To analyze the results of treatment of scaphoid nonunion with questionable viability of the proximal fragment, but without significant deformity or collapse, using a vascularized bone graft of 1,2 intercompartmental supraretinacular artery (1,2 ICSRA) and subsequent osteosynthesis.
Materials and methodsA retrospective study was performed on 10 male patients with a radiographic diagnosis of nonunion. Functionality, pain using Visual Analog Score (VAS), grip strength, patient satisfaction and reintroduction to working life, using QuickDASH and may specific wrist scales were assessed after the treatment. The integration of the graft was checked by radiography.
ResultsThe mean follow-up was 31.4 months, and 90% of the questionnaires were satisfactory. The VAS decreased by 4.6 points and the flexor-extensor mobility gain was 5°. The total graft consolidation rate reached 40% in 5.5 months on average.
DiscussionSeveral studies have demonstrated better results using vascularized bone graft versus non-vascularized. From the description by Zaidemberg in 1991, the vascularized graft with 1,2 ICSRA artery, distal radius, has been the most widely used for the treatment of scaphoid nonunion.
ConclusionsOur results are comparable with the literature reviewed; thus using vascular graft of the 1,2 ICSRA and osteosynthesis with Herbert-type screw may be an alternative treatment for proximal scaphoid nonunion, without collapse or significant deformity.
Estudiar los resultados del tratamiento de la seudoartrosis de escafoides, con dudosa viabilidad del fragmento proximal, pero sin deformidad ni colapso importante del mismo, mediante la utilización de un injerto óseo vascularizado de la arteria suprarretinacular 1,2 intercompartimental (1,2 ICSRA) y osteosíntesis posterior.
Material y métodoEstudio retrospectivo de 10 pacientes varones con diagnóstico radiográfico de seudoartrosis. Después del tratamiento se evaluó la funcionalidad, el dolor medido por la escala analógica visual (EVA), la fuerza de agarre, la satisfacción del paciente y la reintroducción a la vida laboral, utilizando las escalas de Mayo y QuickDASH específicas de muñeca y comprobándose radiográficamente la integración del injerto.
ResultadosEl seguimiento medio fue de 31,4 meses; un 90% de las encuestas fueron satisfactorias. La EVA descendió en 4,6 puntos y la ganancia de movilidad flexo-extensora fue de 5°. La tasa de consolidación completa del injerto alcanzó el 40% en 5,5 meses de media.
DiscusiónDiferentes estudios han demostrado mejores resultados utilizando injerto óseo vascularizado frente al no vascularizado. Desde la descripción por Zaidemberg en 1991, el injerto microvascularizado con arteria 1,2 ICSRA, de radio distal, ha sido el más utilizado para el tratamiento de seudoartrosis del escafoides.
ConclusionesNuestros resultados, comparables con la bibliografía revisada, utilizando el injerto vascularizado de arteria 1,2 ICSRA y osteosíntesis con tornillo tipo Herbert, pueden ser una alternativa de tratamiento para la seudoartrosis proximal de escafoides, sin colapso ni deformidad importante.
Fractures of the scaphoid bone are the most frequent ones of the carpal bones.1,2 The high incidence of appearance of pseudarthrosis represents a problem for choosing the treatment for it.3–6 Given the prevalence in work environments and over age ranges in the first decades of work insertion, scaphoid pseudarthrosis has a major impact on the social and work life of the patients.7 Scaphoid pseudarthrosis can have implications for the development of degenerative changes in the wrist,8,9 beginning in the radioscaphoid joint and then affecting all the bones of the carpus.
Numerous techniques have been described and used to treat scaphoid pseudarthrosis.3–6 These range from the radial styloidectomy, resection of the proximal scaphoid fragment or proximal row of carpal bones; through interventions providing non-vascularized10–14 (Matti-Russe, Fernández, Stark, etc.) and vascularized grafts15–23 (Kawai, Zaidemberg, etc.), up to wrist arthrodesis. Recent studies have shown excellent results in shortening the time of bone consolidation using vascularized bone grafts.24–28 The literature includes transfers of vascular pedicle from the tubercle of the scaphoid itself, pisiforme,26 1st metacarpal27 or palmar and radialdorsus areas15 of the distal radius, achieving the consolidation of the union defect in 80% of the cases.24 Studies have also been published on vascularized grafts from other areas: cubital artery, iliac crest,24 and femoral condyle.24,28
The objective of our study was to study the results of the treatment of scaphoid pseudarthrosis with questionable viability of the proximal fragment, but without significant deformity or collapse (Herbert and Fisher classification type D1).29 To do so, we used a vascularized bone graft with the 1,2 intercompartmental supraretinacular artery (1,2 ICSRA)9–24 described by Zaidemberg plus osteosynthesis.
Materials and methodsWe reviewed 10 patients retrospectively (all male and with a mean age of 20.8 years) treated in our hospital complex between August 2008 and January 2012 with X-ray diagnosis of scaphoid pseudarthrosis, of more than 6 months of evolution without clinical or X-ray evidence of bone consolidation. The patients attended the consultation due to pain and functional limitation of the affected wrist. This corresponded to the dominant wrist in 6 patients. Their employment status included 2 students, 1 athlete and 7 manual workers, where the requirement for strength and agility in both wrists was high.
The mechanisms of lesion for the fractures were grouped into 6 chance falls, 2 sports accidents, 1 work accident, and 1 traffic accident. Two patients had a lesion associated to the fracture of the scaphoid (in 1 case, a trans-scaphoperilunar dislocation with fracture of the radius and, in the other, fracture of the triangular fibrocartilage). Initial treatment for the fracture of the scaphoid was orthopedic in half the cases, surgical (osteosynthesis with Kirschner wire) in 3, and another 2 patients did not receive any treatment at all.
Mean time from the injury to pseudarthrosis surgery with microvascularized graft was 22.3 months. Avascular necrosis of the scaphoid appeared in 6 of the cases (in 4 of them from preoperative MRI and in 2 during the surgical procedure), but 8 of the 10 patients studied lacked preoperative osteoarthritis.
After surgery we assessed aspects such as functionality, pain (VAS), strength of hold, and subjective satisfaction, as well as aspects of reintroduction to the patient's daily life and work. To do so, we used the scores on the QuickDASH and the Mayo wrist scales.30 In addition, graft integration was checked by X-ray. The results, obtained with simple X-ray image in specific projection for the scaphoid, were calculated measuring the pseudarthrosis distance before surgery, from the joint end of the capitate bone to the radial border, taking this measurement as the reference value. We used the computer program for X-ray images at our hospital (PACS version 2.2.1) to do so. After the surgery, with the same X-ray projection and using the same computer program, we measured the distance with that which the new bone formed covered the defect. Using a proportionality ratio, we calculated the percentage of graft consolidation, classifying it as complete, partial, and absence of consolidation for later study:
- •
Complete consolidation: the distance with which the new bone formed covered the defect was complete.
- •
Incomplete (partial) consolidation: the distance with which the new bone formed covered the defect was more than half (>50%).
- •
No consolidation: the distance with which the new bone formed covered the defect was less than half (<50%).
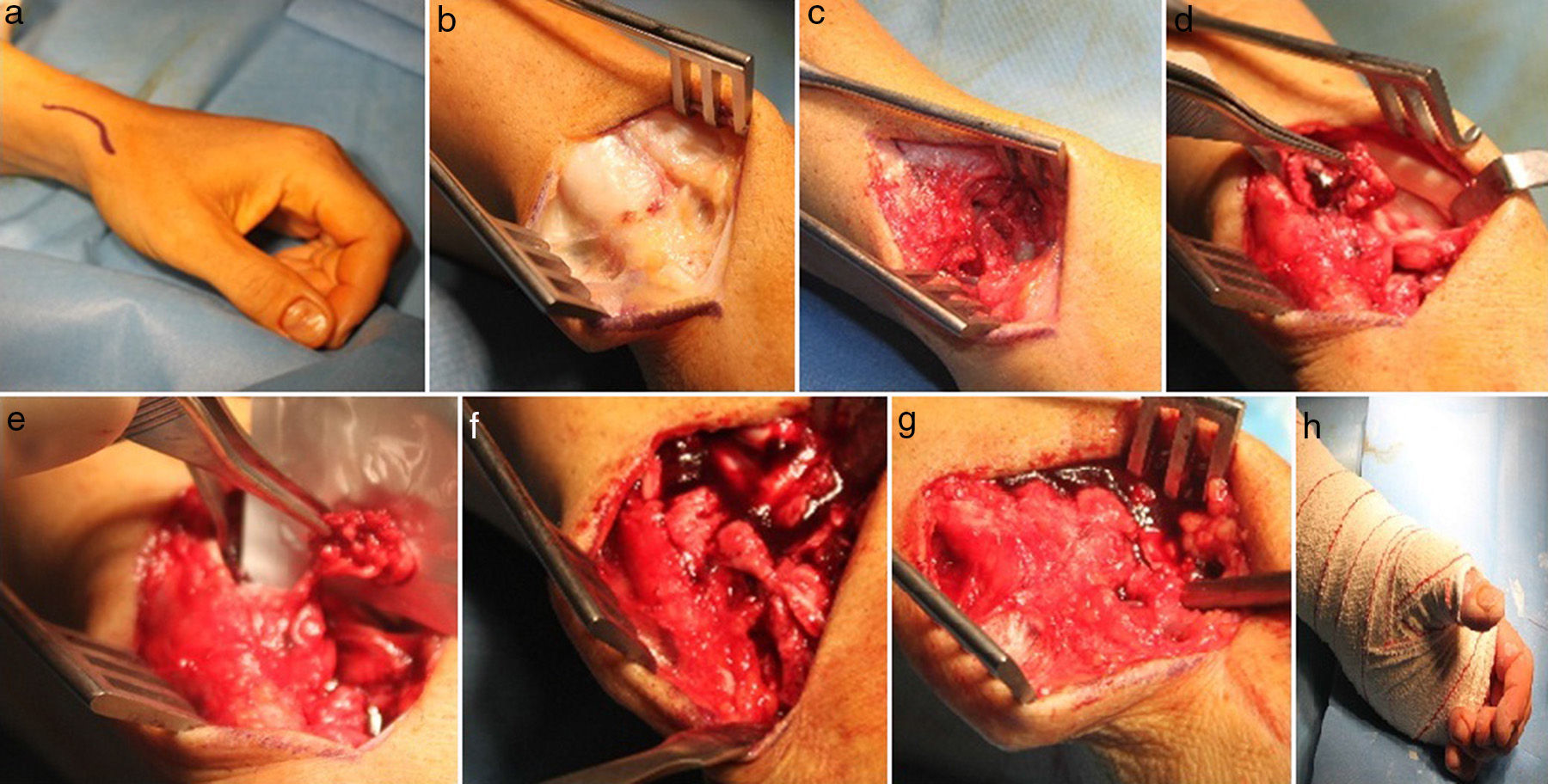
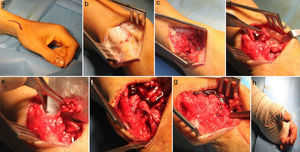
The scaphoid is subjected to a radial dorsal approach, providing safe, excellent scaphoid exposure. Its main disadvantages are the main branch of the radial nerve and possible effect on the dorsal irrigation of the scaphoid (Fig. 1).
Surgical technique for vascularized micrograft for the scaphoid. (a) Radial dorsum approach to the scaphoid in “Italic S”. (b) Exposure of the 2nd extensor compartment. (c) Pseudarthrosis area of the scaphoid. (d) Exposure of the bone graft donor area. (e) Microvascularized bone graft with the 1,2 intercompartmental supraretinacular artery (1,2 ICSRA). (f) Graft bleeding. (g) Fixation of the scaphoid pseudarthrosis. (h) Palmar splint with extension to the 1st finger for 6 weeks.
The patient is placed lying on the surgical table face upwards, with the arm extended over a supplementary table. The forearm is placed in pronation to expose the radial dorsal face of the wrist, ischemia is achieved by elevating the limb, and an ischemia cuff is then inflated to 250mmHg to allow a better view of the 1,2 ICSRA.
A centered “italic S” incision is made over the anatomic snuff box, extending from the base of the 1st metacarpal bone up to 3cm above the anatomic snuff box. The 2nd extensor compartment is exposed dorsally, identifying the tendon of the long extensor muscle of the thumb and identifying the short thumb extensor muscle volarly.
The 1,2 ICSRA, branch of the radial artery, is located between the 1st and 2nd dorsal extensor compartment and presents a retrograde flow. When the fascia between the tendons is opened, the surgeon needs to take care not to cut the superficial sensitive branch of the radial nerve, which is found superficially to the tendon of the long extensor muscle of the thumb.
Both tendons are then separated, retracting the long extensor of the thumb in the dorsal and cubital direction. Identification is established for the radial artery (which crosses the inferior border of the surgical wound supported on the bone) and the tendon of the long radial extensor muscle of the carpus (found in the dorsal side of the wrist joint). This tendon is displaced and retracted in the dorsal and cubital direction along with the tendon of the long extensor muscle of the thumb, to expose the radial dorsal face of the wrist joint.
The next step was a longitudinal incision in the wrist joint capsule. The capsule is retracted in the volar and dorsal direction to expose the joint between the distal end of the radius and the proximal end of the scaphoid. Together with the joint capsule, the radial artery is separated in radial and volar direction. The area of pseudarthrosis of the scaphoid and the radial metaphyseal area, the bone graft donor, are visualized.
We determine the size and shape of the appropriate wedge of the vascularized radial graft of the 1,2 ICSRA to correct the scaphoid defect. We extract the cortical/spongy bone block of the radius, leaving a distance of approximately 1.5cm to avoid injuring the carpal-radial joint, together with the vascular pedicle (branch of the radial artery). We then ligate the artery and the veins proximal to the graft area with 8/0 monofilament. Finally, we check the graft for bleeding by decreasing the pressure of the ischemia cuff. We place the graft and perform an osteosynthesis with Herbert-type screw, to add stability.
The next step is the closure of the capsule and the muscular and cutaneous planes. Mean surgical time was 90min. Lastly, a palmar splint is placed over the wrist, extending to the first finger, to immobilize the wrist for 6 weeks.
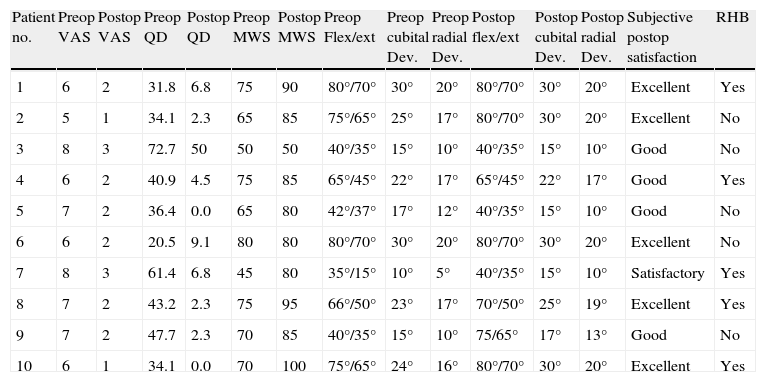
ResultsMean follow-up time in our study was 31.4 months (3–48 months). We performed the statistical study using Student's t-test, Levene test, and Pearson's correlation coefficient. There was a mean increase of 16 points in the Mayo scale, while in that of QuickDASH there was a drop of approximately 34 points. There was a gain of 5° in flexion-extension and a mean of 2° respectively in both the cubital and radial deviations. The VAS score decreased a mean of 4.6 points and 5 patients evaluated their degree of satisfaction as excellent (Table 1). No patient reported worsening of movement, strength or pain after surgery, as compared with the preoperative situation. Only half of the patients operated needed rehabilitation and 5 of the 7 workers in our series returned to their previous employment positions.
Results of the pre- and post-operative variables.
| Patient no. | Preop VAS | Postop VAS | Preop QD | Postop QD | Preop MWS | Postop MWS | Preop Flex/ext | Preop cubital Dev. | Preop radial Dev. | Postop flex/ext | Postop cubital Dev. | Postop radial Dev. | Subjective postop satisfaction | RHB |
| 1 | 6 | 2 | 31.8 | 6.8 | 75 | 90 | 80°/70° | 30° | 20° | 80°/70° | 30° | 20° | Excellent | Yes |
| 2 | 5 | 1 | 34.1 | 2.3 | 65 | 85 | 75°/65° | 25° | 17° | 80°/70° | 30° | 20° | Excellent | No |
| 3 | 8 | 3 | 72.7 | 50 | 50 | 50 | 40°/35° | 15° | 10° | 40°/35° | 15° | 10° | Good | No |
| 4 | 6 | 2 | 40.9 | 4.5 | 75 | 85 | 65°/45° | 22° | 17° | 65°/45° | 22° | 17° | Good | Yes |
| 5 | 7 | 2 | 36.4 | 0.0 | 65 | 80 | 42°/37° | 17° | 12° | 40°/35° | 15° | 10° | Good | No |
| 6 | 6 | 2 | 20.5 | 9.1 | 80 | 80 | 80°/70° | 30° | 20° | 80°/70° | 30° | 20° | Excellent | No |
| 7 | 8 | 3 | 61.4 | 6.8 | 45 | 80 | 35°/15° | 10° | 5° | 40°/35° | 15° | 10° | Satisfactory | Yes |
| 8 | 7 | 2 | 43.2 | 2.3 | 75 | 95 | 66°/50° | 23° | 17° | 70°/50° | 25° | 19° | Excellent | Yes |
| 9 | 7 | 2 | 47.7 | 2.3 | 70 | 85 | 40°/35° | 15° | 10° | 75/65° | 17° | 13° | Good | No |
| 10 | 6 | 1 | 34.1 | 0.0 | 70 | 100 | 75°/65° | 24° | 16° | 80°/70° | 30° | 20° | Excellent | Yes |
Dev.: deviation; Flex/ext: flexion/extension; MWS: Mayo wrist score; postop: postoperative; preop: preoperative; QD: QuickDASH; RHB: rehabilitation.
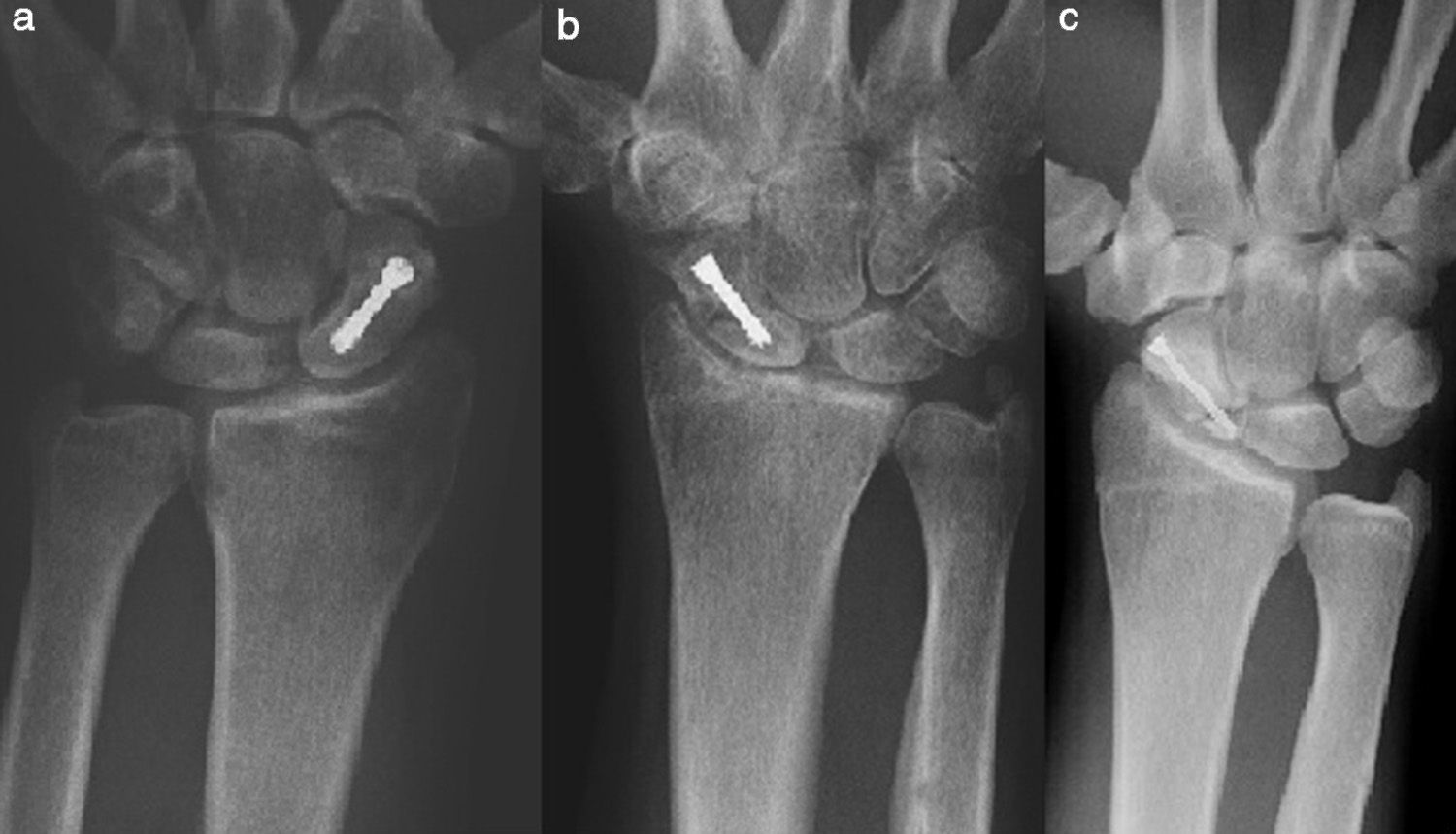
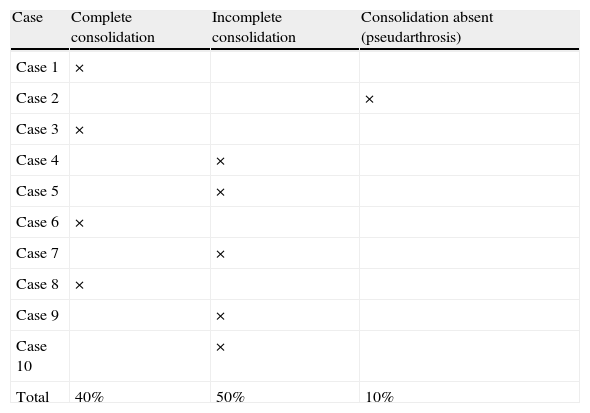
In our study we achieved a rate of complete consolidation in 4 patients (assessed only by X-ray) in a time period of 5.6 months (range: 2–12 months). In addition, the rate of nonunion, with consolidation of the pseudarthrosis area of more than 50%, appeared in another 5 patients. In only a single case were no signs of consolidation observed (Table 2) (Fig. 2).
As complications we can emphasize that we had to perform a rescue surgery on 3 of the 10 patients. This operation consisted of 2 extractions of the osteosynthesis material and 1 partial arthrodesis of the carpal bones with a 4-corner plate (from our point of view, due to poor technical indication). There were no infectious or scaphoid refracture complications. However, we did find a keloid on the scar from the surgical wound and a type I complex syndrome of regional pain in another patient.
DiscussionThe dorsal vascularized bone graft of the 1,2 ICSRA, used in our study, is the treatment of choice for scaphoid pseudarthrosis, with questionable viability of the proximal fragment, but without significant deformity or collapse. This is because it increases the blood supply in the area of nonunion, accelerates the process of ossification, and lowers the risk of new fracture of the scaphoid.29
The first studies on the treatment of scaphoid pseudarthrosis using vascularized bone graft date back to 1983 (Braun), followed by Kuhlmann, Kawai, and Yamamoto,17,18 who utilized a volar distal radial bone graft with pedicle of the pronator muscle.
Since its description by Zaidemberg et al., in 1991,18 the microvascularized graft with 1,2 ICSRA, with retrograde flow and of distal radius, has become more and more utilized for the treatment of pseudarthrosis of fractures with questionable viability of the proximal fragment, but without collapse and maintaining the shape of the scaphoid. In spite of this, the rates of consolidation for such pseudarthrosis vary widely and can range from 27% to 100%24 (Table 3).
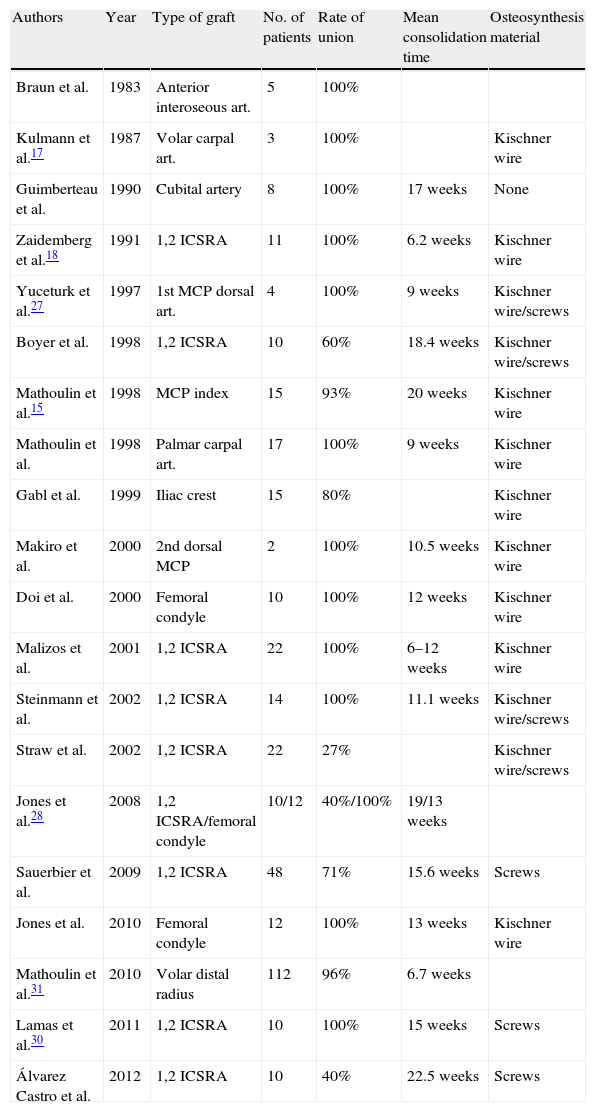
Studies Published on the Use of Various Grafts for the Treatment of Pseudartrosis of the Scaphoid.
| Authors | Year | Type of graft | No. of patients | Rate of union | Mean consolidation time | Osteosynthesis material |
| Braun et al. | 1983 | Anterior interoseous art. | 5 | 100% | ||
| Kulmann et al.17 | 1987 | Volar carpal art. | 3 | 100% | Kischner wire | |
| Guimberteau et al. | 1990 | Cubital artery | 8 | 100% | 17 weeks | None |
| Zaidemberg et al.18 | 1991 | 1,2 ICSRA | 11 | 100% | 6.2 weeks | Kischner wire |
| Yuceturk et al.27 | 1997 | 1st MCP dorsal art. | 4 | 100% | 9 weeks | Kischner wire/screws |
| Boyer et al. | 1998 | 1,2 ICSRA | 10 | 60% | 18.4 weeks | Kischner wire/screws |
| Mathoulin et al.15 | 1998 | MCP index | 15 | 93% | 20 weeks | Kischner wire |
| Mathoulin et al. | 1998 | Palmar carpal art. | 17 | 100% | 9 weeks | Kischner wire |
| Gabl et al. | 1999 | Iliac crest | 15 | 80% | Kischner wire | |
| Makiro et al. | 2000 | 2nd dorsal MCP | 2 | 100% | 10.5 weeks | Kischner wire |
| Doi et al. | 2000 | Femoral condyle | 10 | 100% | 12 weeks | Kischner wire |
| Malizos et al. | 2001 | 1,2 ICSRA | 22 | 100% | 6–12 weeks | Kischner wire |
| Steinmann et al. | 2002 | 1,2 ICSRA | 14 | 100% | 11.1 weeks | Kischner wire/screws |
| Straw et al. | 2002 | 1,2 ICSRA | 22 | 27% | Kischner wire/screws | |
| Jones et al.28 | 2008 | 1,2 ICSRA/femoral condyle | 10/12 | 40%/100% | 19/13 weeks | |
| Sauerbier et al. | 2009 | 1,2 ICSRA | 48 | 71% | 15.6 weeks | Screws |
| Jones et al. | 2010 | Femoral condyle | 12 | 100% | 13 weeks | Kischner wire |
| Mathoulin et al.31 | 2010 | Volar distal radius | 112 | 96% | 6.7 weeks | |
| Lamas et al.30 | 2011 | 1,2 ICSRA | 10 | 100% | 15 weeks | Screws |
| Álvarez Castro et al. | 2012 | 1,2 ICSRA | 10 | 40% | 22.5 weeks | Screws |
Source: Chang et al. modified.24.
Among the factors described in the failure of the vascularized graft, the following can be included advanced age, performance of a prior failed surgery, avascular necrosis of the proximal pole of the scaphoid, preoperative scaphoid deformity, resistance to the graft, early signs of carpal osteoarthritis, and the various osteosynthesis materials used, among others. Based on this we can state that not all grafts are appropriate for all types of pseudarthrosis, and that surgical indication of bone grafts with or without vascularization depends on these factors.
The non-vascularized bone grafts used in the techniques of Matti-Russe and Fisk-Fernández (of trapezoid shape) have various indications. The technique of Matti-Russe is performed in cases of stable pseudarthrosis without, or with minimum, displacement, because it does not make it possible to correct the “humpback” or “dorsal hump” deformities that the scaphoid can adopt. That of Fisk-Fernández is utilized in cases of unstable pseudarthrosis with deformity of the scaphoid, with the proximal fragment viable and without signs of advanced osteoarthritis in the carpus.29
Insofar as vascularized bone grafts, the one used by the volar pathway is indicated in alteration of the vascularization of the scaphoid, with deformity in flexion and shortening.29,31
As limitations of our work, we can point out that MRI with gadolinium was not used to diagnose avascular necrosis of the scaphoid, due to questions of healthcare pressure and delay of over 6 months to perform this test in our hospital, with the consequent surgical delay. We are conscious of the fact that this test, based on the study by Cerezal et al.,32 is the most reliable one to define vascularization of the proximal pole in scaphoid pseudarthrosis.30 We would also like to mention the limited size of our sample (n=10 cases), which leads to a loss of statistical power in our results.
Scaphoid pseudarthrosis is difficult to treat and represents one of the most significant challenges in hand surgery. Studies on the use of various types of grafts for the treatment of scaphoid pseudarthrosis3,24 have shown better results using vascularized bone graft (88% in pseudarthrosis consolidation), while this was only 47% using non-vascularized bone graft.5,6 Although the vascularized graft has been shown to be better in comparison with the non-vascularized, not all the studies have been favorable.5,24 Consequently, research with prospective random studies would help to define even better the risk factors that worsen the success rates for consolidation of pseudarthrosis. Likewise, such studies would help to establish indications and improvements for this complex surgical technique.
ConclusionsThere is a correlation between lower preoperative mobility and greater carpal osteoarthritis, with a worse prognosis for consolidation being associated with presence of lesions associated with pseudarthrosis. In carpal osteoarthritis, described as SNAC wrist by Krakauer, this disorder appears preoperatively in 2 patients. In patient number 3 grade iii SNAC wrist and in grade I SNAC wrist in patient number 9, and both with associated lesions that make the prognosis worse.
There is no clear correlation between the preoperative X-ray image and the range of wrist mobility and, evidently, patient satisfaction is related to the degree of postoperative mobility.
Although our results did not reach a rate of complete consolidation as high as that shown in the references (40% compared with 100%), the clinical evolution of our patients from the point of view of pain and arc of mobility improved in comparison with the preoperative situation. Our lower rate of consolidation could be related, as we have indicated in the discussion, to the healthcare limitations of our hospital environment with reference to requesting specific diagnostic image tests for this disorder.32 Likewise, it might be related to poor therapeutic indication on our part, in 2 patients of our series (patients 3 and 9) that, in presence of carpal osteoarthritis from previous associated lesions, cast a shadow on our results.
Even with these results and the limitations indicated, and after reviewing the literature, we believe that 1,2 ICSRA and osteosynthesis with Herbert-type screw is a treatment alternative to bear in mind for scaphoid pseudarthrosis, with questionable viability of the proximal pole and without presence of significant deformity or collapse, to improve pain and arc of mobility in the affected wrist.
Level of evidenceLevel of evidence 4.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that no experiments on human beings or animals were performed for this research.
Data confidentialityThe authors declare that they followed the protocols of their work center on the publication of patient data and that all patients included in the study received sufficient information and gave their informed consent in writing to participate in this study.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Álvarez-Castro A, Ramos-del Río A, Diez-Romero J, Alonso-Recio A, Fernández-Hernández Ó, Juárez-Cordero C, et al. Resultados del tratamiento de seudoartrosis de escafoides con injerto microvascularizado de arteria 1,2 intercompartimental suprarretinacular y osteosíntesis. Rev Esp Cir Ortop Traumatol. 2014;58:44–51.