To evaluate the results after locking plate internal fixation of proximal humerus fractures by means of a motion capture system, and functional scales.
Material and methodRetrospective study of a cohort of 47 elderly patients undergoing surgery from January 2010 to December 2014. After a minimum follow-up of two years, two functional scales (Constant-Murley and Quick DASH), and a quality of life scale (EQ-5D) were used for clinical evaluation. For objective evaluation of the range of motion a kinematic marker-free analysis with cameras was performed.
ResultsThe average age was 74.85 years. Average functional scores were: Constant-Murley 70.06 points, Quick DASH 35.74 points and EQ-5D 6.79 points. The average range of motion was: flexion, 111.49°; extension: 24.13°; abduction: 109.40°; adduction: 15.13°; external rotation: 38.96°, and internal rotation: 49.28°. Correlation was found between the two functional scales, between them and the EQ-5D, and between range of motion and functional scales (except for external rotation) as well as between range of motion and EQ-5D (except for flexion and external rotation).
ConclusionLocking plate osteosynthesis in proximal humerus fragility fractures achieved good functional and quality of life scores. Motion capture systems can be a useful tool for the functional assessment of shoulder pathology allowing an objective evaluation of range of motion.
Evaluar los resultados de las fracturas de húmero proximal tratadas mediante osteosíntesis con placa empleando captura de movimiento y escalas funcionales.
Material y métodoEstudio retrospectivo de 47 pacientes mayores de 65 años, tratados mediante osteosíntesis con placa bloqueada en el mismo centro, desde enero de 2010 a diciembre de 2014. Tras un seguimiento mínimo de 2 años, se realizó una evaluación de los resultados obtenidos mediante 2 escalas funcionales (Constant-Murley y Quick DASH) y una escala de calidad de vida (EQ-5D). Para analizar el balance articular de forma objetiva se empleó un sistema de análisis cinemático con cámaras y sin marcadores.
ResultadosLa edad media fue 74,85 años. Los resultados funcionales expresados mediante la puntuación media fueron: Constant-Murley, 70,06 puntos; Quick DASH, 35,74 puntos; y EQ-5D, 6,79 puntos. Los arcos de movilidad medios fueron: flexión, 111,49°; extensión: 24,13°; abducción: 109,40°; aducción: 15,13°; rotación externa: 38,96° y rotación interna: 49,28°. Se encontró correlación estadística entre las 2 escalas funcionales y de ambas con la EQ-5D. También se advirtió correlación estadística entre los movimientos estudiados con las escalas funcionales (excepto rotación externa) y con la escala de calidad de vida (excepto flexión y rotación externa).
ConclusiónLa osteosíntesis con placa bloqueada en las fracturas de húmero proximal del anciano obtiene unos buenos resultados funcionales y de calidad de vida. El uso de sistemas de captura de movimiento permite una medición más objetiva de estos resultados y puede ser una herramienta útil en la valoración funcional de esta patología.
Proximal humerus fractures have a high incidence rate in the population, particularly after 65 years of age, making it the third most common fracture after hip and wrist fractures.1 The most widely used treatment is still conservative treatment2 and in up to 80% of the cases, the fractures are minimally displaced and good outcomes are achieved without surgery.3 Nevertheless, there are many patients who will require surgical treatment due to the high volume of this pathology. These fractures represent a challenge for the surgeon because of their complexity, the many existing treatment options, and the high risk of complications they entail.
There is no clear consensus in the bibliography with respect to what the best option is for use in those cases that do require surgery, and individualised treatment is advocated. One of the most widely used alternatives is the utilisation of locking plates with angular stability. These implants provide outstanding primary biomechanical stability,3,4 even in osteoporotic bone, enabling the previous proximal humerus anatomy to be restored.5 While the functional results obtained with this type of fixation are satisfactory, a significant number of complications have been noted in relation to the osteosynthesis of these fractures.6–8
Several validated scales have been used to evaluate the functional outcomes following surgery for these fractures, but all of them exhibit a certain degree of subjectivity.9,10
The use of kinematics has been suggested to distinguish between true recovery (restoration of premorbid movement) and the use of compensatory (alternative) movement patterns while carrying out a task.11
Three dimensional kinematic motion capture yields an objective measurement of the joint's range of movement12 and, consequently, its comparison and expression in numeric values. Kinematic analysis describes the movements of the body through space and time, including linear and angular displacements, speeds, and accelerations.
The main objective of this study is to present the results obtained following open reduction and internal fixation with angular stability locking plate of proximal humerus fractures by means of motion capture and functional rating scales in elderly patients.
Material and methodA retrospective study of 47 patients with a displaced proximal humerus who underwent surgery with of osteosynthesis by means of a plate at an Orthopaedic Surgery and Trauma Service during the period of time between January 2010 and December 2014.
Patients were included who were over the age of 65 years, with proximal humerus fracture, treated by means of osteosynthesis with a Philos plate (DePuy Synthes, Switzerland) at our centre, who completed follow up, and agreed to undergo the kinematic test of movement analysis.
The following exclusion criteria were set: (1) individuals under the age of 65 years; (2) pathological or open fractures; (3) fractures with conservative treatment or other, non-surgical treatment option; (4) osteosynthesis performed as rescue following another previous treatment; (5) patients who did not agree to participate through informed consent or demise; (6) intervention or follow up carried out at a different centre.
The study was approved by the Autonomous Research Ethics Committee and each patient was reported and previously agreed to being included by means of an informed consent form.
All participants previously consented to have their data collected and used for the purposes of this study.
Surgical techniqueAll the individuals were operated on by 7 surgeons belonging to the same Orthopaedic Unit. The anaesthesia used for this process was general anaesthesia with endotracheal intubation combined with regional block of the brachial plexus.
Patients were placed semi-seated in the beach chair position, as it enables the extremity to be better managed and to facilitate the use of radioscopy. In all cases, the deltopectoral approach was chosen. After identifying the tuberosities and referencing them with sutures for subsequent re-anchoring, the fragments were reduced and the place was temporarily fixated with Kirschner wires. The plate was placed 5mm distal to the greater tuberosity to keep it from bumping into the greater tuberosity during abduction, and 2–4mm posterior to the lateral edge of the bicipital groove. The locking screws of the humeral head were implanted under radioscopic guidance. The distal portion of the plate was fixated with a primary bicortical screw, and the remaining screws were locked to the plate. Finally, the rotator cuff sutures were anchored under the plate.
At the end of the surgery, the length and proper placement of the screws and of the plate, the stability of the fracture and passive mobility of the shoulder were all once again verified under radioscopic control.
Following the intervention, the shoulder was immobilised with a sling for 3 weeks, which was removed several times per day to do exercises. Patients were instructed to do isometric exercises of the deltoids, biceps, and triceps, as well as pendular exercises 3 times per day starting on the day after the operation and larger passive movements starting at the second postoperative week. At 3 weeks, the sling was gradually removed and abandoned entirely between the fourth and fifth postoperative weeks.
Postoperative evaluationPostoperative clinical and radiological evaluation was carried out at 2 weeks, 6 weeks, 3 months, 6 months, 2 years, and at the end of follow up.
The Constant-Murley Shoulder score, Quick Disabilities of the Arm, Shoulder and Hand score (Quick DASH), and EuroQol-5D (EQ-5D) functional scales were used, as well as simple anteroposterior (AP) and axial projections of the shoulder. The Constant-Murley Shoulder scale score factors in 4 parameters: pain, activities of daily living, joint equilibrium, and strength. This last parameter was measured by means of a series of calibrated weights, that gradually increased, and the measurement was obtained from the weight that the patient was able to hold for 5s, 3 consecutive times.
During the interview at the end of the 2-year follow-up period, an objective assessment of the range of motion of the shoulder was performed using the Younext 4D Motion Capture system of movement analysis, which is capable of measuring movement in the 3 axes of space (height, width, and depth), adding time as the fourth dimension.
Study methodology of the shoulder with the Younext 4D systemA tracking system without markers was used that recognises the patient's natural movement and translates it into data that make it possible to recreate a 3D rendering of said movement. The analysis of the movement of the shoulder is performed by means of a 4D capture that enables us to ascertain the coordinates and relative positions of the points of reference of the upper extremities.
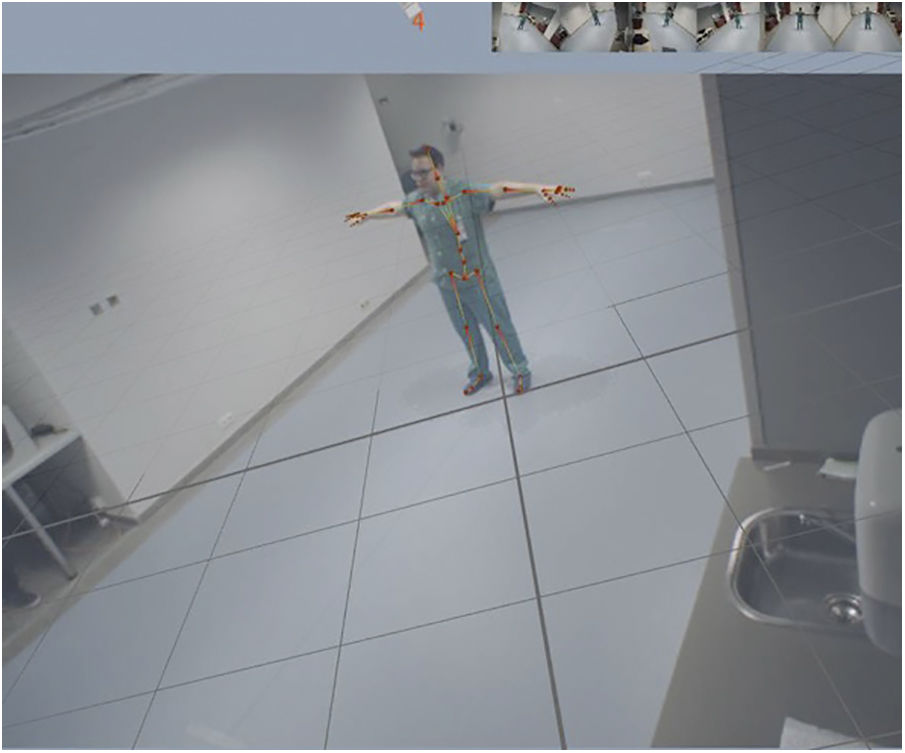
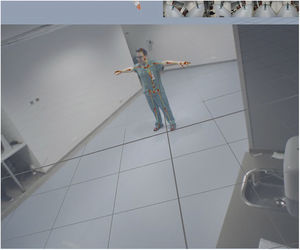
The system is installed in a well-lit 8×4×2.5m room/action area, consisting of a matte linoleum floor to prevent shine that interferes with the recording, and 6 PS Eye cameras arranged in such a way as to obtain 3 viewing angles in the frontal area of the person and 3 viewing angles of the posterior areas, as shown in Fig. 1.
The software in charge of capturing the images is the iPi Recorder. This program pools real-time viewing from all of the cameras installed on a single screen and distinguishes between the background with respect to the person being studied. The study subject should wear properly fitting clothing that contrasts with the floor; in this case, a short-sleeved black tee shirt. Fig. 2 shows an example of the capture obtained using a standard body type.
The starting reference points for the study are established on the patient, placed in the centre of the space assigned for this purpose with their arms extended in the form of a cross.
Simple movements in flexion, extension, abduction, adduction, and rotations of the shoulder were initially performed in order to analyse the range of motion. Exercises related with the activities of daily living were then performed: touching their contralateral ear passing their arm over their head, washing their axilla, simulating removing their bra, personal hygiene, bringing food to their mouth, and combing their hair. Each movement was performed separately and had a starting point and an ending point: the patient was standing upright, with arms relaxed at their sides. Both arms, the one that had undergone surgery and the healthy one, were analysed separately.
After filming the movement, the file was imported into the iPi Mocap Studio software programme, which recognises the body's anatomical position and creates a virtual image or avatar that reproduces the patient's movements.
The generated file was then processed by the Bioviewer programme, which externalises the parameters enabling the movements made to be analysed and contrasted. The system is capable of measuring the angles, lengths, ranges of motion, speeds, and accelerations in all the joints. The final report obtained contains comparative numerical and graphic data regarding movement in flexo-extension, adduction, abduction, and rotations of the shoulder. In addition, a summary table is obtained that displays the range, angles, speed, and acceleration of the movements studied.
Statistical analysisPearson's correlation was used to assess the existence of a statistically significant relation between the different scales applied, with a 95% confidence interval. The data were processed using the SPSS version 22.0 (SPSS Inc., Chicago, IL, USA) statistical software package.
ResultsOf the 156 patients who underwent surgery during the time period indicated, 47 met the inclusion criteria and agreed to be interviewed for a clinical evaluation 2 years following surgery and were finally eligible for admission into the study.
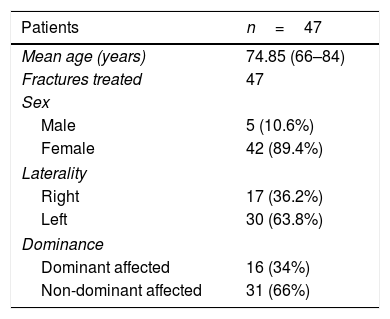
The sample's demographic characteristics are displayed in Table 1.
The aetiology of the fracture was an accidental fall with low energy trauma in the 100% of the cases.
The mean follow up was 4.69 years, with a range of between 2.49 and 7.14 years.
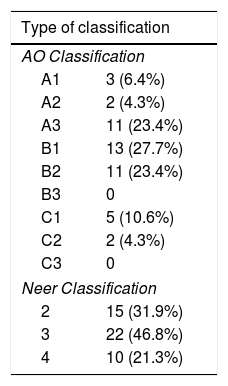
The type of fracture according to AO and Neer classifications are recorded in Table 2. In our study, the most common ones were 3-part fractures.
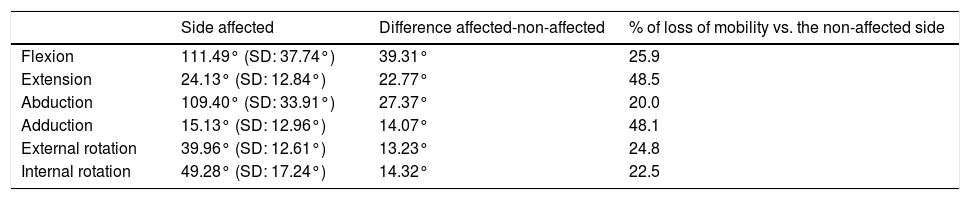
The mean values of the clinical evaluations at the end of the follow-up period were 70.06 points on the Constant-Murley scale (range: 38–97), 35.74 on the Quick DASH (range: 2.2–77.3), and 6.79 on the EQ-5D (range: 0–10). The mean ranges of motion (in flexion, extension, abduction, adduction, internal rotation, and external rotation) of the side affected by the fracture and the mean values of the differential between the arm affected and the healthy arm can be consulted in Table 3.
Range of displacement measured by motion capture.
| Side affected | Difference affected-non-affected | % of loss of mobility vs. the non-affected side | |
|---|---|---|---|
| Flexion | 111.49° (SD: 37.74°) | 39.31° | 25.9 |
| Extension | 24.13° (SD: 12.84°) | 22.77° | 48.5 |
| Abduction | 109.40° (SD: 33.91°) | 27.37° | 20.0 |
| Adduction | 15.13° (SD: 12.96°) | 14.07° | 48.1 |
| External rotation | 39.96° (SD: 12.61°) | 13.23° | 24.8 |
| Internal rotation | 49.28° (SD: 17.24°) | 14.32° | 22.5 |
SD indicates the standard deviation calculated.
When analysing the Constant-Murley score and the EQ-5D, a positive moderate correlation was obtained (R=.488 and p<.000); the relation between the Quick DASH and the EQ-5D scales was likewise moderate, but in this case, it was negative (R=−.501 and p<.000), given the inverse scoring compared to the Constant-Murley scale. Likewise, the correlation between both functional scales was strong, significant statistically, and negative (R=−.729 and p<.000).
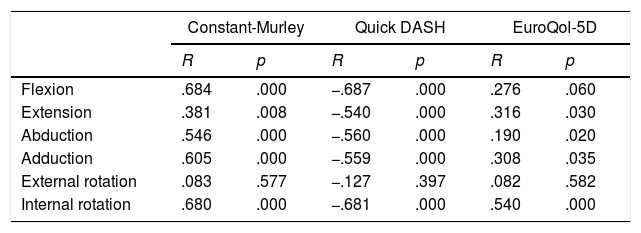
Table 4 presents the results of the analysis that was made to ascertain whether or not there was a correlation between the results obtained on the different scales and the ranges of motion determined by the motion capture.
List of results from motion capture with the Constant-Murley, Quick DASH, and EuroQol-5D scales.
| Constant-Murley | Quick DASH | EuroQol-5D | ||||
|---|---|---|---|---|---|---|
| R | p | R | p | R | p | |
| Flexion | .684 | .000 | −.687 | .000 | .276 | .060 |
| Extension | .381 | .008 | −.540 | .000 | .316 | .030 |
| Abduction | .546 | .000 | −.560 | .000 | .190 | .020 |
| Adduction | .605 | .000 | −.559 | .000 | .308 | .035 |
| External rotation | .083 | .577 | −.127 | .397 | .082 | .582 |
| Internal rotation | .680 | .000 | −.681 | .000 | .540 | .000 |
R represents the value of Pearson's correlation calculated and p, the value of statistical significance.
The results of the scale EQ-5D correlated positively with extension (R=.477 and p=.002) and adduction (R=.354 and p=.015) of the shoulder. There was a moderate negative, statistically significant correlation between the DASH scale and flexion, abduction, adduction, and internal rotation. Finally, there was a moderate positive, statistically significant correlation between the Constant-Murley score and flexion, extension, abduction and adduction.
DiscussionThere are any number of studies that offer the clinical results attained in the treatment of proximal humerus fractures in the elderly, but no clear consensus exists as to what the best treatment option is.13,14 In addition to those that collect the functional results obtained from conservative treatment, by means of osteosynthesis with locking plate and, more specifically, with the Philos plate,15–19 recent works have evaluated the barrage of new options, such as total reverse arthroplasty of the shoulder, as an alternative to osteosynthesis with a plate or to hemiarthroplasty.20 These results are particularly relevant given that the postoperative outcomes may the activities of daily living. To analyse this issue, several different, patient- or evaluator-rated functional scales have been used; similarly, quality of life scales to appraise how the fracture affects patient in general and do not focus solely on the functionality of the limb by itself.21 All of these scales exhibit a certain component of subjetivity,9,10 especially the Constant-Murley Shoulder scale; strength can be overestimated in elderly patients.
Motion capture has been used to evaluate the shoulder to quantify the range of motion of the joint in healthy individuals22,23 and in different pathologies that can affect the glenohumeral joint, such as a tear of the rotator cuff24,25 or joint disease secondary to such a tear treated by means of a reverse arthroplasty of the shoulder.12 These studies conduct kinematic analysis using methods that entail the use of real-time radioscopy22,24 or markers12 by means of optoelectronic motion capture systems that make use of multiple, high-speed cameras that send infrarred light signals to capture the reflections from passive markers placed on the body or transmit movement data from active markers that contain infrarred-emitting diodes. Our work offers a double innovation: this methodology is used for the first time to assess outcomes following osteosynthesis of humeral head fractures and movement is analysed in four dimensions with cameras without the need for markers or X-ray, thereby preventing exposure to radiation and avoiding dependence on markers placed on the patient that make examination more uncomfortable.7 Although the Younext 4D method (3D reconstructions of movement over time) has been used in other joints, we can state that its application in this type of injury is original and of great usefulness.
The results in our series have not differed significantly with respect to the production mechanism or demographic characteristics of the sample; nor have the functional parameters, in particular the Constant-Murley scale, or regarding quality of life, in comparison with other series in the literature.26,27
The results obtained reveal a correlation between the different functional scales and with the quality-of-life scale, which demonstrates that the use of these scales is appropriate to evaluate functionality in these patients, as verified in other studies.28,29
On analysis of the functional results obtained by means of motion capture, we see that flexion and abduction movements were the ones for which the affected arm displayed greater loss of degrees of mobility versus the unaffected arm. These data also coincide with those published in other works in which measurement was performed manually.26,30
The range of motion following surgery, both in flexion and in abduction, made it possible for the arm to be moved over the top of the head, with abduction and rotations being the movements that were least affected. In contrast, extension and adduction were decrease by close to 50% in the affected arm in comparison with the healthy arm. In our study, the mean score on the EQ-5D scale was 6.79 points, which would indicate that the loss of mobility in these 2 ranges does not have very noticeable repercussions on patients’ quality of life and that, nonetheless, satisfactory functionality can be achieved. We have seen that if values exceeding 90° of flexion and abduction are achieved, and acceptable rotations are likewise attained, our patients’ quality of life was not significantly affected. These data are in line with the quality-of-life results obtained in other similar studies.21
Finally, the correlation between the objective measurement obtained by means of motion capture and the different functional scales was analysed. Said correlation was seen to exist for all the movements scrutinized, except for external rotation, with the Quick DASH and Constant-Murley scales. These data indicate that motion capture represents the results obtained objectively and can be a highly useful tool. The absence of correlation with external rotation could be due to the fact that loss in this type of movement has less of a functional impact on specific aspects that are examined by these scales. Correlation of motion capture with the quality-of-life scale was likewise good, with the exception of external rotation and flexion. This implies that, after achieving mean flexion of 90° and sufficient external rotation, the limitations in these movements does not affect these patients’ quality of life.
The limitations of the study include its retrospective nature and the small sample size. There are no similar studies with this same motion capture technology with which to compare; as a result, the results must be interpreted with caution. The 2-year follow-up does not allow for long-term outcomes to be evaluated — a timeframe in which the appearance of osteoarthritic phenomena could limit functionality even further, especially joint deterioration, which could translate as a worsening of the scores on the scales.
ConclusionsOsteosynthesis with locking plate in proximal humerus fractures in the elderly achieves good functional results and quality of life. Motion capture is an emerging tool that makes it possible to obtain objective measurements when assessing outcomes in these patients and correlate appropriately with the functional scales typically used, as well as with quality-of-life scales. We believe that it is an alternative that enables better interindividual comparisons to be made, given its objectiveness, and can contribute to shed greater light about functional results in proximal humerus fractures, as well as to appraise other musculoskeletal diseases.
Level of evidenceLevel of evidence IV.
Conflict of interestsNone declared.
Please cite this article as: Gómez-Blasco AM, Hernández-Fernández A, Roche-Albero A, Martín-Hernández C. Resultados medidos con captura de movimiento en las fracturas de húmero proximal tratadas mediante osteosíntesis con placa bloqueada. Rev Esp Cir Ortop Traumatol. 2019;63:268–274.