Recurrent shoulder dislocation is infrequent after forty years and presents different injuries than younger patients.
ObjectiveTo compare injuries and complications after surgery between one group older than forty years of age and another younger group.
Material and methodsA review was made on all patients who had undergone arthroscopic surgery due to glenohumeral instability from 1999 until 2011. The mean follow-up was 64 months.
The case group consisted of all patients older than 40 years at the time of the surgery (n=21), which was compared with a similar sized control group of randomly selected younger patients (n=27).
ResultsThe mean age in the older group was 54 years (SD 11.86), while it was 26 years (SD 5.80) in the younger group.
No differences were founded between both groups in labrum injury, Hill–Sachs injury, and bone Bankart lesion (P>.05). Rotator cuff tears were 7.3 times (95% CI; 2.5–21.6) more frequent in the older group (81%) compared to the younger group (P<.05). However, neurological injuries after dislocation were not more frequent in this group.
There was no significant difference between the complications after surgery and the age according to the design (P>.05).
ConclusionsAnterior recurrent dislocation after forty years of age is usually associated with rotator cuff tears. Arthroscopic treatment of instability was effective with no more postoperative complications.
La inestabilidad glenohumeral recurrente es poco frecuente a partir de la cuarta década de la vida y presenta diferencias respecto de la del paciente más joven.
ObjetivoComparar las lesiones y las complicaciones postoperatorias de una población de 40 años o más intervenida de inestabilidad glenohumeral respecto a un grupo control más joven.
Material y métodosSe procedió a la revisión retrospectiva de los pacientes intervenidos mediante cirugía artroscópica de inestabilidad glenohumeral desde 1999 hasta 2011. Se realizó un seguimiento medio de 64 meses.
El grupo principal estaba constituido por todos los pacientes de 40 años o más intervenidos en el periodo de estudio (n=21), el cual fue comparado con un grupo control de pacientes más jóvenes seleccionado aleatoriamente con un tamaño similar (n=27).
ResultadosEn el grupo de los mayores, la media ± desviación estándar de edad fue de 54 ± 11,86 años, mientras que en el grupo de menor edad fue de 26 ± 5,80 años.
No se encontraron diferencias entre ambos grupos respecto a la presencia de lesión del labrum, lesión de Hill-Sachs y lesión de Bankart óseo (p>0,05). La lesión del manguito de los rotadores fue 7,3 veces (IC del 95%, 2,5–21,6) más frecuente en el grupo de mayor edad (81%) respecto los de menor edad (p<0,05). En cambio, las complicaciones neurológicas posteriores a la luxación no fueron más frecuentes en dicho grupo (p>0,05).
No se encontró asociación entre las complicaciones postoperatorias y la edad agrupada según el diseño (p>0,05).
ConclusionesLa inestabilidad glenohumeral anteroinferior recurrente después de la cuarta década de la vida presenta con frecuencia lesión del manguito de los rotadores. El tratamiento artroscópico de la inestabilidad fue eficaz, sin presentar mayores complicaciones postoperatorias.
Glenohumeral instability often becomes recurrent after the first episode of dislocation in young patients.1 The incidence of recurrence decreases after the fourth decade of life, ranging between 0 and 16%2 and becoming less frequent with increasing age; only 5–6% in patients older than 60 years.3
The initial dislocation in young patients involves lesions of the capsulolabral complex. At older ages, it often associates rotator cuff injuries, as well as a higher incidence of neurological lesions.4
Araghi reported that all patients over 40 years with recurrent instability presented lesions of the anteroinferior labrum, with between 35% and 100% of cases associating rotator cuff lesions.4 Other authors have reported rotator cuff and anterior capsule lesions and in all cases.5
Stayner points out that dislocations taking place after the fourth decade of life frequently associate neurological damage, in most cases neuropraxia of the axillary nerve.6 Toolanen found electromyogram alterations in 65% of patients aged over 40 years who suffered glenohumeral dislocation.7
In patients of advanced age, repeated dislocations often produce lesions in the rotator cuff, which plays an important role as a dynamic stabilizer of the shoulder joint. This has highlighted the special relevance of its repair in the treatment of glenohumeral instability.5,8,9
The aim of this study was to compare lesions and postoperative complications in a population of patients aged 40 years or more who underwent an arthroscopic intervention for glenohumeral instability compared to a control group of patients aged less than 40 years.
Material and methodsDesignWe conducted a retrospective study on a cohort of patients intervened for glenohumeral instability. The study period was from January 1999 until January 2011, with a minimum follow-up of 12 months and a mean duration of 64 months.
Inclusion criteria were patients with recurrent glenohumeral instability symptoms, who were treated by arthroscopic surgery upon failure of the rehabilitation treatment for at least 6 months.
We excluded fractures of the proximal end of the humerus (except Hill–Sachs lesion) and glenoid fractures over 30%, inveterate dislocations, neurological dislocations prior to the dislocation and open surgeries.
In addition, all patients were studied with preoperative magnetic resonance imaging or arthro-resonance. Ultrasound scans were obtained in cases with suspected tendon injury, although the inclusion criteria were clinical.
Patients were stratified into 2 groups according to their age at the time of surgery. The main group consisted of all patients aged 40 years or over who had undergone surgery during the study period (n=21). This group was compared with a similarly sized control group of randomly selected patients aged under 40 years (n=27).
The variables studied in each group were: age, gender, occupation, sport, laterality, dominance, dislocations prior to surgery, hospital reduction, capsulolabral lesions, rotator cuff lesions, surgical treatment, postoperative complications and reinterventions.
Data collection and analysisData collection was performed through electronic medical records and a clinical interview. The statistical analysis was performed using the SPSS 19.0 software program. The means were compared using the Student t test for variables with a normal distribution and the nonparametric Mann–Whitney U test for those without. Frequencies were compared with the chi-square test or Fisher exact test when the expected frequencies below 5 were over 20%.
Surgical techniquePatients were operated on and monitored by arthroscopic surgeons. The intervention was performed under general anesthesia, combined with interscalene nerve block in most cases. Patients were placed in a lateral position with the arm under simple traction of 3kg. The approach took place through anterior (work), posterior (vision) and anterosuperior (vision and work) portals. Capsulolabral lesions were treated by detachment, reinsertion of the labrum and capsular plication with suture-anchoring. Rotator cuff disinsertions were repaired either by direct suture or reanchoring, depending on the type of lesion. In general, patients were admitted for 24h for pain control. Postoperative revisions in consultation took place on the third and sixth weeks and on the third and fifth months.
Rehabilitation protocolWe maintained immobilization for the first 3 weeks using a sling which was removed for washing, elbow flexion and extension exercises and pendular shoulder movements. Between the third and sixth weeks we began the intermittent removal of the sling, as well as passive and assisted active exercises. In cases were the rotator cuff was repaired, this phase was delayed until the fifth-sixth week. After the sixth week we started non-assisted active exercises. Around week 10–12 we began the muscle strengthening phase. Usual sports and occupational activities were resumed on the fifth postoperative month.
ResultsDescriptive analysis of the sampleIn the group aged 40 years or more the mean±SD age was 54±11.86 years, while in the younger group it was 25.92±5.80 years.
We found an asymmetrical gender distribution by age group. Women were more predominant in the older group (61.9%), whereas males were more predominant in the control group (70.40%). These differences were statistically significant (P<.05).
The most frequently affected side was the right in both groups, which in most cases also corresponded to the dominant side.
In the older group, 72% of patients suffered an initial traumatic dislocation and required reduction in hospital. However, in the younger age group, 60% suffered an initial traumatic dislocation and only 31% of cases required reduction in hospital. Hospital reduction was 2.14 times (95% CI: 1.18–3.89) more frequent in the older group (P<.05).
We identified significant differences in the number of dislocations before surgery, which were more common in the younger group (P<.001).
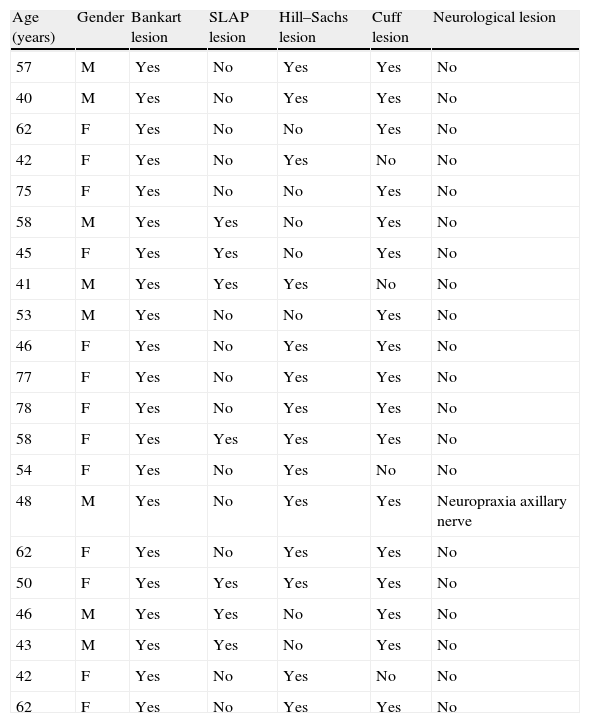
Lesions of the rotator cuffs were 7.3 times (95% CI: 2.5–21.6) more frequent among the older age group (81%) than the control group (11.10%) (P<.0001). Patients aged over 40 years underwent repair of the tendinous lesion in 50% of cases, whereas the remaining 31% were treated by regularization of the lesion, as they presented partial tears with few symptoms attributable thereto. The mean number of affected tendons for that group was 1 (interquartile range: 0.5–2) (Table 1).
Lesions in the group of patients aged 40 years or older.
| Age (years) | Gender | Bankart lesion | SLAP lesion | Hill–Sachs lesion | Cuff lesion | Neurological lesion |
| 57 | M | Yes | No | Yes | Yes | No |
| 40 | M | Yes | No | Yes | Yes | No |
| 62 | F | Yes | No | No | Yes | No |
| 42 | F | Yes | No | Yes | No | No |
| 75 | F | Yes | No | No | Yes | No |
| 58 | M | Yes | Yes | No | Yes | No |
| 45 | F | Yes | Yes | No | Yes | No |
| 41 | M | Yes | Yes | Yes | No | No |
| 53 | M | Yes | No | No | Yes | No |
| 46 | F | Yes | No | Yes | Yes | No |
| 77 | F | Yes | No | Yes | Yes | No |
| 78 | F | Yes | No | Yes | Yes | No |
| 58 | F | Yes | Yes | Yes | Yes | No |
| 54 | F | Yes | No | Yes | No | No |
| 48 | M | Yes | No | Yes | Yes | Neuropraxia axillary nerve |
| 62 | F | Yes | No | Yes | Yes | No |
| 50 | F | Yes | Yes | Yes | Yes | No |
| 46 | M | Yes | Yes | No | Yes | No |
| 43 | M | Yes | Yes | No | Yes | No |
| 42 | F | Yes | No | Yes | No | No |
| 62 | F | Yes | No | Yes | Yes | No |
F: female; M: male.
No differences were found between both groups regarding the presence of capsulolabral complex lesion, Hill-Sachs lesion, bony Bankart lesion and SLAP lesion (P>.05) (Table 1).
All patients presented labral lesions. Reinsertion took place in 100% of cases, with a mean number of 3 anchors being used in both groups.
SLAP lesion was found in 7 patients in the older age group and in 3 patients in the younger age group. In 7 cases, it was a type V lesion and in 3 cases it was a type I lesion. Type V lesions were treated by reinsertion with anchors (Table 1).
Regarding complications following the dislocation, there were no statistically significant differences between groups. The only case was a 48-year-old patient with axillary nerve neuropraxia caused by the dislocation. As sequelae, he presented hypoesthesia in the lateral region of the shoulder and motor deficit for shoulder abduction 4/5 (Table 1).
Analysis of complicationsWe did not observe any association between postoperative complications and the age groups established. However, our sample size offered a low statistical power for the association studied.
Postoperative complications were classified as major if they required reoperation and minor if they did not require surgery.
Among the major complications, there was 1 case of postoperative infection in the older age group which required arthroscopic lavage and specific intravenous antibiotic therapy. In addition, 3 patients in the younger age group required reoperation due to pain and stiffness. All cases underwent arthroscopic arthrolysis. In 2 cases, it was necessary to remove protruding metallic implants.
Among the minor complications, 2 patients presented a feeling of instability without reaching redislocation. Reoperation was not necessary in any case.
Upon analysis of prognostic factors, no differences in complications were found by comparing the established age groups (P>.05): 13.6% in the group >40 years and 19.2% in the group <40 years, or comparing by gender (P>.05): 7.4% in males and 9.5% in females. Neither were there any statistically significant differences (P>.05) in complications in relation to the number of dislocations prior to surgery; 0% when there had been more than 3 dislocations and 13.8% when there had been less than 3.
Patients who did not require reduction in hospital, 12.5% compared to 4.2% who did require hospital reduction (P>.05), did not develop further complications.
DiscussionRecurrent glenohumeral instability is a rare entity after the fourth decade of life,2,3 which characteristically presents different lesions compared to cases occurring in younger patients.10,11 Therefore, the diagnosis and therapeutic management should be specific for this age group.
A degenerative process of the rotator cuff tendons takes place between the fourth and sixth decades of life,12 making them more vulnerable to lesions.13,14 The rotator cuff acts as the main dynamic stabilizer of the shoulder joint15 so its lesions affect glenohumeral stability.15–19In vitro studies have shown that the loss of 2 rotator cuff tendons plays a significant role in the recurrence of instability.20 Some authors have reported rotator cuff injuries in 100% of patients with recurrent dislocation.4,5
Voight points to age and number of redislocations as risk factors for rotator cuff injury.8 Porcellini suggests an association between the number of redislocations and rotator cuff injuries, especially after 7 dislocations in patients aged 40–60 years. On the other hand, no such association existed with Bankart and capsular lesions.16
In our series, 81% of older patients presented tendon injury, thus making it 7.3 times more frequent compared to younger patients (11.10%) (P<.05). However, no differences were found for other lesions. Neither was an association found between the number of dislocations prior to surgery and tendinous and Bankart lesion.
Given the high incidence of tendinous lesions in glenohumeral dislocation among elderly patients, physical examination and a preoperative study are essential14 in order to establish adequate surgical planning.9
Neurological lesions following anteroinferior shoulder dislocations are more common among older patients,7 with vascular lesions being very rare at any age.21 Occasionally, a neurological lesion of the brachial plexus may coincide with massive rotator cuff tear, thus masking the lesion and delaying its treatment. This entity was first described by González22 and subsequently named by Groh as “terrible triad of the shoulder”.23
No patient in our series suffered vascular lesions after dislocation and only 1 patient in the older group presented neuropraxia of the axillary nerve. No significant differences in neurovascular complications after dislocation were found between both age groups, thus contradicting the reports in the literature.6,7
The treatment of anteroinferior glenohumeral instability has undergone a gradual evolution in recent decades. Many techniques, both open5 and arthroscopic,24,25 have been proposed throughout this development.
Voight proposed repair of the labrum and rotator cuff lesion in active patients aged under 60 years, whilst also suggesting that tendon repair would be sufficient for patients aged over 60 years with less physical activity.8 Neviaser proposed that rotator cuff and capsule repair would be enough to restore shoulder stability.5
Regarding the results, Maier published identical redislocation results in younger patients compared to older patients, with the latter presenting worse functional results.26 Other authors argue that the functional results and residual chronic pain eventually improve in cases associating rotator cuff repair.27 Rapariz stated that functional outcome was directly influenced by rotator cuff injuries in the sagittal plane, especially when they affected structures in the anterior pillar.28
Although rotator cuff repair exclusively has been proposed as a treatment option for glenohumeral instability in patients with advanced age,5,11 most authors recommend associating it to capsulolabral repair.8,16,28–30
In our experience, arthroscopic repair offered excellent results in restoring stability, since there were no cases of redislocation. Regarding postoperative complications, the most frequent were limitation of mobility and pain, with only 3 patients in the younger age group requiring reoperation.
Age, gender and the number of previous dislocations were not associated to a higher incidence of postoperative complications. In addition, no further risk factor for their development was found.
The limitations of our study included the limited sample size, which entailed a low statistical power. The reason for this was that recurrent shoulder instability is a rare entity after the fourth decade of life. Moreover, an assessment of functional outcomes was not performed, since this was not among the objectives of the study.
ConclusionsAfter the fourth decade of life, patients with recurrent shoulder dislocations often present rotator cuff lesions. However, they do not develop major neurological complications after dislocation.
The arthroscopic treatment of recurrent instability in patients aged over 40 years by reanchoring of the labrum and capsular plication is effective to restore joint stability, with no higher incidence of postoperative complications being found.
Level of evidenceLevel of evidence III.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation adhered to the ethical guidelines of the Committee on Responsible Human Experimentation, as well as the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
The authors wish to express their gratitude to the Traumatology and Orthopedic Surgery Service at Alcorcón.
Please cite this article as: López-Hualda A, Marín-Aguado MA, Valencia-García H, López-González D, Gavín-González C. Inestabilidad glenohumeral en pacientes mayores de 40 años: lesiones, tratamiento y complicaciones. Rev Esp Cir Ortop Traumatol. 2014;58:38–43.