To evaluate the predictive value of Modic typeII changes on nuclear magnetic resonance (NMR) prior to intervention by discectomy for lumbar disc herniation in patients with radicular symptoms.
Material and methodRetrospective descriptive study of 190 patients (58.2% men and 41.8% women) with a mean age of 43.5 years, treated between December 2005 and January 2013.
They were divided into group 1, single disc herniation (n=85), and group 2, with disc herniation and changes Modic typeII (n=80).
Variables studied: weight, height, handedness, level of injury, previous neurological deficit, postoperative complications, persistent pain and need for posterior lumbar fusion, with a mean of 67 months (group 1: 68.1; group 2: 66.8).
ResultsIn group 1 there were four hernia recurrences requiring revision surgery and six patients needed lumbar fusion. In group 2, four recurrences were also revised and eight cases requiring arthrodesis were observed.
No statistically significant differences were found when comparing the occurrence of relapse (p=.903), the need for subsequent fusion (p=.572) or in the remaining variables.
DiscussionThe data obtained and the characteristics of our study, we cannot say that Modic typeII changes were a predictive sign of the result of lumbar discectomy in our study population.
Evaluar el valor predictivo de los cambios Modic tipoII en la resonancia magnética nuclear (RMN), previa a intervención de hernia discal lumbar mediante discectomía, en paciente con clínica radicular.
Material y métodoEstudio descriptivo retrospectivo realizado en 190 pacientes (58,2% hombres, 41,8% mujeres) con una edad media de 43,5 años, intervenidos entre diciembre de 2005 y enero de 2013.
Se dividieron en grupo 1, con hernia discal simple (n=85), y grupo 2, con hernia discal y cambios Modic tipoII (n=80).
Variables estudiadas: peso, talla, lateralidad, nivel de la lesión, déficit neurológico previo, complicaciones posquirúrgicas, persistencia de dolor y necesidad de artrodesis lumbar posterior, con un seguimiento medio de 67 meses (grupo 1: 68,1; grupo 2: 66,8).
ResultadosEn el grupo 1 se registraron 4 recidivas herniarias que requirieron revisión quirúrgica y 6 casos precisaron artrodesis lumbar. En el grupo 2 se observaron 4 recidivas que también se revisaron y 8 casos que precisaron artrodesis.
No se encontraron diferencias estadísticamente significativas al comparar la aparición de recidiva (p=0,903), necesidad de artrodesis posterior (p=0,572), ni en el resto de variables.
DiscusiónCon los datos obtenidos y las características de nuestro estudio, no podemos afirmar que los cambios Modic tipoII sean un signo predictivo del resultado de la discectomía lumbar en nuestra población de estudio.
Low-back pain remains one of the main causes of incapacity and chronic disability that affects people during their working lives. This pain can have several aetiologies, for example, disc herniation, or degenerative disc disease or both. In most cases back pain improves with non-surgical therapy, reserving surgery for when this fails.1
Simple lumbar disc herniation is one of the most common diagnoses in adults with lumbar sciatic pain. In cases with evident neurological impairment, and incoercible or chronic pain, surgical treatment, such as vertebral fusion and simple discectomy can be an option. The decision to perform a discectomy is generally clear for patients with a herniated disc that has been confirmed by imaging tests and with clinical symptoms of concordant unilateral sciatic pain. However, surgeons have been reluctant to perform discectomies on patients who have disc degeneration with Modic changes revealed on magnetic resonance imaging (MRI), irrespective of the size of the hernia.2
Signal changes in vertebral end-plates were first described by Roos et al.3 and eventually classified by changes of signal intensity on MRI by Modic et al.4 They are considered a characteristic of degenerative disc disease. It is important to stress that it is difficult to know whether these changes precede lumbar sciatica, since normally an MRI will not have been performed prior to its onset.5 These changes are classified by the onset of degenerative anomalies in the vertebral end-plates and the bone marrow and can be divided into the following types6:
- •
Type I: hypointense signal on T1 and hyperintense signal on T2, due to increased vascularisation caused by mechanical stress.
- •
Type II: hyperintense signal on T1 and isointense or hyperintense signal on T2, due to the presence of fat degeneration.
- •
Type III: hypointense signal on T1 and hypointense signal on T2, caused by the presence of sclerosis.
The prevalence of Modic changes varies from 18% to 62% in patients with low back pain,7,8 with more type II Modic changes.9 These degenerative changes in the vertebral endplates cannot be consistently correlated with symptoms of low back pain, since there is currently no scientific evidence for this.10,11
Due to the lack of objective data and studies in the literature to guide decision-making for these patients, some surgeons consider performing vertebral fusion rather than discectomy, fearing persistence of chronic back pain or the recurrence of a herniated disc.
Therefore, the objective of our study was to evaluate the predictive value of a finding of type II Modic changes on MRI prior to microdiscectomy for lumbar herniated disc, in a patient with radicular symptoms. It is our hypothesis that microdiscectomy is effective treatment for patients with a herniated disc, and concordant and predominant sciatica, despite the presence of type II Modic changes.
MethodsA retrospective, descriptive study performed on 190 patients operated for lumbar herniated disc by microdiscectomy between December 2005 and January 2013 with radicular symptoms.
Patients who had undergone microdiscectomy at the same level (n=9), those who showed Modic type I changes on MRI prior to the operation (n=7), and those lost to follow-up (n=9) were excluded from the study.
The patients were divided according to the findings on MRI prior to the intervention into group 1, with simple herniated disc (n=85), and group 2, with herniated disc and Modic type II changes in the vertebral bodies at the same level (n=80).
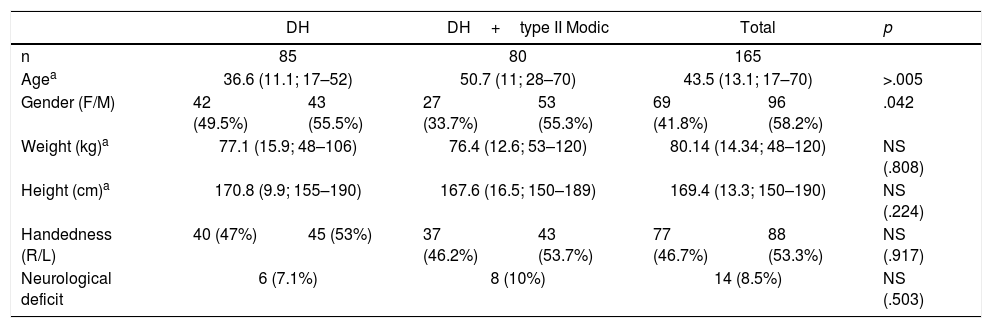
Both groups were compared by age, gender, weight, size, handedness, level of their lesion and previous neurological deficit (15 cases: 2 foot drop and 13 loss of strength). Of all the complications that can occur after this procedure, only dural tear, poor surgical wound healing and immediate postoperative pain were observed.
The need to perform a subsequent arthrodesis was observed, due to the onset of symptoms of low back pain in both groups, with a mean follow-up of 67 months.
The low back pain had to be defined as intolerable and incoercible for arthrodesis to be indicated. Because different clinicians performed the follow-up, it was defined as a VAS equal or above 4 or moderate-severe on a qualitative scale.
Pearson's chi-squared test and Fisher's exact test were used for comparing the qualitative variables, and the Student's t-test for the quantitative variables. Levene's test was used beforehand to check the homogeneity of variance hypothesis. A 95% confidence interval was estimated in all the tests.
ResultsEventually a total of 165 patients were included in the study (58.2% males and 41.8% females) with a mean age of 43.5 (13.06; 17–70) years.
There were 85 patients in group 1 with a mean weight and height of 77.1 (15.9; 48–106) kg and 170.8 (9.9; 155–190) cm respectively, 6 cases had a preoperative neurological deficit (7.1%).
There were 80 patients in group 2 with a mean weight and height of 76.4 (12.6; 53–120) kg and 167.6 (16.5; 150–189) cm, with a prior neurological deficit in 8 cases (10%).
Both groups were comparable because no statistically significant difference was found with regard to weight, height, handedness or the presence of neurological deficit prior to the surgical intervention (Table 1).
Clinical and demographic variables.
| DH | DH+type II Modic | Total | p | ||||
|---|---|---|---|---|---|---|---|
| n | 85 | 80 | 165 | ||||
| Agea | 36.6 (11.1; 17–52) | 50.7 (11; 28–70) | 43.5 (13.1; 17–70) | >.005 | |||
| Gender (F/M) | 42 (49.5%) | 43 (55.5%) | 27 (33.7%) | 53 (55.3%) | 69 (41.8%) | 96 (58.2%) | .042 |
| Weight (kg)a | 77.1 (15.9; 48–106) | 76.4 (12.6; 53–120) | 80.14 (14.34; 48–120) | NS (.808) | |||
| Height (cm)a | 170.8 (9.9; 155–190) | 167.6 (16.5; 150–189) | 169.4 (13.3; 150–190) | NS (.224) | |||
| Handedness (R/L) | 40 (47%) | 45 (53%) | 37 (46.2%) | 43 (53.7%) | 77 (46.7%) | 88 (53.3%) | NS (.917) |
| Neurological deficit | 6 (7.1%) | 8 (10%) | 14 (8.5%) | NS (.503) | |||
However, statistically significant differences were found with regard to age (p>.005) and gender (p=.042), but these were not found to be significant when a stratified analysis was performed for these variables.
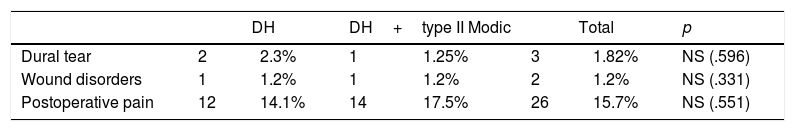
Neither were statistically significant differences found when comparing the groups in terms of complications following the operation (Table 2).
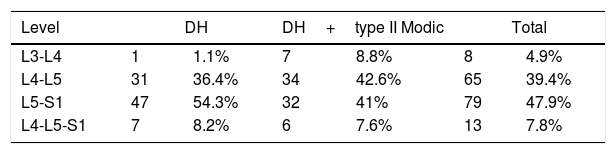
The most affected level was L5-S1 (54.3%) in group 1; by contrast, in group 2, it was L4-L5 (42.6%). The difference between each level of involvement when the two groups were compared was not statistically significant (Table 3).
Four cases suffered a recurrence of the disc herniation in group 1 (4.71%), and 6 patients (7.1%) underwent arthrodesis during mean follow-up of 68.1 months. Four cases (5%) in group 2 suffered a recurrence of their herniated disc (5%), and eight cases underwent arthrodesis at the same level due to the onset of low back pain in 8 cases (10%) in a mean follow-up of 66.8 months. No statistically significant differences were observed between either group with regard to recurrence rate or the need to perform an arthrodesis.
DiscussionAlthough the literature reports excellent results in the improvement of clinical symptoms of sciatica caused by disc herniation after lumbar discectomy, relief of low back pain is less predictable.1,7 The reason for this is not clear, but markers for degenerative disease exist. Modic changes have traditionally been considered potential risk factors,2,5 however, currently some authors maintain that their preoperative presence is not associated with postoperative clinical outcomes.12
Modic changes are closely related to the normal degenerative process that affects the lumbar spine, and their prevalence increases with age. However, the exact pathogenesis underlying these changes, their association with segmental instability of the lumbar spine and low back pain are still unclear.13 Recent studies demonstrate that the intervertebral discs with type II MC present a significant increase in IL-1β, GM-CSF and ENA-78, and there is a tendency towards increased TNF-α, thus reinforcing their association with low back pain.14
These degenerative changes are also present in a great many asymptomatic patients. Modic changes reflect the dynamic nature of spinal degeneration and it has been demonstrated that in some cases they can be reversed. Type II MC, therefore, are not as stable or quiescent as was originally thought.15 Doubts have also been raised as to whether these changes should be used as a predictive value of clinical symptoms or surgical outcome.12 It is difficult for the surgeon to weigh up these factors when contemplating a simple microdiscectomy compared to a vertebral fusion,10 since there is a substantial difference in morbidity between these two interventions.16
At present, in our practice, microdiscectomy is the standard procedure for treating patients with predominant sciatica and concordant disc herniation, regardless of Modic changes. Vertebral arthrodesis can always be considered in the future, for the cases that require it.17
One of the exclusion criteria was to have undergone a previous microdiscectomy at the same level, since postoperative type II Modic changes can occur.18
Another exclusion criterion was the presence of type I Modic changes on MRI, since on their own they have a high positive predictive value for the onset of low back pain,19,20 and they also accelerate the processes of disc and vertebral degeneration.21,22
Given the natural history of degenerative disc disease, and the multifactorial causes of low back pain, this select group of patients might go on to develop mechanical pain in the future, and require a more invasive intervention, such as vertebral fusion.23–25 However, this study demonstrated that microdiscectomy was effective in the sample of patients with disc herniation and predominant sciatica symptoms, irrespective of the presence of type II Modic changes.26,27 We also observed a recurrence rate of herniation in our patients of 4.9%, the most frequent rates reported in the literature ranging from 5% to 15%.28
In conclusion, after undertaking our study, we cannot confirm that the presence of type II Modic changes on preoperative MRI in patients with lumbar disc herniation with predominantly radicular symptoms was a predictive sign of the outcome of lumbar discectomy in the study population. Nevertheless, studies are required with a greater level of evidence and with more case reports, in order to extrapolate their prognostic value to the population in this situation.
Level of evidenceLevel of evidence III.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the research was carried out according to the ethical standards set by the responsible human experimentation committee, the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that they have followed the protocols of their centre of work regarding the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Conflict of interestsAll co-authors meet the requirements for authorship. The authors have no conflict of interest to declare.
We would like to thank Dr. A. Jaén for her collaboration in preparing the statistical analysis of the data and Dr. M. Bernaus for his collaboration in correcting the text drafted in English.
Please cite this article as: Figa R, Morera-Dominguez C. Valor predictivo de cambios Modic tipo II en la elección del tratamiento quirúrgico de hernia discal lumbar. Rev Esp Cir Ortop Traumatol. 2018;62:297–301.