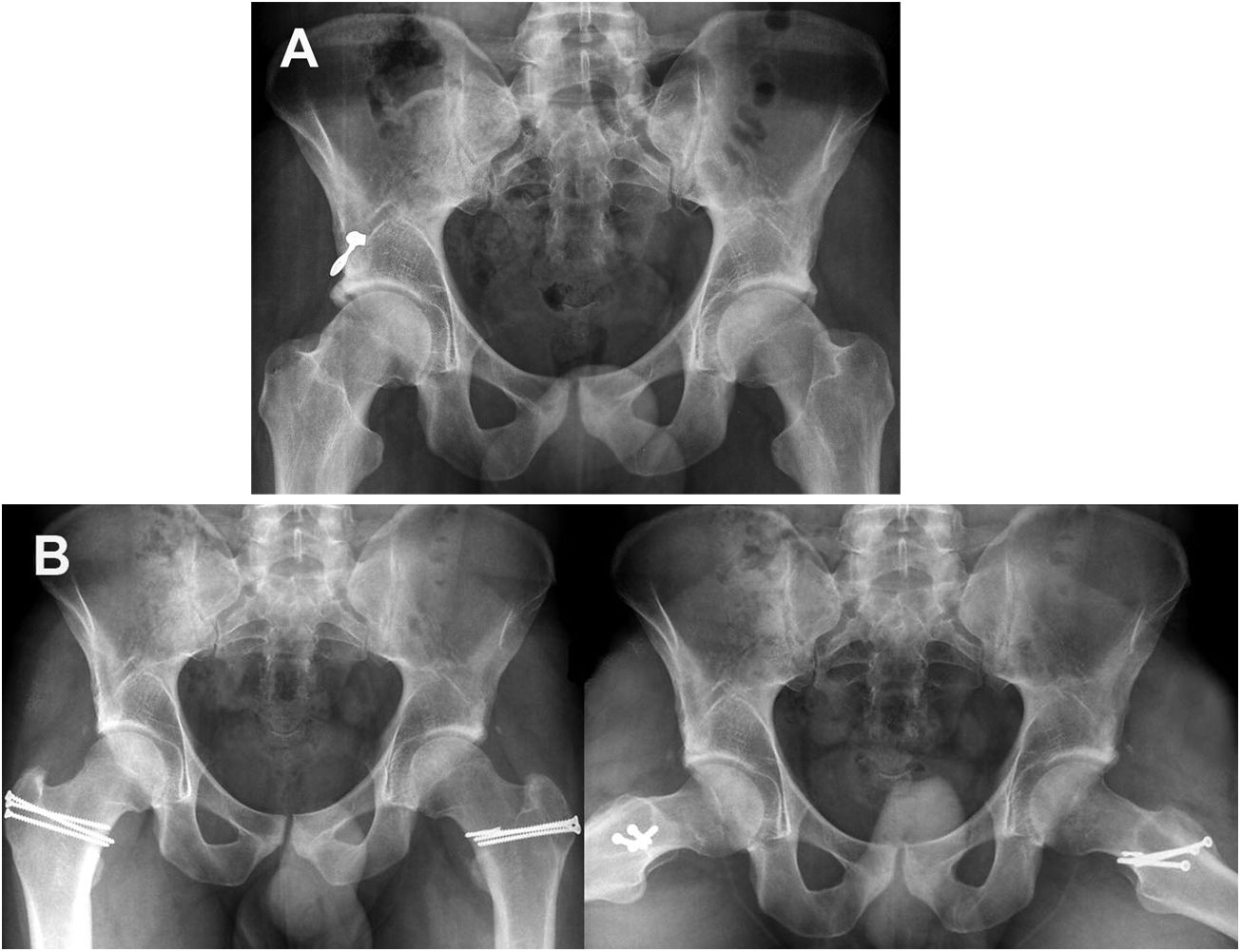
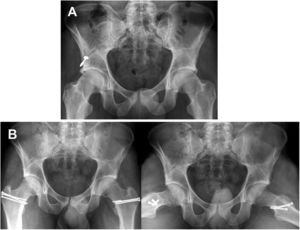
Pre and postoperative images of a pincer type deformity. A) AP radiologic image of a patient aged 46 years with bilateral pincer type FAI with symptomatic left hip that shows prominent acetabular edges; Tönnis grade I. B.) AP radiographies 12 months after SHD to correct the pincer type deformity that shows the postoperative result after osteoplasty of the acetabular edge and labral repair of the left hip.
Pre and postoperative images of a mixed type FAI. A) AP radiologic image of a 22-year-old male patient with bilateral mixed type symptomatic FAI; Tönnis grade 0. B) AP and frogleg 30 (left hip) projections and 36 (right hip) months after SHD for the treatment of mixed FAI which shows complete correction of deformities with acetabular and femoral osteochondroplasty. The labrum was not repaired due to bilateral ossification.
Description of nominal variables was made using absolute and relative frequencies, and quantitative variable through averages and range (min-max), in keeping with the sample distribution. Comparisons between quantitative variables were assessed with the Student’s t-test. For nominal variables they used the Chi-squared independence test or the exact Fisher test. Analysis was performed with the SPSS® software, versión 21.0. Statistical significance was established at a p value of ≤.05.
ResultsOf the total 65 patients who underwent surgical hip dislocation between January 2006 and December 2018, 40 patients (42 cases) met with the defined criteria and had a complete follow-up.
There were 15 women and 25 men patients aged between 15 and 56 years of age, with an average of 36.3 years at the time of surgery.
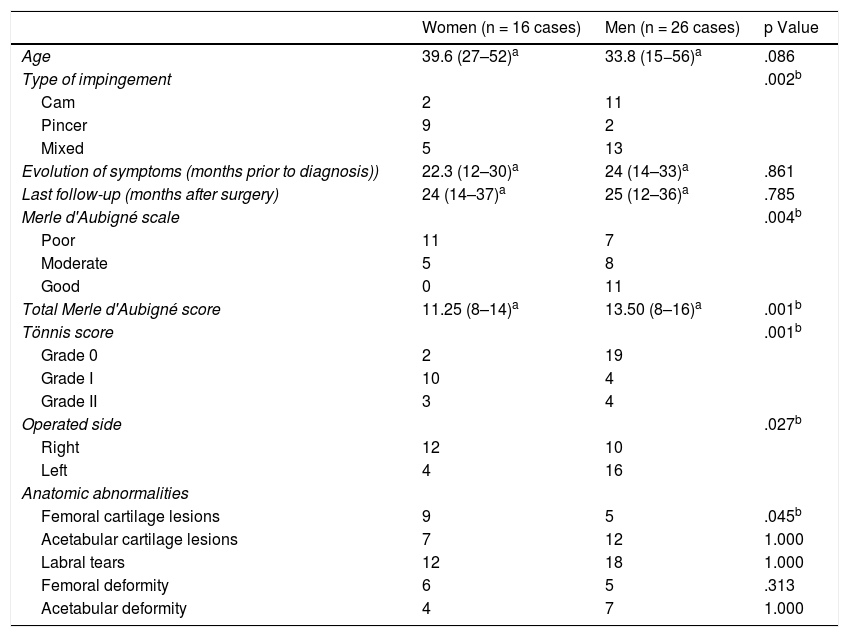
Regarding FAI laterality, this occurred on the right side in 20 patients, and on the left side in 18, with bilateral and symptomatic occurrence in 2 patients. According to the type of FSI, 13 cases were cam type, 11 pincer and 18 mixed. The average assessment time of symptoms before surgery was 22.5 months (min 12–max 33 months), and the average time of postoperative evolution was 24 months (min 12–max 37, months) (Table 1).
Description of baseline demographic and clinical characteristics of the cases stratified by sex.
| Women (n = 16 cases) | Men (n = 26 cases) | p Value | |
|---|---|---|---|
| Age | 39.6 (27–52)a | 33.8 (15−56)a | .086 |
| Type of impingement | .002b | ||
| Cam | 2 | 11 | |
| Pincer | 9 | 2 | |
| Mixed | 5 | 13 | |
| Evolution of symptoms (months prior to diagnosis)) | 22.3 (12–30)a | 24 (14–33)a | .861 |
| Last follow-up (months after surgery) | 24 (14–37)a | 25 (12–36)a | .785 |
| Merle d'Aubigné scale | .004b | ||
| Poor | 11 | 7 | |
| Moderate | 5 | 8 | |
| Good | 0 | 11 | |
| Total Merle d'Aubigné score | 11.25 (8–14)a | 13.50 (8–16)a | .001b |
| Tönnis score | .001b | ||
| Grade 0 | 2 | 19 | |
| Grade I | 10 | 4 | |
| Grade II | 3 | 4 | |
| Operated side | .027b | ||
| Right | 12 | 10 | |
| Left | 4 | 16 | |
| Anatomic abnormalities | |||
| Femoral cartilage lesions | 9 | 5 | .045b |
| Acetabular cartilage lesions | 7 | 12 | 1.000 |
| Labral tears | 12 | 18 | 1.000 |
| Femoral deformity | 6 | 5 | .313 |
| Acetabular deformity | 4 | 7 | 1.000 |
Preoperative clinical classification according to the modified Merle d’Aubigné-Postel scale was poor in 18 cases, moderate in 13 and good in 11, with a total average score of 12.60. The preoperative Tönnis score for radiologic classification of the OA showed that half of the sample was grade 0, with its majority corresponding functionally as moderate or good (Table 1).
In surgery it was observed that 15 cases had femoral cartilage lesions, 20 acetabular cartilage lesions and 31 had labral tears. The femoral and acetablar deformities were present in 11 and 12 hips, respectively (Table 1).
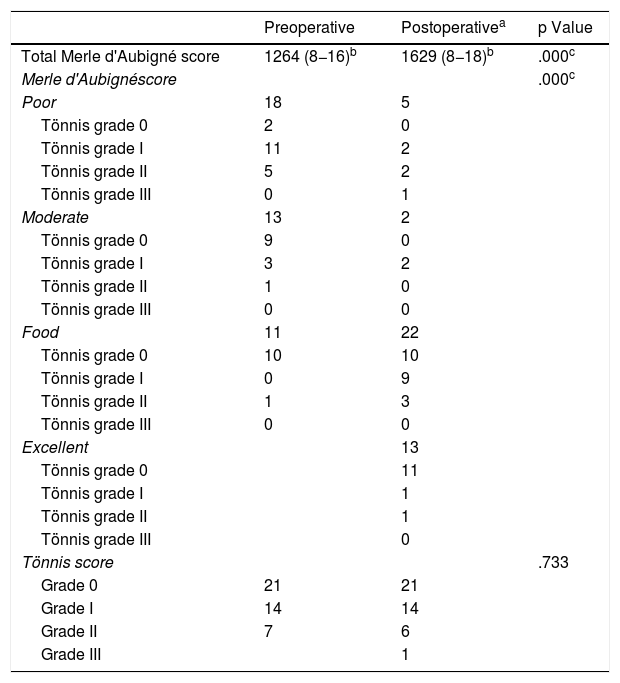
During the last follow-up, clinical classification according to the modified Merle d’Aubigné-Postel scale was poor in 5 cases, moderate in 2, good in 22 and excellent in the remaining 13 hips, with an average score of 16.28 for the total of cases. There was a significant change regarding the average preoperative Merle d'Aubigné score. Moreover, the pain score improved significantly by 4.26 presurgical points to 5.42 in the last follow-up (p ≤ .05) (Table 2).
Clinical and radiologic comparative preoperative and postoperative scores.
| Preoperative | Postoperativea | p Value | |
|---|---|---|---|
| Total Merle d'Aubigné score | 1264 (8−16)b | 1629 (8−18)b | .000c |
| Merle d'Aubignéscore | .000c | ||
| Poor | 18 | 5 | |
| Tönnis grade 0 | 2 | 0 | |
| Tönnis grade I | 11 | 2 | |
| Tönnis grade II | 5 | 2 | |
| Tönnis grade III | 0 | 1 | |
| Moderate | 13 | 2 | |
| Tönnis grade 0 | 9 | 0 | |
| Tönnis grade I | 3 | 2 | |
| Tönnis grade II | 1 | 0 | |
| Tönnis grade III | 0 | 0 | |
| Food | 11 | 22 | |
| Tönnis grade 0 | 10 | 10 | |
| Tönnis grade I | 0 | 9 | |
| Tönnis grade II | 1 | 3 | |
| Tönnis grade III | 0 | 0 | |
| Excellent | 13 | ||
| Tönnis grade 0 | 11 | ||
| Tönnis grade I | 1 | ||
| Tönnis grade II | 1 | ||
| Tönnis grade III | 0 | ||
| Tönnis score | .733 | ||
| Grade 0 | 21 | 21 | |
| Grade I | 14 | 14 | |
| Grade II | 7 | 6 | |
| Grade III | 1 |
The postoperative classification of Tönnis was grade 0 and grade I in 35 cases; with no changes in the total cases regarding preoperative scoring. However, postoperatively the grade 0 Tönnis score corresponded mostly to hips functionally classified as good or excellent. There were no significant variations in the Tönnis classification after surgery. Only one case progressed to develop OA; the patient who was a woman aged 46, deteriorated from grade II to grade III which required THA 48 months after SHD (Table 2).
There was also one case of heterotopic ossification and 3 tronchanteric non-unions which required reattachment.
DiscussionSurgical hip dislocation in patients with FAI in this Colombian cohort showed highly satisfactory results in the short-term follow-up regarding early functional results. The study results were consistent with previous studies, showing a significant improvement in the Merle d'Aubigne hip scores in patients treated for FAI with SHD.4,12,24,25
Sample size (n = 42) was comparable to other reported SHD series for the treatment of FAI, such as that of Beck et al., 2004 (n = 19)25; Espinoza et al., 2007 (n = 60)24; Yun et al., 2009 (n = 15)26; Peters et al., 2010 (n = 96)27; Jäger et al., 2011 (n = 22)15; Mladenović et al., 2014 (n = 21)10 and Steppacher et al., 2015 (n = 97).28 In a systematic review published in 2014 related to global discrepances in diagnoses, surgical treatment of FAI and research by Yeung et al.,16 showed that out of 105 studies, 34 assessed the results of the treatment with SHD and 91.4% came from North America and Europe, whilst none originated from South America.16 Our findings are therefore the only available evidence in the literature relating to the benefits of SHD as a surgical option in patients with FAI in our region.
It has been shown that a dominant male population is linked to FAI, with a male/female ratio of approximately 60/40.16 In keeping with our study, 26 of the 42 cases (62%) occurred in males. Also Amantulla et al., 20155 and Hellman et al., 20142 described that cam type FAI was traditionally found in young, athletic males who have an abnormally shaped femoral head, whilst the pincer type FAI is mostly found in active middle aged women with a deep-set or misaligned acetabulum.5 Also, in our sample, the distribution of sexes by FSI type showed greater frequency of males with an average age of 33.1 ± 10.0 years for the cam type,whilst the pincer type was more common among women with an average age of 41.2 ± 7.7 years.
The opportune diagnosis of FAI is essential to reduce the risk of permanent joint damage and OA. A delay in diagnosis could be correlated with poor outcomes and progression to OA.12,29 Several studies have reported good outcomes when the patients refer to an average of 2.3–2.5 years of duration of symptoms prior to diagnosis.12,26 In our study, the average duration between the onset of symptoms and the diagnosis was approximately 2 years (24 ± 7.00 months), which is in keeping with previous reports.
One of the first publications which reported long-term outcomes of SHD for the treatment of FAI was that of Beck et al., 2004,25 who showed satisfactory functional outcomes reflected in improvements in the Merle d’Aubigné score in 13 of 19 patients. After this, several other studies conducted by Espinoza et al., 200624 and Peters et al., 2010,27 assessed the short and medium-term results of the FAI treatment with SHD. Both studies show a significant improvement in clinical scores, reduction of pain and an improved function compared with their preoperative values in one to four years after surgery.24,27 In general, the published studies on adults with FAI have demonstrated a estimated rate of 80% of excellent and good clinician outcomes after SHD.6,7,12 Similarly, our study showed a significant functional improvement reflected in the increase of the average Merle d’Aubigné score from 12.6 to 16.2 points, especially in the reduction of pain from 4.26 to 5.42 points. With regard to the frequency in Merle categories, our cases go from 18 to 5 in the poor category, from 13 to 2 in the moderate, 11 to 22 in the good and zero to 13 in the excellent category.
In general, apart from the anatomical restoration of the femoral head and acetabulum close to normality for functional ends, the treatment of FAI has as its objective at the last instance to prevent or delay the degeneration of the hip joint which if not would lead to early osteoarthritis.3,7,8,29 The Tönnis classification provides the means for assessing the progression or stability of osteoarthritis.20,21 In our study, the Tönnis scoring showed that permanent joint damage did not progress in most cases, and direct relationship of this scoring with the functional classification was maintained. The hips with the best functional category presented with a Tönnis score of 0 pre and postsurgically. These results reaffirm that in the short term treatment with SHD was successful in achieving one of the essential objectives.
Total hip arthroplasty is a common outcome for patients with FAI in an advantage stage of osteoarthritis (Tönnis III-IV) or with chondral damage or extensive labral damage. Beck et al., 2004, reported that 5 out of 19 of their patients required THA due to stage II osteoarthritis, severe chondral damage and labral ossification.25 Equally, Peters et al., 2010; Mladenović et al., 2014 and Steppacher et al., 2015, found absolute and relative frequencies which were similar to patients who underwent THA (6.25%, 11.5% and 11%) in their respective assessed cohorts.10,27,28 In our series, a case of 42 (2.4%) required THA approximately 4 years after surgery. The patient presented with grade II Tönnis prior to surgery and progressed to grade III.
Although in recent years arthroscopic treatment for FAI has been preferred by several surgeons over SHD, various systematic reviews which compare both treatments have concluded that these techniques have similar rates of satisfactory outcomes. Neither has been demonstrated to be higher than the other.7,29,30 The procedure using surgical hip dislocation described by Ganz et al., 2001,31 is ideal for FAI treatment, since abnormal contact, be it intraarticular or extraarticular, is directly observed during the operation and in particular in posterior defects which may be difficult to observe and repair with the arthroscopic technique.10,32 Furthermore, the SHD technique enables preservation of blood flow to the femoral head with complete visualisation of the acetabulum, minimising the risk of AVN.10,11,32 In this study no patients presented ANV as a complication, which shows that SHD is a safe procedure with a low rate of complications when surgeons are experienced.7,10,32
This study is not exempt from the limitations of its retrospective design, with limited information for the periodical follow-up and the lack of a control group.
ConclusionIn keeping with what was previously demonstrated in several publications, we confirmed that SHD may be successfully used to treat patients with FAI and has a low rate of short-term complications. As far as we are aware this is the first report of results from a surgical hip dislocation procedure in this region, which establishes the importance and novelty of this study given the comparable sample size with others previously reported.
FinancingThis research did not receive any specific aid from public sector, commercial sector or not-for-profit entities.
Conflict of interestsThe authors have no conflict of interests to declare.
The authors wish to thank Doctor David Suárez for his contribution in data acquisition.
Level of evidence IV.
Please cite this article as: Sarassa C, Carmona D, Vanegas D, Restrepo C, Gomez L, Herrera AM. Pinzamiento femoroacetabular tratado con luxación quirúrgica de la cadera: resultados a corto plazo. Rev Esp Cir Ortop Traumatol. 2021;65:424–431.