Radiocarpal dislocation is an extremely uncommon injury in Traumatology, and is usually produced by high energy trauma. There are two types of dislocation, type I: pure radiocarpal dislocation and type II: fracture-dislocation. The gold standard treatment according to the literature is surgical treatment fixing the fractures and repairing the injured ligaments. We report a clinical case of radiocarpal dislocation type I in a healthy 19-year-old male after a minor trauma. The dislocation was reduced by traction, and the wrist immobilized in a plaster cast. The functional outcome 12 months after the injury was excellent.
La luxación radiocarpiana es una entidad extremadamente infrecuente y se produce habitualmente por traumatismos de alta energía. Se distinguen 2 tipos, tipo I: luxación radiocarpiana pura, y tipo II: con fractura asociada. El tratamiento de elección según la literatura es quirúrgico con osteosíntesis de las fracturas y reparación ligamentosa siendo el pronóstico pobre. Presentamos el caso un varón de 19 años que presentó luxación radio carpiana pura tras un traumatismo banal. Tras la reducción urgente fue tratado de forma ortopédica con un yeso antebraquiopalmar obteniéndose buen resultado funcional a los 12 meses de la lesión.
Radiocarpal dislocation is defined as the complete and permanent loss of joint contact between the bones of the forearm and the first row of bones of the carpus. In the large majority of cases it is due to high-energy trauma.
Moneim and Dumontier classified these dislocations into 2 types: type I, pure radiocarpal dislocation, and type II, associated to other lesions or fracture-dislocation.1,2
This pathology is extremely infrequent, with an incidence of 0.2%2,3 of all dislocations. Type I is even more rare, as there have been less than 20 cases reported in the literature.4,5 Between both types, there are only 4 series with more than 10 patients.2,6–8
The treatment is not well-established in the literature. Some authors prefer surgical treatment and have reported good results2,6,7 whilst others have published good results with orthopedic treatment.9–11
Case reportWe present the case of 19-year-old male patient. He was a right-handed hairdresser, without hyperlaxitude or previous history of interest, who attended the emergency service following a low intensity trauma on the volar side of the left wrist in a neutral position, caused by an impact from a football. Clinically, he presented “dinner fork” deformity with pain and functional impotence in the left wrist.
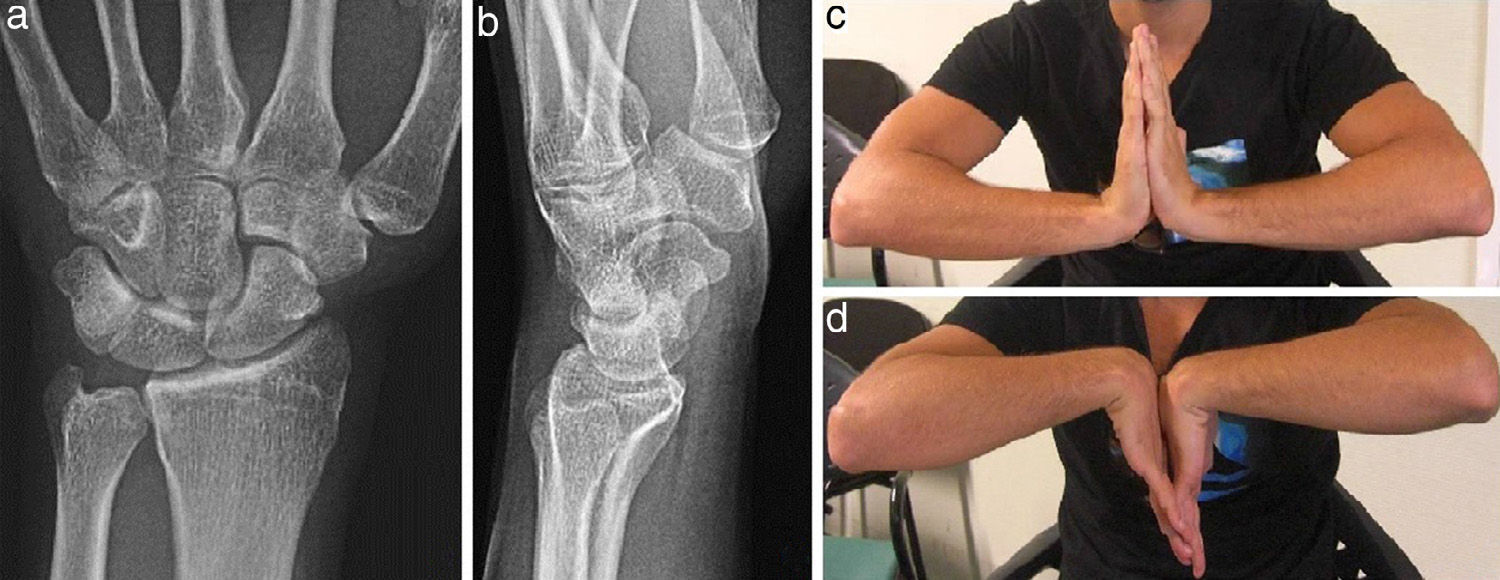
Following the initial radiographic study (Fig. 1a and b), he was diagnosed with Dumontier type I dorsal radiocarpal dislocation. We conducted closed reduction through traction at the emergency service after infiltration of a local intraarticular anesthetic, placed a closed plaster cast and radiographically verified the correct reduction (Fig. 1c and d). Given the clinical and radiographic stability, after the reduction we decided to maintain the immobilization for 7 weeks.
ResultAfter removing the cast, the patient presented flexion of 40° and extension of 35°, which improved without the need for rehabilitation up to flexion 85° and extension 70° 12 weeks after the trauma.
One year after the initial lesion, the patient reported no pain, feeling of instability or signs of nerve compression. He also presented active mobility of 92° flexion and 86° extension with preserved pronosupination (Fig. 2c and d). The control radiograph did not show any relevant alterations when compared to the contralateral wrist (Fig. 2a and b). We measured the strength (grip test measured with a dynamometer [Jamar®, Patterson Medical, Warrenville, IL, USA]) and found it to be 90.36% compared to the dominant hand. The DASH disability score result was 1.6 (range: 0–100) and the Mayo Wrist Score was 90 (range: 0–100).
DiscussionThe first case of radiocarpal dislocation, dorsal or volar and with or without fracture, was described in 19269 and, since then, less than 70 cases have been published.1,3,9–12 The majority of these cases are type II radiocarpal dislocations. We only found 9 published cases of pure dorsal radiocarpal dislocation8 and only 1 of these was similar to the one presented in this work, with a non-displaced fracture of the ulnar styloid process.9
This dislocation is normally associated to fractures of the distal radius or fractures of the carpal bones and, except in 1 case,11 is due to high-energy trauma.
The diagnosis is simple to establish through conventional radiography in 2 projections and emergency joint reduction is indicated to reduce the risk of vascular and neural lesions.
The treatment has not been clearly established, since the existing series combine different types of dislocation, different therapeutic options and, in addition, there are no long-term follow-up data.8 Most authors propose a surgical treatment with a volar approach,3 double approach5,8 or, in some cases, an arthroscopic approach with osteosynthesis of the fractures and repair of the capsule-ligament complex.6,7 On the other hand, we also found 3 published cases which were treated orthopedically through immobilization with a cast for 4–6 weeks9–11 and also reported positive functional results.
In spite of the low incidence of these type of lesions, the literature2,8,13 seems to infer that surgical treatment would be indicated in Dumontier type II dislocations, since in these kind of dislocations it is safe to assume that the radiocarpal ligaments continue to be subject to the radial styloid, so bone reduction and fixation through percutaneous or open surgery with a volar or double approach fixing the fracture should manage to achieve joint stabilization.
However, in type I dislocations, in which there is minor or no bone lesion, the indication for surgical treatment is not so clear. According to the initial work by Dumontier,3 in these kind of dislocations the radiocarpal ligaments would be damaged and the prognosis would be unfavorable. Nevertheless, this unfavorable functional prognosis is not reflected in the literature,2–7,11 rather the opposite, the results published in relation to orthopedic treatment of type I dislocations, as in our case, are positive.9–11
It is possible that this discrepancy is determined by joint stability following the reduction. Thus, an unstable dislocation after the reduction would indicate the presence of a considerable ligamentous lesion and would probably condition surgical treatment. On the other hand, if the lesion is stable after the reduction this would suggest a less severe ligamentous lesion which could, therefore, be treated orthopedically.
For the above reasons, in type I radiocarpal dislocations, after emergency reduction, it is important to assess joint stability through serial radiographic controls and, once the immobilization has been removed, clinically verify stability through forced flexion-extension maneuvers and inclinations. When instability is not observed, orthopedic treatment may be a good therapeutic alternative.
Level of evidenceLevel of evidence V.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Please cite this article as: Jiménez-Jiménez IJ, Caballero-Martel JR, Ojeda-Castellano J. Luxación radiocarpiana tras traumatismo banal. Rev Esp Cir Ortop Traumatol. 2015;59:66–68.