Superior labral anterior to posterior (SLAP) injuries are widely recognized as a cause of pain and dysfunction in the shoulders of active patients. The aims of the present study were to analyze SLAP injuries in the workplace, and to evaluate the reliability of physical examination and imaging techniques for the diagnosis of work-related SLAP injuries.
Material and methodsRetrospective chart review of 58 SLAP injuries treated in our occupational health centre from 2005 to 2015 in 815 patients undergoing shoulder arthroscopy. Data were collected on mechanism of injury, clinical proceedings, complementary tests (contrasting the initial magnetic resonance imaging report with that of a radiologist specializing in musculoskeletal pathology), arthroscopy findings and treatments performed.
ResultsThe most common mechanism of injury was acute injury while handling weight, in the majority of cases, above the head. SLAP injury was suspected in 41% of cases through anamnesis and physical exam, in 29% through the initial magnetic resonance imaging report, and in 52% through the specialized radiologist's report. In 78%, associated injuries were present, the most common being rotator cuff injuries.
ConclusionsSLAP injuries in the workplace are rare and are often a diagnostic finding during surgical intervention performed for a different associated injury. Arthro-magnetic resonance imaging and magnetic resonance imaging have lower reliability than physical exams in the diagnosis of work-related SLAP injuries. A radiologist specializing in musculoskeletal pathology could probably improve the reliability of imaging test interpretation in work-related SLAP injuries.
La lesión del labrum superior anteroposterior (SLAP) es una conocida causa de dolor y disfunción del hombro en pacientes activos. El objetivo fue estudiar las lesiones de SLAP en población laboral y valorar la fiabilidad de la exploración física y las técnicas de imagen en el diagnóstico de las lesiones de SLAP en el entorno laboral.
Material y métodosRevisión retrospectiva de 58 lesiones de SLAP tratadas en nuestra mutua laboral desde 2005 hasta 2015 en 815 pacientes en los que se realizó una artroscopia de hombro. Se han recogido datos del mecanismo lesional, datos clínicos, pruebas complementarias (comparando el informe radiológico inicial con el de un radiólogo especializado en musculoesquelético), hallazgos artroscópicos y tratamiento realizado.
ResultadosEl mecanismo lesional más frecuente ha sido la lesión aguda levantando peso, en la mayoría de casos, por encima de la cabeza. La lesión de SLAP se sospechó en el 41% con anamnesis y exploración física, en el 29% de los informes radiológicos iniciales y en el 52% en los informes del radiólogo especialista en musculoesquelético. Presentaron lesiones asociadas el 78%, la mayoría lesiones del manguito rotador.
ConclusiónLa lesión de SLAP en el entorno laboral es infrecuente y muchas veces se diagnostica durante una artroscopia realizada por otra lesión. La artrorresonancia magnética y la resonancia magnética tienen menos fiabilidad que la evaluación clínica para su diagnóstico. Un radiólogo especializado en musculoesquelético podría mejorar la rentabilidad de las pruebas de imagen en el diagnóstico de estas lesiones.
Superior labral anterior to posterior (SLAP) injury has been described as the cause of pain and dysfunction in the shoulder in active patients.1,2 Snyder et al.2 described the pathological complex that form the superior labral and long head of the biceps (LHB) and coined the term “SLAP injuries”, classifying them in accordance with their arthroscopic features into 4 Types (i–iv).
There is surprisingly little information in the literature on SLAP injuries in manual labourers or the workplace. The SLAP injury is extensively described and reviewed in athletes whose sport involves throwing (external abduction and rotation). In these cases this is due to the repetition micro trauma produced by the peel-back mechanism of the LHB over the labrum.3 Apart from the peel-back mechanism in athlete throwers SLAP injuries have been described by repetitive movements above the shoulder, by direct trauma, injury by traction and injury by compression with the arm in flexion and abduction or even injuries which are not associated with any clear mechanism.4,5
Clinical diagnosis is difficult due to variable and non specific clinical presentation.4,5 The characteristic pain of the SLAP injury is usually a pain in the anterior surface of the shoulder, in the bicipital groove and in shoulder movements above the head.2 Several manoeuvres and exploratory tests have been described for SLAP injuries and LHB lesions: Speed test,6 Yergason manoeuvres,6 O’Brien test,6,7 Meyers test,6 etc. However, analysis by independent observers of these tests has revealed inconsistent results and has not provided any secure diagnosis.4 The frequent lesions associated with a SLAP injury make diagnosis even more compex.6,8
Magnetic resonance imaging (MRI) and arthro-MRI are the most widely accepted additional tests for the diagnosis of a SLAP lesión,9,10 but sensitivity and specificity rates both for MRI and arthro-MRI are highly varied in values in the multiple studies undertaken, with some consensus in considering arthro-MRI superior to MRI for SLAP lesion diagnosis.9–11 On many occasions diagnosis was made using arthroscopy,4 but even so it has to be carefully interpreted, bearing in mind possible anatomical variants of the labrum, and also to be interpreted together with clinical history, physical examination and imaging test findings, as major intra and interobservant differences have been described in the diagnosis of these lesions by arthroscopy.12–14 No consensus has been reached regarding the treatment of SLAP injuries, particularly in elderly patients and in type II lesions of the Snyder classification.2,15 The choice of treatment method would depend on the type of lesion, the patient and concomitant lesions.16
The main objective of this study was to study SLAP lesions in a working population and assess the reliability of physical examination and the imaging techniques in the diagnosis of SLAP lesions in the workplace.
Material and methodRetrospective review of SLAP lesion patients who underwent surgery in our occupational health centre from 2005 to 2015. The surgical reports of the 815 patients who received arthroscopy of the shoulder during this period of 11 years were reviewed. Fifty eight SLAP injuries were diagnosed and treated (in 56 patients), confirmed by arthroscopy. Therefore all the patients were attended in an occupational health centre and their injuries were considered as accidents at work or occupational health conditions.
The medical histories were reviewed, from which epidemiological data were extracted: age at the time of surgery, sex, dominant hand, affected limb and medical history of relevance or other interventions and type of injury mechanism. Data relating to physical examination (whether a SLAP lesion was suspected or not) were obtained and the additional tests carried out (anamnesis and physical examination were undertaken in all cases by the same senior surgeon). The surgeon systematically gave a complete physical examination to all patients who had presented with shoulder pain and this included, among other manoeuvres for assessing other possible lesions, the speed test, the Yergason manoeuvre and the O’Brien test. The time interval was also calculated from when the patient suffered from the injury until they were operated on and the sick leave period. The medical findings in the arthroscopy were obtained from the surgical reports for the type of SLAP lesion and for the associated lesions and treatment carried out.
The images and reports directly available from the MRI and arthro-MRI were analyzed (with contrast intra-articular injection). Magnetic resonance equipment of 1.5T was available for the imaging studies in the 3 centres where the tests were performed. The MRI imaging of the original tests were reassessed (with the same information that was made available to the radiologist who evaluated the test initially), by a radiologist specializing in musculoskeletal diseases who currently works in our hospital (a different person from the radiologists who reported on the tests originally made) and who at the time of reviewing the images was not aware of the study that was being carried out. The most commonly used sequences by the specialist radiologist for assessing the SLAP injury were axial PDFS sequences (proton density with fat saturation) and T2 FS (fat saturation) coronal sequence.
Forty patients were reassessed out of those who had complete imaging studies. In the other 18 cases the imaging study had been carried out by an external company and the radiologist did not have the complete original study but had an edited version which could have biased interpretation. For this reason, only the 40 studies which could be handled in equal conditions by the radiologist who initially assessed them were reassessed and the MRI reports were compared by the 2 radiologists.
All the patients were operated on by the same senior surgeon (ESA) under general and local anaesthesia using an interscalene block, with the patients lying on their side with traction of 4.5kg, initially using a standard posterior portal for systematic arthroscopic examination and anterior and anterolateral work portals, with one optional osterolateral portal for the treatment of posterosuperior lesions. The SLAP lesions were treated at the surgeon's discretion using debridement or suture with labral anchorage, or tenotomy or tenodesis of the tendon of the LHB, in addition to treatment of the associated lesions when necessary. In our opinion the first choice of treatment in actively employed patients is the repair of the labrum (one or two anterior anchorages in anterior SLAP II, one or 2 posterior in posterior SLAP II and one anterior and another posterior in anterior and posterior SLAP). When the biceps tendon is also injured tenodesis is undertaken (fixation using interferential subpectoral extra-articular screws and only in patients with low functional demand, who are older and have other associated lesions is tenotomy an option.
Data processing was performed confidentially and respecting the anonymity of the patients, collecting data in a base created by the Microsoft Excel 2010 programme. Statistical analysis was made with the help of the IBM SPSS Statistics 22 programme. This consisted of a descriptive analysis of variables, calculating the distribution of frequencies for qualitative variables and the arithmetic mean and standard error of the mean for quantitative variables. To estimate the interobserver concordance between the radiologists who initially reported on the MRI and the 2nd radiologist the Kappa (κ) correlation coefficient was used where 0: poor concordance; .01–.2: slight concordance; .21–.40: acceptable concordance; .41–.60: moderate concordance; .61–.80: considerable concordance; .81–1: almost perfect concordance.17
For this type of retrospective study approval from the ethics committee was not required. Informed consent from each patient was obtained prior to the surgical intervention and included the use of data for educational or research purposes.
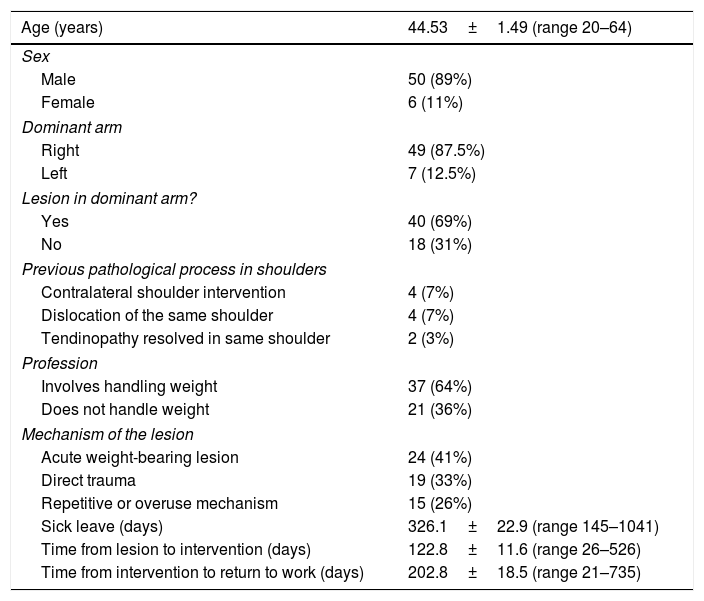
ResultsWe reviewed the surgical reports of 815 arthroscopies of the shoulder from 2005 to 2015 which were carried out in our service, finding 58 SLAP lesions (in 56 patients) confirmed by arthroscopy during this period of 11 years. This comprises a percentage of 7.12% in the total shoulder arthroscopies performed. Epidemiological data are shown in Table 1. In all patients the initial reasons for the consultation was pain in the shoulder during active employment. The most common mechanism was acute injury to the shoulder whilst carrying out an activity handling weight in the arms, in the majority of cases, above the head (41%), followed by direct trauma (33%); in a third patient group the precise mechanism could not be objectified but during their regular employment activity they carried out a repetitive activities with over-use of the shoulder, which could explain the lesion (26%). After anamnesis and a physical examination a SLAP lesion was suspected in 24 cases (41%), whilst in 34 cases (59%) there was no clinical suspicion of this, but surgical intervention proceeded with other suspected diagnoses (in the majority of cases partial or complete rupture of one or several rotator cuff tendons). In these 34 cases the SLAP lesion diagnosis was made during arthroscopic examination.
Epidemiological data, lesion mechanisms and duration times.
| Age (years) | 44.53±1.49 (range 20–64) |
|---|---|
| Sex | |
| Male | 50 (89%) |
| Female | 6 (11%) |
| Dominant arm | |
| Right | 49 (87.5%) |
| Left | 7 (12.5%) |
| Lesion in dominant arm? | |
| Yes | 40 (69%) |
| No | 18 (31%) |
| Previous pathological process in shoulders | |
| Contralateral shoulder intervention | 4 (7%) |
| Dislocation of the same shoulder | 4 (7%) |
| Tendinopathy resolved in same shoulder | 2 (3%) |
| Profession | |
| Involves handling weight | 37 (64%) |
| Does not handle weight | 21 (36%) |
| Mechanism of the lesion | |
| Acute weight-bearing lesion | 24 (41%) |
| Direct trauma | 19 (33%) |
| Repetitive or overuse mechanism | 15 (26%) |
| Sick leave (days) | 326.1±22.9 (range 145–1041) |
| Time from lesion to intervention (days) | 122.8±11.6 (range 26–526) |
| Time from intervention to return to work (days) | 202.8±18.5 (range 21–735) |
Data are expressed as a mean±EEM.
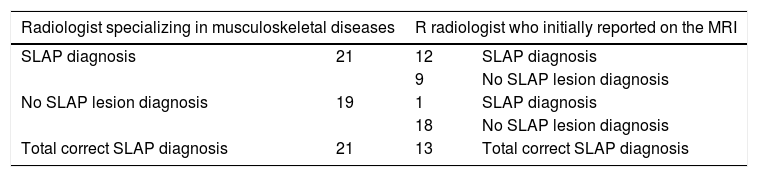
All patients had an MRI, with a radiologist's report who had access to the patient's medical record. In 41 cases (71%) the radiologist did not suspect a SLAP lesion and in 17 he or she did (29%). In all patients with a suspected SLAP lesion by MRI this type of lesion had already been suspected during their visit to the orthopaedic surgeon from medical features and examination. In 7 cases where the orthopaedic surgeon suspected a SLAP lesion there were no apparent events suggestive of the SLAP lesion in the MRI. Arthro-MRI was used to complete the study prior to intervention in 13 patients (22%) in keeping with the surgeon's criterion. In 7 cases SLAP lesion was suspected (54%) and in 6 it was not (46%). In the 7 cases where the lesion was suspected in the arthro-MRI it had also been suspected clinically and with the MRI. In 5 of the 6 cases in which there was no report of the SLAP lesion in the arthro-MRI there had been clinical suspicion of it. In the reassessment of the 40 MRI available to the radiologist specializing in musculoskeletal disease the SLAP lesion was suspected in 21 cases (52%). Table 2 contains the results when comparing the MRI reports of the radiologist specializing in musculoskeletal disease with those of the radiologist who initially made a report on the study. The interobserver correlation coefficient is κ=.51, which is a moderate concordance between both radiologists.17
Comparison between the radiologist specializing in musculoskeletal diseases and the radiologist who initially reported on the MRI.
| Radiologist specializing in musculoskeletal diseases | R radiologist who initially reported on the MRI | ||
|---|---|---|---|
| SLAP diagnosis | 21 | 12 | SLAP diagnosis |
| 9 | No SLAP lesion diagnosis | ||
| No SLAP lesion diagnosis | 19 | 1 | SLAP diagnosis |
| 18 | No SLAP lesion diagnosis | ||
| Total correct SLAP diagnosis | 21 | 13 | Total correct SLAP diagnosis |
κ=.51 moderate concordance.
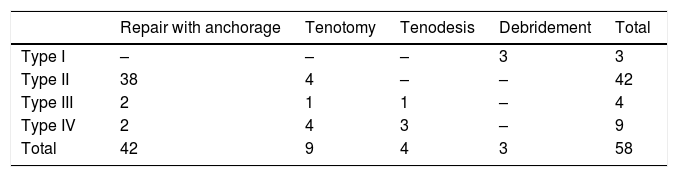
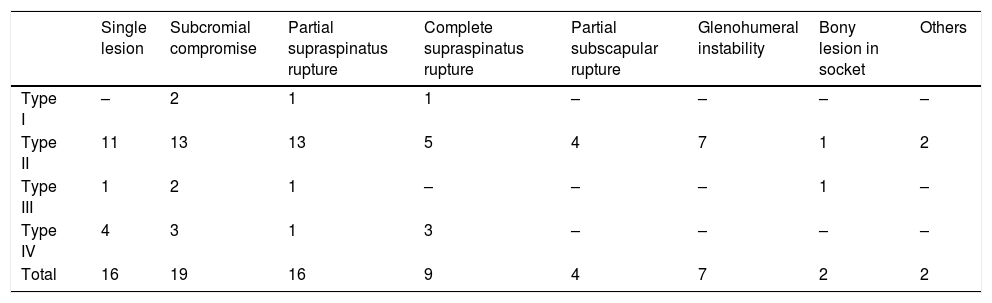
Table 3 shows the classification of the SLAP lesions in accordance with the arthroscopic findings, and the treatment undertaken. Only in 16 patients (28%) was the SLAP lesion found as a single lesion, in 19 patients (32%) there were signs of subacromial compromise, in 16 cases (28%) of partial rupture of the supraspinatus tendon, in 9 patients (16%) complete rupture of the supraspinatus tendon, in 4 patients (7%) partial rupture of the subscapular tendon, in 7 cases (12%) anterior inferior or posterior labral lesion with glenohumeral instability, in 2 patients (3%) bone lesions in the socket, in one case acromion clavicular arthrosis and in another case lesion of the middle glenohumeral ligament. Table 4 shows the lesions associated with the type of SLAP lesion.
Type of SLAP lesion and associated lesions (there are some patients with more than one associated lesions).
| Single lesion | Subcromial compromise | Partial supraspinatus rupture | Complete supraspinatus rupture | Partial subscapular rupture | Glenohumeral instability | Bony lesion in socket | Others | |
|---|---|---|---|---|---|---|---|---|
| Type I | – | 2 | 1 | 1 | – | – | – | – |
| Type II | 11 | 13 | 13 | 5 | 4 | 7 | 1 | 2 |
| Type III | 1 | 2 | 1 | – | – | – | 1 | – |
| Type IV | 4 | 3 | 1 | 3 | – | – | – | – |
| Total | 16 | 19 | 16 | 9 | 4 | 7 | 2 | 2 |
This retrospective study analyzed SLAP injuries in the workplace (occupational therapy patients) and the reliability of anamnesis, physical examination and imaging techniques for SLAP injury diagnosis in the working population.
Although SLAP lesions are widely recognized as the cause of pain and dysfunction in the shoulder of active patients,1,2 their rate of occurrence is low in the different published studies, ranging between 3% and 26%.1,2,5,18,19 Numerous series have been published on sportspeople,1,19,20 the military5,21 and also the population in general,8,22 but to our knowledge there has only been one published study on the workforce population.23 In our series the incidence rate was 7.12% out of the total shoulder arthroscopies performed, which is comparable to other epidemiological studies published on SLAP injuries in the general population (6–9%)8,22 and in elite sportspeople whose sport involves throwing mechanisms (6–12%),1,19,20 but it is lower in comparison to epidemiological studies in the military (25–37%).5,21
The mean age of the patients of our series was 44, which is within the range described in the literature for general population5,18,24 series and in particular in a workplace,23 but higher than the mean age of some series described by elite sportspeople or the military.20,25 Similarly to the majority of studies published on SLAP lesions,8,23,26,27 in our series there was a clear predominance of lesion in males (90%) and in the dominant limb (69%).
The most common mechanism of SLAP injury described in the literature is repetitive microtrauma from traction of the biceps tendon on the labrum (peel-back mechanisms)3 in sportspeople using throwing mechanisms. In contrast, other studies1,19 reported the most common mechanism as the direct trauma from a fall with the arm extended. In our study the most common mechanism was acute injury in the shoulder whilst carrying out an activity handling weight with the arms, in most cases, above the head (biomechanically a similar mechanism to that involved in sportspeople throwing), followed by direct trauma.
According to that described in the literature the most common lesions are type ii, with a low frequency of type iii and iv lesions.1,5,8 Similarly to that reported by other authors, in our series the most common type of lesion was type ii (72%), but a high frequency of type iv (16%) stood out, compared with other series which describe an incidence of 5–10%.5,8
In our series there was a low rate of clinical suspicion in the diagnosis of the SLAP lesion (41%). This is probably influenced by the high rate of associated lesions which present, which obscure or hide the medical symptoms of SLAP. In our study MRI was less diagnostically efficacious than physical examination (29% of suspected cases), and in all patients where there was a suspected SLAP lesion from the MRI this had already been suspected in the visit to the orthopaedic surgeon by anamnesis and physical examination. 100% of the patients for whom the arthro-MRI had a suspected SLAP lesion result, there had also been clinical suspicion and in the MRI and therefore we did not obtain any further suspected diagnosis. Furthermore, in 83% of cases of SLAP lesion being confirmed by arthroscopy where the arthro-MRI was negative for the SLAP lesion, this lesion was suspected in the physical examination. As a result, in our series the arthro-MRI did not add anything to the SLAP lesion diagnosis, and it also entailed a greater risk of complications for the patient as it was an invasive test,27 compared to what was described in other studies where greater rates of sensitivity and specificity were observed undertaking an arthro-MRI with contrast intra-articular injection.9,28 However, if the MRI images are assessed by a radiologist specializing in musculoskeletal disease, in our series the rate of suspicion would have increased up to 52%, which improves clinical suspicion by 11% and the suspicion of the radiologist who initially reported on the imaging by 23%. The interobserver correlation coefficient is κ=.51, which suggests a moderate concordance between both the radiologists, and it is therefore important to know which radiologist is assessing the study made and to be aware whether the variability could be relatively high. Therefore, our study suggests that a radiologist who is specialized in musculoskeletal disuse could improve the efficiency of the imaging studies in the case of SLAP lesions.
A repair of the SLAP lesion was made in 72% of cases, and in 90% of cases if we only take into account type II lesions (Table 3). This high percentage of SLAP lesion repair as opposed to the use of tenotomy or tenodesis is in keeping with the tendency described in the literature for the years when the procedures were undertaken.24,29 Although some studies suggest that in patients over 35 results are better with tenodesis26 we believe like other authors25 that in patients with high functional demand and when there are also associated lesions good results are obtained with repair, at least in the workplace.
The incidence of lesions associated with SLAP lesions in arthroscopic findings described in the literature is very high (69–90%),5,8,18,20,25 which coincides with that observed in our series (72%). This, together with the low rate of clinical suspicion and radiography, suggests that to a large extent the patients with SLAP lesions have been diagnosed incidentally when other lesions have been treated, which were the principal diagnosis for which they were operated on.29 As a result, a shoulder surgeon should be technically prepared to resolve a SLAP lesion and should have the necessary tools, material and implants available to treat it when performing a shoulder arthroscopy for any other reason.
In order to typify the lesions the Snyder et al.2 classification was used. The classifications described by Maffet et al.19 and Powell et al.30 offer a detailed anatomical description of the lesion, with different subtypes but due to their complexity and lower use of the same in regular clinical practice the surgeon performed the operations using the Snyder et al. classification.2
This study has its own limitations as a retrospective study, especially regarding data collection (there was no standardized clinical evaluation), and there was a relatively small sample distributed over a long period of time, with the consequent variations in diagnosis and treatment following the technological evolution of the specialty (regarding imaging studies, implants, etc.). In future prospective studies the criteria should be clearly defined for the diagnosis of the SLAP lesion, with a clearly defined protocol of physical examination, request for further studies (MRI, arthro-MRI or both) with an appropriate control group and with a sample large enough to offer more solid, valid data.
ConclusionsSLAP lesions in the workplace are rare and are usually the result of a diagnostic finding during arthroscopy of the shoulder performed for another lesion. Anamnesis and physical examination, direct arthro-MRI and magnetic resonance are reliable tools for the diagnosis of SLAP lesions. A radiologist specialized in musculoskeletal disease could take better advantage of the imaging studies in SLAP lesions in the workplace.
Level of evidenceLevel of evidence iv.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Navío-Fernández F, Miranda I, Sánchez-Alepuz E, Shahin M, Pastor-Fernández E, Carratalá V, et al. Lesión del labrum superior anteroposterior (SLAP) en el entorno laboral. Rev Esp Cir Ortop Traumatol. 2019;63:261–267.