The purpose of the study was to evaluate the functional results after medial patellofemoral ligament (MPFL) reconstruction in patients using auto- and allograft.
Patients and methodsA retrospective study was conducted on 28 patients with recurrent patellar dislocation, with 13 patients (13 knees) undergoing MPFL reconstruction with hamstring autograft, and 15 patients (16 knees) with reconstruction surgery with allograft. The total group included 13 males and 15 females, with an age range of 15–38 years. The graft-related morbidity was studied and a clinical assessment was performed using the pre- and postoperative Kujala score. Associated complications were reported for each group. All the patients had more than 12 months of follow up.
ResultsNo recurrent dislocations or graft related complications were reported in either group. The post-operative Kujala subjective knee score was 89.2 in the autograft group, and 92.6 in the allograft group (p>.05). One patient in the allograft group received a revision surgery due to poor positioning of anchors. Another patient in the allograft group had non-displaced patella fracture related to the bone tunnels and another patient had flexion deficit and needed mobilisation under anaesthesia.
ConclusionThere were no significant differences between both groups, and the results were comparable.
Evaluar los resultados clínicos en pacientes con inestabilidad femoropatelar sometidos a reconstrucción del ligamento patelofemoral medial (LPFM) con auto y aloinjerto.
Pacientes y metodologíaEvaluación clínica retrospectiva de 28 pacientes con inestabilidad femoropatelar sometidos a cirugía de reconstrucción LPFM; se analizaron un grupo de 13 pacientes (13 rodillas) en que se utilizó autoinjerto obtenido de los tendones isquiotibiales y otro grupo de 15 pacientes (16 rodillas) con aloinjerto. El grupo total correspondió a 13 hombres y 15 mujeres con edades entre 15-38 años. Se estudió la morbilidad asociada al injerto y técnica quirúrgica, se realizó evaluación clínica con escala de Kujala, pre y postoperatoria y se evaluaron sus complicaciones. El seguimiento fue mayor a 12 meses.
ResultadosNo encontramos episodios de reluxación ni complicaciones asociadas al injerto en ninguno de los grupos. El puntaje promedio postoperatorio de la escala de Kujala en el grupo de autoinjerto fue de 89,2 y en el grupo de aloinjerto fue de 92,6 (p>0,05). En el grupo de autoinjertos un paciente fue reoperado por mala posición del material de osteosíntesis y en el grupo de aloinjertos un paciente presentó una fractura de rótula no desplazada provocada por los túneles óseos realizados y otro paciente requirió movilización bajo anestesia por déficit de flexión.
ConclusiónNo encontramos diferencias significativas entre ambos grupos y los resultados clínicos fueron similares.
Recurrent patellar instability is a frequent pathology that mainly occurs among young patients. Different surgical techniques have been described to treat it, although their indications and results are the subject of some discussion. However, reconstruction of the medial patellofemoral ligament (MPFL) has gained many adepts due to its low rate of redislocation (0–10%).1–3 Anatomical studies have shown that the MPFL is the main medial stabiliser of the patella, contributing to 80% of its lateral displacement.4,5 On the other hand, in over 90% of cases of recurrent instability there is some lesion of the MPFL.6 This fact, associated to the limited capacity for scarring of the ligament, increases the laxity of the medial retinaculum.7,8 The MPFL has a key function in the patellofemoral joint, however, reconstruction techniques employed are very different depending on each author. Several graft fixation methods have been used for different types of grafts, including autografts from the semitendinosus,9–11gracilis12 and adductor magnus13 muscles and from the quadricipital14 and patellar15 tendons, as well as synthetic16 compounds and allografts,17 but no consensus has been reached about the ideal kind of graft. Allografts have shown advantages in terms of morbidity and allow a faster recovery, but they are not extensively used. The aim of the present study is to evaluate the clinical results of patients undergoing MPFL reconstruction with an allograft and to compare these results with those from patients in whom an autograft was used, mainly regarding recurrence, results and complications. Our working hypothesis is that MPFL reconstruction using an allograft shows better results and allows a faster recovery, without associated donor region morbidity.
Patients and methodologyWe conducted a retrospective review of 28 patients who underwent MPFL reconstruction at our centre between January 2007 and February 2012. All the patients presented a history of patellar instability with a minimum of 2 episodes of dislocation. The work obtained approval from the Ethics Committee of our centre.
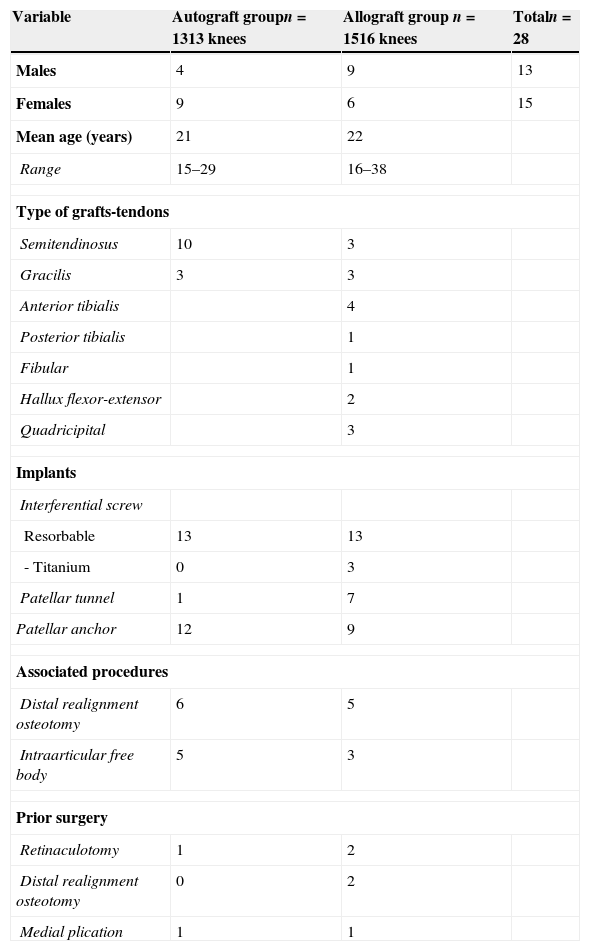
Patients were randomly divided depending on the type of graft used: group 1 included patients who underwent MPFL reconstruction with a hamstring autograft, whilst group 2 included patients who underwent MPFL reconstruction with an allograft. Group 1 included 13 patients (13 knees), with 9 females and 4 males, with a mean age of 21 years (range: 15–29 years), with a mean follow-up period of 17 months (range: 15–29 months). Group 2 included 15 patients (16 knees), with 6 females and 9 males, with a mean age of 22 years (range: 16–38 years) and a mean follow-up period of 42 months (range: 80–29 months). In both groups, MPFL reconstruction was carried out in a single procedure or associated to realignment in cases where patients presented a distance greater than 20mm between the anterior tibial tuberosity and the trochlear groove (TT–TG). In total, 7 patients from both groups presented some kind of prior surgical procedure associated to the instability (Table 1).
Demographic data of intervened patients.
| Variable | Autograft groupn=1313 knees | Allograft group n=1516 knees | Totaln=28 |
|---|---|---|---|
| Males | 4 | 9 | 13 |
| Females | 9 | 6 | 15 |
| Mean age (years) | 21 | 22 | |
| Range | 15–29 | 16–38 | |
| Type of grafts-tendons | |||
| Semitendinosus | 10 | 3 | |
| Gracilis | 3 | 3 | |
| Anterior tibialis | 4 | ||
| Posterior tibialis | 1 | ||
| Fibular | 1 | ||
| Hallux flexor-extensor | 2 | ||
| Quadricipital | 3 | ||
| Implants | |||
| Interferential screw | |||
| Resorbable | 13 | 13 | |
| - Titanium | 0 | 3 | |
| Patellar tunnel | 1 | 7 | |
| Patellar anchor | 12 | 9 | |
| Associated procedures | |||
| Distal realignment osteotomy | 6 | 5 | |
| Intraarticular free body | 5 | 3 | |
| Prior surgery | |||
| Retinaculotomy | 1 | 2 | |
| Distal realignment osteotomy | 0 | 2 | |
| Medial plication | 1 | 1 | |
All the allografts used came from the grafts bank of our centre, obtained through sterile surgical technique, without irradiation, and were previously cryopreserved.18 The allografts used in each procedure, according to availability at our bank, were semitendinosus (3), anterior tibial (4), posterior tibial (1), quadriceps with bone chip (3), gracilis allograft (2), hybrid allograft of flexor and extensor hallucis longus (2) and fibular allograft (1) (Table 1). Patients were evaluated in the preoperative and postoperative periods using the Kujala scale.19 In addition, the morbidity associated to the graft and the surgical technique were also evaluated, as were episodes of redislocation and complications at the end of the follow-up period.
Surgical techniqueAll patients underwent a diagnostic arthroscopy and in the 11 cases in which a distal realignment osteotomy was planned, this was performed before the MPFL reconstruction. We used an ischaemia tourniquet with all patients. The surgical approach was a double femoral and patellar incision. On the patella we made a 3–4cm incision aligned with the medial edge of the patellar tendon, exposing the medial edge of the patella in its 2 upper thirds. The deep layer of the retinaculum remained intact. On the femur, we made a 2cm longitudinal incision, between the femoral epicondyle and the tubercle of the greater adductor, with the knee in slight flexion, taking care not to damage the main branch of the saphenous nerve. Using a curved periostotome we differentiated the interval between the retinaculum and the capsule. The periostotome was introduced from the patellar incision towards the femoral incision to leave a retinacular tunnel through which we passed looped suture to subsequently introduce the graft. The point of femoral fixation was located with a 2.4mm guide needle, just behind the medial femoral epicondyle and distal to the tubercle of the greater adductor. Once the exact point of femoral insertion had been selected, we created a 6–7mm tunnel with a cannulated drill bit, depending on the diameter of the graft, with a depth of 25–30mm. The graft was fixed on the femur with a resorbable interferential screw in 26 cases and with a titanium interferential screw in the 3 remaining cases, in whom a quadricipital tendon allograft was used.
The 2 remaining ends of the graft were passed outside the joint between the deep and middle layers of the retinaculum towards the patella. In the first cases, they were fixed through 2 parallel transosseous tunnels in the patella and with non-resorbable suture. Due to the risk of patellar fracture, we modified the surgical technique, preferring the use of titanium anchors and non-resorbable suture. The critical point of fixation was determined with the knee at 30° flexion, avoiding excessive medial tension and reevaluating the correct tension of the graft in different ranges of flexion-extension. In extension, we evaluated the tension of the graft by displacing the patella laterally up to a maximum of 7–9mm.
PostoperativeThe rehabilitation protocol was started in the immediate postoperative, using a continuous, passive knee mobiliser during the first 48h, in an initial range of 0–30°, and subsequently adapting to the tolerance of each patient. In addition, isometric exercises of the quadriceps muscles were also started. The same protocol was followed in patients with an associated distal realignment osteotomy. At the time of discharge, patients used canes for partial load according to their tolerance for 2–3 weeks, and an articulated orthosis was placed, progressively increasing the range of mobility and removing it after 6 weeks, as long as the patient had sufficient muscle control of the limb to prevent falls and rotational instability in the knee. Physiotherapy focused on strengthening the quadriceps, and hip rotator muscles to, at the same time, avoid fibrosis of the soft tissues of the joint which might have caused joint rigidity. Dynamic training of the limb was started after 3 months, with exercises focusing on the sports activity of each patient.
Data treatment and statistical analysisThe statistical analysis was conducted by means of nonparametric tests, using the Mann–Whitney U test to compare the preoperative and postoperative Kujala scores, as well as the results between both groups. We also classified the results of the Kujala test qualitatively,20 considering a poor result ≤64 points, an acceptable result between 65 and 84 points, and a good to excellent result ≥85 points.
ResultsThe mean score in the preoperative Kujala scale was 53.8 points in the group with autografts and 60.2 points in the group with allografts. The postoperative score increased to 89.1 and 92.6 points, respectively. Both differences were statistically significant. We did not find significant differences between the groups in the preoperative or postoperative scores. We registered good and excellent results (Kujala >85) in 11 of the 13 knees (84.6%) in the group with autografts, and in 14 of the 16 knees (87.5%) in the group of allografts. In overall terms, 86.2% of operated knees corresponded to good and excellent results.
The mean postoperative score in the subgroup of patients with associated realignment osteotomy was 93.8 points in the group with autografts and 92.9 points in the group with allografts. Among patients who only underwent MPFL reconstruction, the mean scores were 84.5 and 92.4 points respectively. We did not find statistically significant differences between the subgroups.
All patients regained their range of joint mobility in the operated knee, except for 1 patient in the group of allografts who required mobilisation under anaesthesia due to a flexion deficit after 6 months from the intervention, a female in whom the MPFL was reconstructed in isolation, and who evolved favourably after the mobilisation, without requiring further procedures.
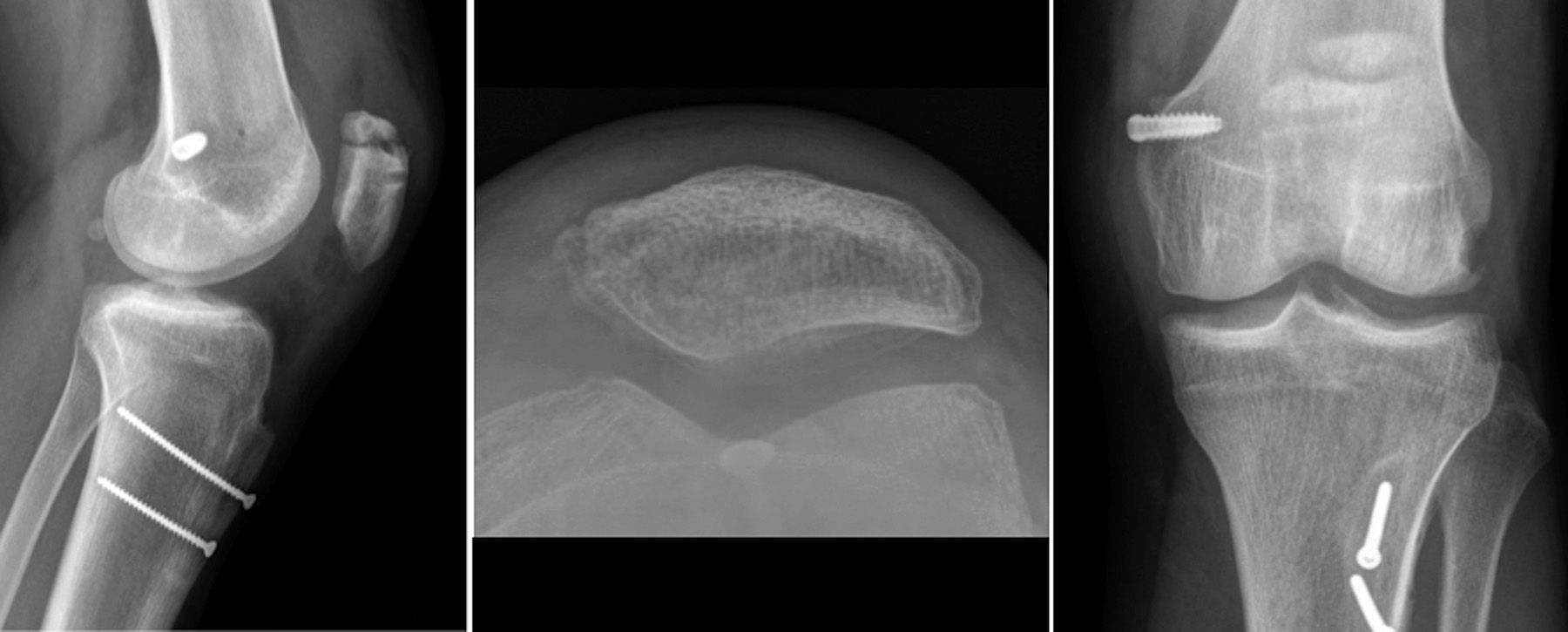
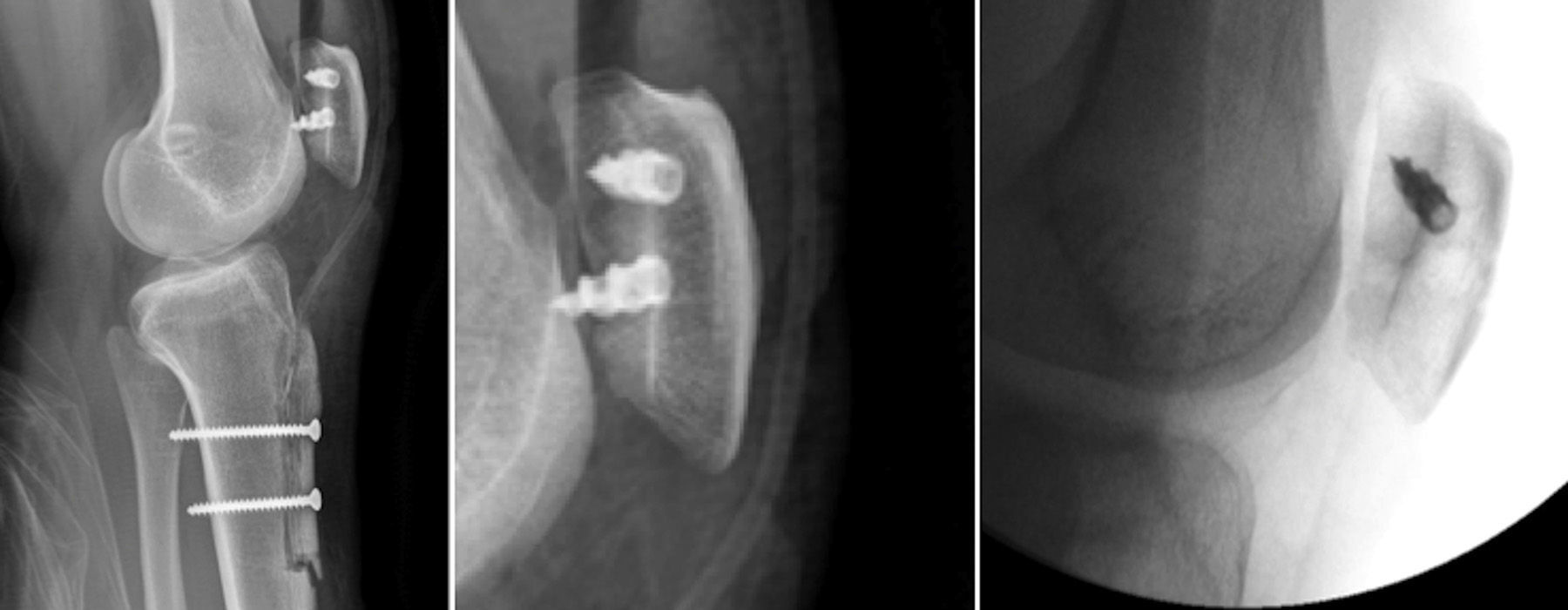
Among the complications observed, we can highlight that, in the group of allografts, 1 patient presented a patellar fracture 3 months after the surgery (Fig. 1). This was a non-displaced fracture caused by a direct trauma on a patient with transosseous patellar tunnels who was treated orthopedically with a good result. In the group of autografts, 1 patient required reintervention due to malposition of the fixation material, so the patient underwent relocation of the patellar anchors (Fig. 2). At the end of the follow-up period, none of the patients presented new episodes of dislocation or subluxation after the MPFL reconstruction procedure, and there were no cases of postoperative infection.
MPFL reconstruction has shown good results, with low rates of redislocation and a final Kujala scale score varying between 84 and 92 points.1–3 It is mainly indicated in cases of recurrent dislocation, with no bone alterations. Our series of patients presented comparable results to those reported in other works, with a rate of redislocation and overall mean Kujala score of 90 points at the end of the follow-up period. The use of allografts favours an early start of rehabilitation, as it avoids donor site morbidity, thus reducing the initial pain and allowing early work of hamstring muscles. However, these theoretical advantages were not demonstrated during the final follow-up, since we found differences in the postoperative results obtained in the group of autografts. It is worth highlighting that our series did not present any cases of postoperative infection or allograft failure, which are the complications traditionally associated to the use of cadaver grafts in other surgical procedures for ligament reconstruction.21 Moreover, we did not find any cases of hematomas or symptomatic tears in the donor region that could delay postoperative rehabilitation in the autograft group.
Regarding the complications observed in our series, both joint rigidity and patellar fracture were problems reported in the literature, generally related to the technique more than the type of graft. Joint rigidity has been reported as a common problem in proximal extraarticular procedures, particularly in MPFL reconstruction,22 although it was not frequent among our patients. Mobility deficit may have been due to several factors, including postoperative haemorrhage, delayed start of mobilisation, lack of an adequate physiotherapy protocol and errors in the graft fixation isometry that may have restricted full knee flexion. It is important to identify as soon as possible any factors that may cause rigidity and delay rehabilitation. Some published series report up to 20% of patients who required mobilisation under anaesthesia23; however, the authors admit a delay in the start of rehabilitation work due to the low resistance of femoral fixation. In our study, we only observed 1 patient who required mobilisation under anaesthesia, but she did recover full mobility. An adequate femoral and patellar fixation offers adequate initial resistance, allowing safe joint mobilisation from the first day with a low risk of causing arthrofibrosis.
We present 1 case of patellar fracture; described in the literature.24–26 All the fractures were associated to the use of patellar tunnels, with their diameter and orientation being a risk factor to take into consideration. It is for this reason that we modified the surgical technique, using patellar fixation anchors. Although some biomechanical studies have demonstrated that fixation with transosseous tunnels offers greater resistance than anchors, the difference is not significant.27
We must take into account that our series included patients who had been previously operated for other episodes of redislocation, patients suffering recurrent dislocation without bone malalignment and patients with recurrent dislocation with malalignment. According to our indications, patients who presented recurrent dislocation without alteration of the TT-TG distance only underwent MPFL reconstruction. When they presented a traumatic recurrent dislocation with alteration of the TT-TG, they underwent distal realignment osteotomy using the Elmslie–Trillat technique and MPFL reconstruction. In the subgroup of patients with autograft in whom an isolated MPFL reconstruction was performed, we observed a lower score in the postoperative Kujala scale, with no statistically significant differences compared to the same group in whom an osteotomy was associated, or with the allograft group with isolated reconstruction. Within the group of allografts, the results for both subgroups were equivalent. We believe that the association of an osteotomy adds greater complexity to the surgical procedure and subsequent rehabilitation; however, this was not reflected in the final results obtained.
Realignment has generated controversy, with some authors arguing that the benefits of reconstruction have not been proven among patients with an anatomical cause for their instability. However, we consider that a MPFL reconstruction benefits the instability surgery, mainly in cases suffering failure of medial structures or hyperlaxity after the osteotomy, due to the high rates of MPFL lesion in recurrent dislocations, in up to 94% of cases,28 and the importance of the MPFL in the biomechanics of the patellofemoral joint. It is worth highlighting that 2 of the patients who presented prior instability surgery underwent distal realignment due to altered TT–TG, presenting redislocation subsequent to their first surgery, and they improved significantly in the clinical scale after the MPFL reconstruction. In a systematic review of the results of MPFL reconstruction, Buckens et al.28 considered the heterogeneity of the series with different coadjutant procedures, which may underestimate the real success of the reconstruction. In spite of this, they concluded that reconstruction offers superior functional results, or at least equal, to those of other classical techniques used to correct instability. The heterogeneity of the patients in our series emphasises the importance of an adequate selection of cases and the need to evaluate the most adequate surgical indication in each situation in order to ensure an optimal result, since the type of graft selected does not affect the result of MPFL reconstruction.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Calvo Rodríguez R, Figueroa Poblete D, Anastasiadis Le Roy Z, Etchegaray Bascur F, Vaisman Burucker A, Calvo Mena R. Reconstrucción del ligamento patelofemoral medial. Evaluación de los resultados clínicos del autoinjerto frente al aloinjerto. Rev Esp Cir Ortop Traumatol. 2015;59:348–353.