Mostrar nuestra experiencia con el uso del abordaje de Stoppa sobre fracturas del acetábulo con afectación de la lámina cuadrilátera.
Material y métodoEstudio retrospectivo; nivel iv. Todos los pacientes fueron intervenidos en un centro de tercer nivel por cirujanos con experiencia en el tratamiento de fracturas pélvicas. Se recogieron datos sobre los pacientes, sus lesiones, particularidades del tratamiento y resultados clínicos y radiológicos. Se llevó a cabo un análisis estadístico descriptivo y analítico.
ResultadoLa muestra se compuso de 16 pacientes. Quince sufrieron fracturas asociadas. En 15 se emplearon implantes anatómicos específicos y en 4 abordajes ampliados. La reducción fue anatómica en 9. Siete presentaron alguna complicación, requiriéndose procedimientos adicionales en 4. Destacó la alta tasa de infección postoperatoria, que se dio en 3 pacientes.
DiscusiónLos resultados radiológicos son asimilables a los previamente reportados en la literatura. No obstante, experimentamos una alta tasa de complicaciones. Sobre ello pudo influir la especial dificultad de los casos y el proceso de adaptación a la nueva técnica.
ConclusiónMediante el abordaje de Stoppa hemos conseguido una alta tasa de reducciones buenas o anatómicas. Sin embargo, es una técnica exigente y no exenta de complicaciones.
To report our experience with the use of Stoppa approach for fractures of the acetabulum with quadrilateral plate involvement.
Material and methodRetrospective study; level iv. All patients were operated in a third level trauma center. The surgical team was experienced in the management of pelvic fractures. Data about patients, injuries, treatment features and clinical and radiological results were collected. We performed a statistical analysis; both descriptive and analytical.
Result16 patients integrated the sample. 15 suffered associated fracture patterns. Anatomical plates were used in 15. Four required extended approaches. Reduction was anatomical in 9. 7 suffered some complication, needing the additional surgical procedures in 4. The surgical site infection rate was particularly high, appearing in 3.
DiscussionRadiological results were within the previously reported. We had a high complication rate, particularly infection. This outcome may be influenced by the special complexity of our cases and the adaptation process to a new technique.
ConclussionUsing the Stoppa approach we achieved lots of good or anatomical reductions. However, is an exigent and not without complications technique.
Reducing acetabular fractures affecting the quadrilateral plate remains a challenge for the orthopaedic surgeon. Achieving anatomical and stable osteosynthesis is difficult using the classical approaches (ilioinguinal and Kocher–Langenbeck), since exposure and the ability to manipulate fragments are limited. Moreover, the intense manipulation of neurovascular structures and the wide dissection of muscular planes increase the risk of complications.1,2
In recent years several anterior intrapelvic approaches have been developed. These include the very popular modified Rives-Stoppa approach. This was described in 1984 for the treatment of complex or recurrent inguinal hernias,3 and later extended to the treatment of pelvic ring4 and acetabular fractures.5
We present a case series of acetabular fractures affecting the quadrilateral plate, operated after the recent introduction of the Stoppa approach in our centre.
Material and methodThis is a retrospective study. All the patients were operated in a tertiary level hospital between March 2015 and May 2017 by the same surgical team. The cases were followed up from the start of recruitment until June 2017. All available patients with displaced acetabular fracture and quadrilateral plate involvement treated by internal fixation using a Stoppa-type anterior intrapelvic approach were included. Skeletally immature subjects were excluded.
All the fractures were studied by simple radiography (X-ray) and computed tomography and classified according to the system proposed by Judet et al.6 The appearance of a “Gull sign” (superomedial impaction)7 and central dislocation were collected. Preoperative planning was carried out. The quality of reduction was classified by X-ray according to the system proposed by Matta,8 which covers 4 typologies: anatomical reduction (separation of fragments 0–1 mm), imperfect (2–3 mm), poor (>3 mm) and secondary surgical congruence. RAIM Viewer® (Centre d’Imatge Mèdica Digital, Corporació Sanitària Parc Taulí; Sabadell, Barcelona, Spain) was used for the radiographic analysis.
In all cases, cotrimoxazole 800 + 160 mg was administered intravenously; one preoperative dose and two postoperative doses every 12 h. Low molecular weight heparin was used for antithrombotic prophylaxis according to size and weight from admission to start of weight-bearing. General anaesthesia with orotracheal intubation and bladder catheterisation were employed systematically.
The patients were placed in the supine position on a radiotransparent operating table. A continuous traction device was not used. The surgical field was prepared including the lower limb on the side of the fracture. The main surgeon placed him/herself in front of the opposite hip to the injury; one of their 2 assistants in front of the other hip and the other in front of the limb on that side in order to be able to manipulate it. The skin incision was of the Pfannenstiel type (transversal suprapubic). A longitudinal incision was made in the linea alba and the abdominal wall musculature retracted to either side. The space of Retzius was obliterated with gauze, which separates and protects the bladder. The deep dissection ran posteriorly over the periosteum of the pectineus crest. Flexion of the hip then helped the femoral neurovascular bundle to lose tension. Malleable blades are recommended to retract the peritoneal sac.5 The corona mortis, if found, was attached with a LIGACLIP® (Ethicon®) multiple clip applier. The approaches were extended depending on the type of fracture and need for exposure.
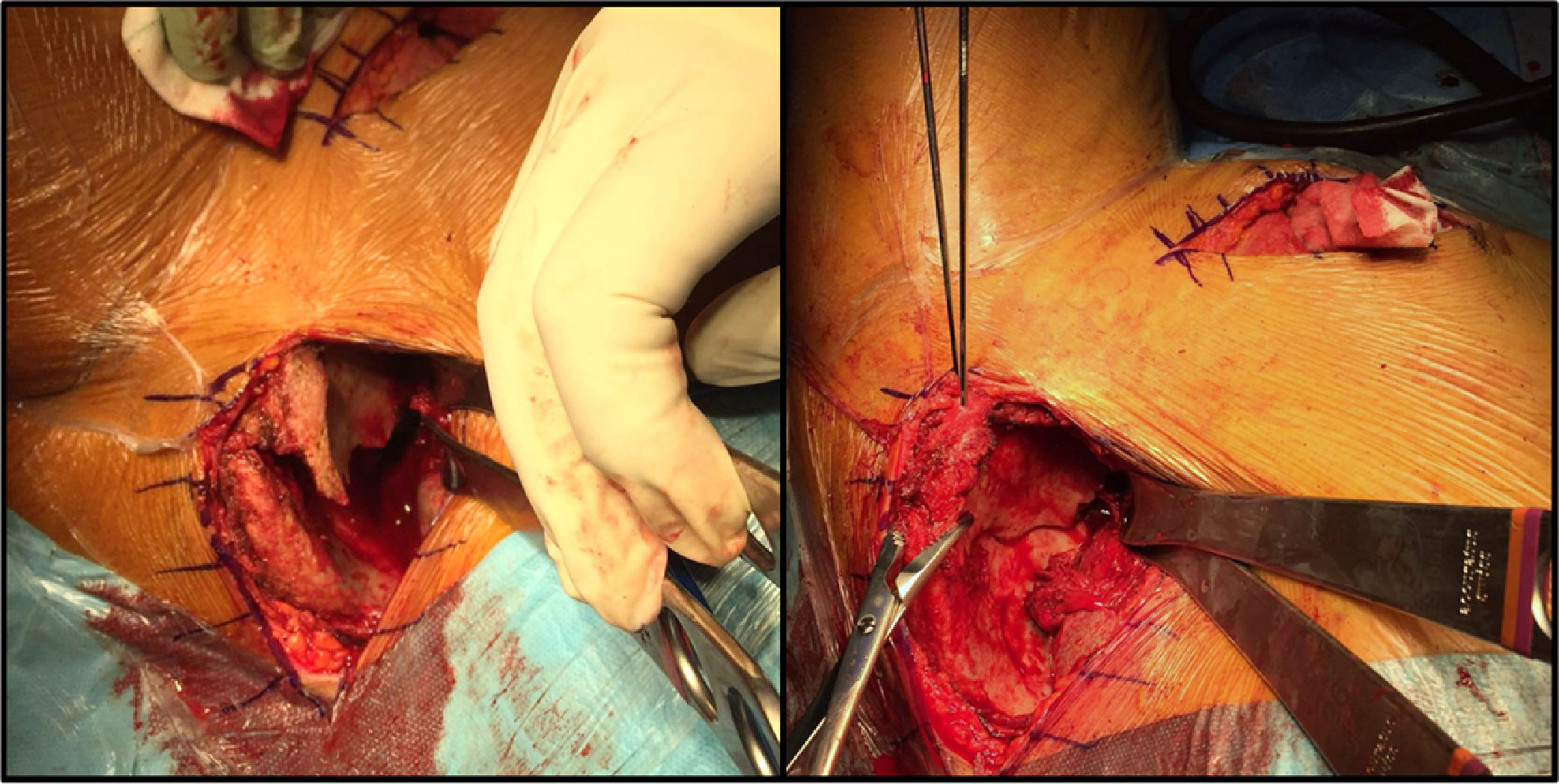
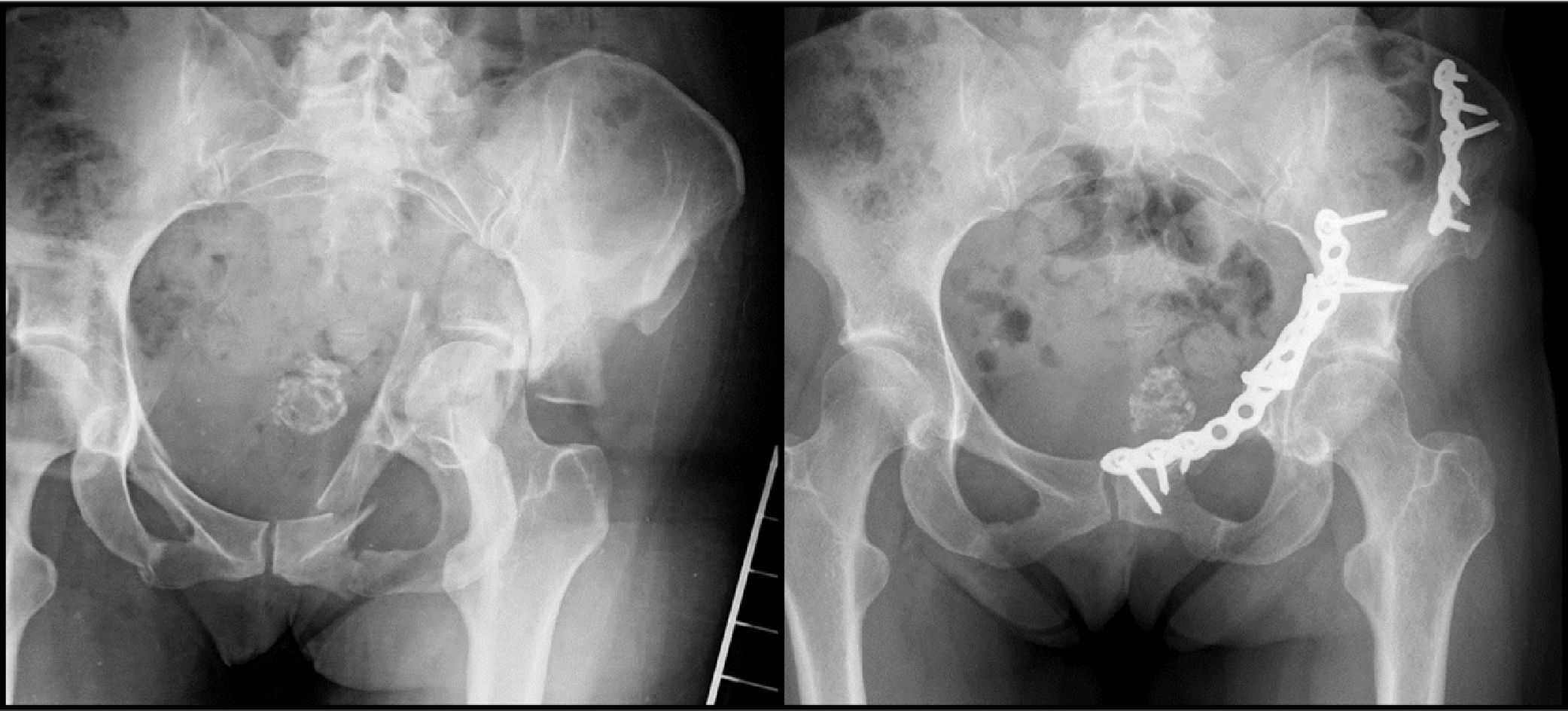
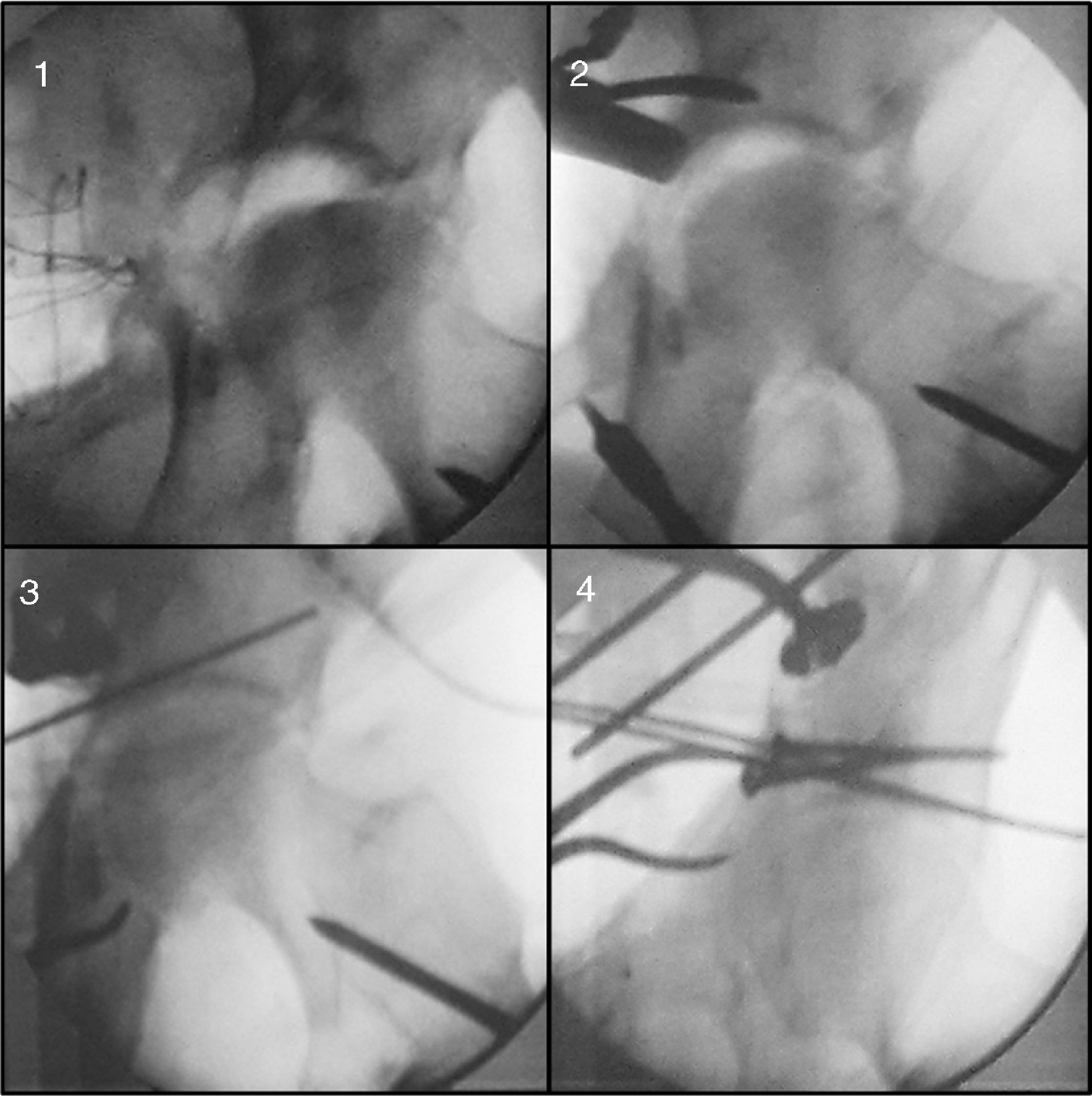
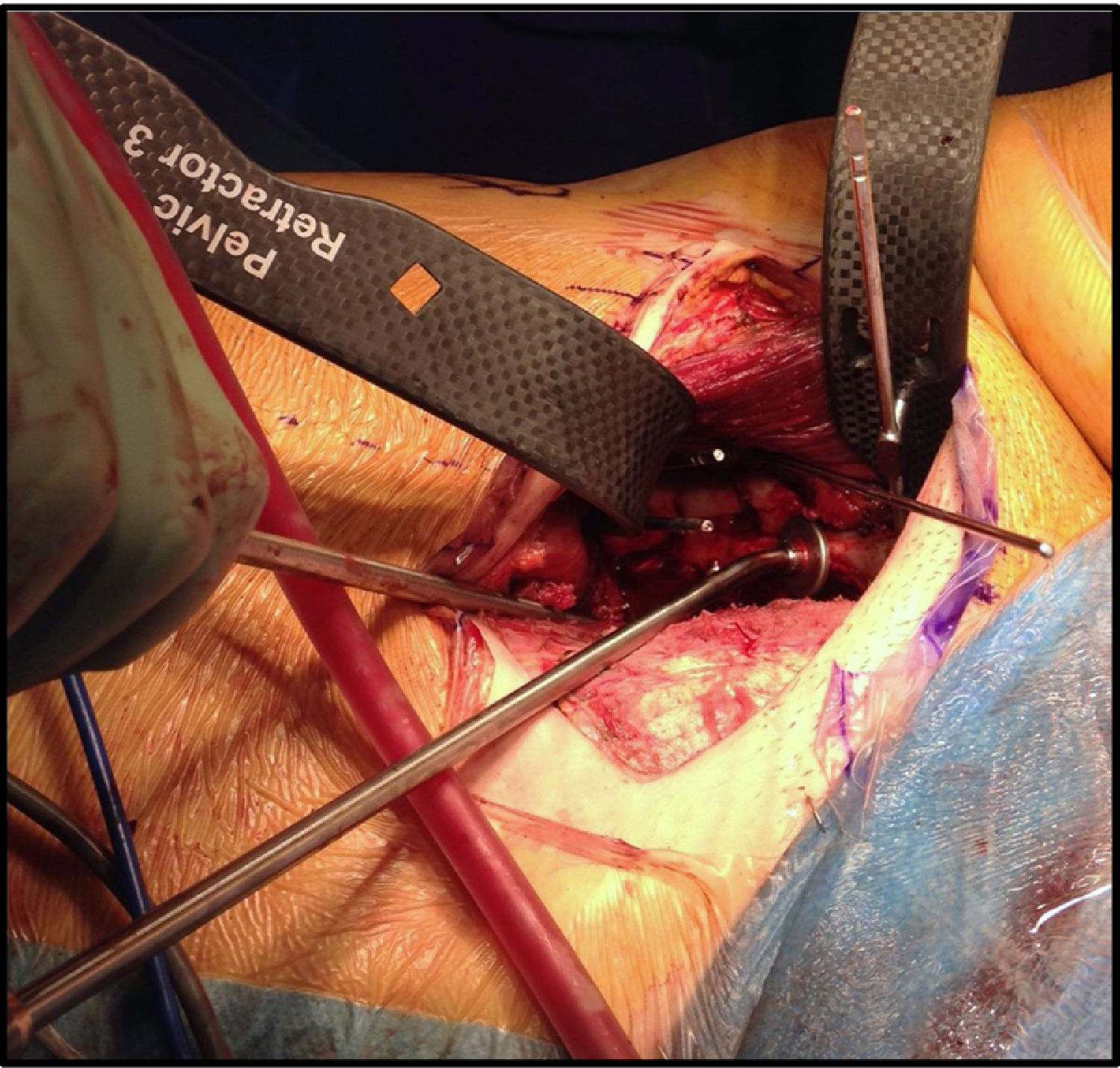
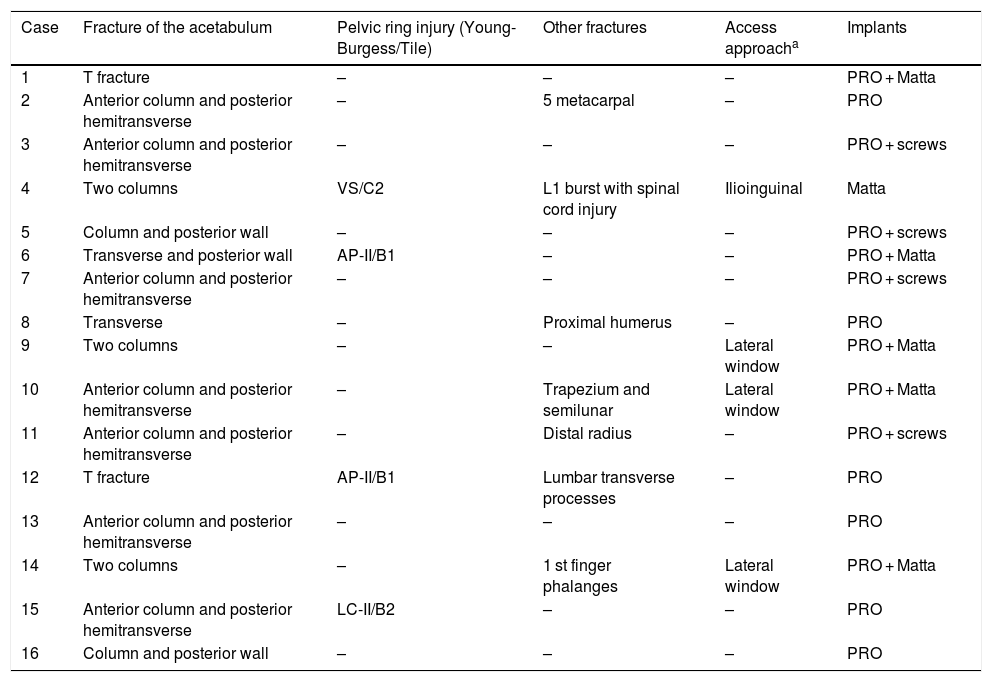
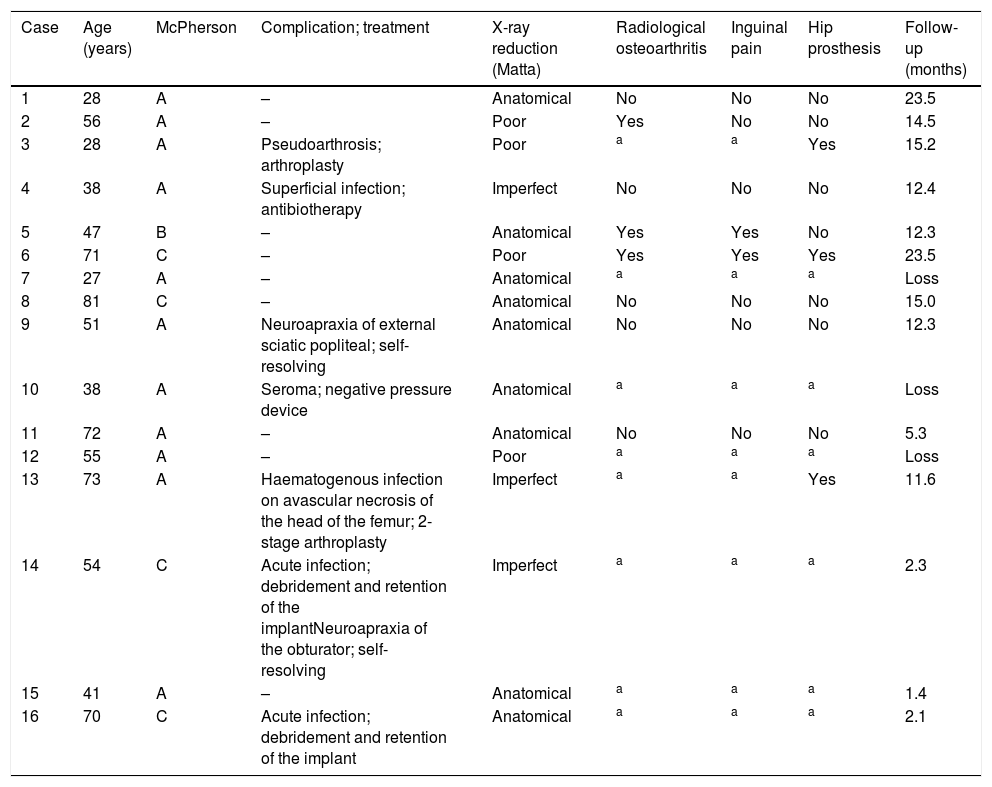
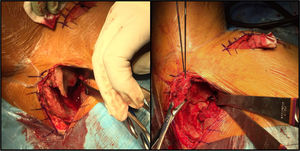
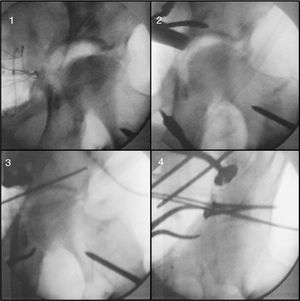
The various fracture components were reduced and stabilised in a centripetal direction. Iliac fossa fractures, more easily accessed through the lateral window of the iliolinguinal approach were always stabilised first. Fig. 1 is an example of this step. The preoperative and postoperative radiological images of the same patient are shown in Fig. 2. The anterior column was reduced by direct manipulation, usually with forceps. To correct its medialisation, traction can be applied through a Schanz screw implanted in the neck of the femur. The hip is accessible through the fractured quadrilateral plate, allowing the removal of retained osteochondral fragments or the diagnosis of chondral injuries. Depression in the weight-bearing area (if this occurs) can be corrected by disimpacting the roof with an elevator through the joint line. Once reduced, it is filled with bone graft and stabilised with support screws. This manoeuvre is shown in Fig. 3. Reduction of the quadrilateral plate is essential to verify that the joint reconstruction is anatomical. This can be achieved by exerting a lateral force vector directly through the endopelvic plate, which has a support effect in this direction.5,9Fig. 4 illustrates the exposure achieved with the approach and the ability to control fragments.
Fracture reduction must be performed in a centripetal direction (towards the joint), so that the mobilisation of the joint fragments is not affected by poor reduction of more peripheral lines. Dissection of a lateral window is essential to control high fractures of the anterior column or iliac fossa, as can be seen in the image. Note the notching, in which the ipsolateral extremity is free.
The images correspond to the patient in Fig. 1, a 51-year-old woman with a fracture of the 2 columns. Through an lateral access window, the fracture of the iliac fossa was reduced. Subsequently a Stoppa approach was created through which the remaining components of the fracture could be reduced and stabilised, including the quadrilateral plate. An anatomical quality reduction was achieved.
The image is an example of how it is possible to correct impaction of the roof through the fracture site. (A) the superomedial impaction and the end of the Schanz screw implanted in the femur on which it is tractioned can be seen. (B) A periosteal elevator is inserted below the joint surface to elevate the depression. (C) The correction is temporarily stabilised with Kirschner needles. (D) Definitive stabilisation with support screws between joint fragments. The endopelvic plate with be placed later.
In the image the available surgical field can be seen from the side opposite the lesion. For better exposure, we used the radiotransparent retractors of the PRO® (Stryker®) system. In this case, the medialisation and extension of the anterior column were corrected with a pusher applied over the pectineus crest. The force was directed laterally and caudally. Once the desired correction was achieved, osteosynthesis was completed with an endopelvic support plate.
The acetabular and pelvic osteosynthesis systems PRO® and Matta® (Stryker®) were chosen for osteosynthesis of the acetabular and anterior pelvis, including their sequential retractors, straight and mouldable curved plates, endopelvic anatomical plates and associated screws. If there was associated pelvic ring instability, osteosynthesis of the posterior pelvis was performed with cannulated sacroiliac screws (aap Implantate AG®).
A suction drain was inserted into the deep space in all patients and removed 24h following the surgery. Sitting and transfer were allowed, supported on one foot contralateral to the injury, were allowed 48 h following the procedure, at which time the urinary catheter was removed.
The variables gathered were: demographic characteristics, history (based on the staging system of McPherson for periprosthetic hip infection10), occurrence mechanism, associated injuries in the pelvis or other fractures, emergent and definitive treatment modality (including the chronology of care milestones, operating time and implant used) and clinical and radiological results, as well as blood analysis parameters. A descriptive and analytical statistical analysis was performed with Stata’s suite® (StataCorp®; College Station, Texas, U.S.A.). Pearson’s χ² test was used for the comparison of proportions. The non-parametric Mann–Whitney U test was used for comparison of 2 means, given the sample size. To compare the means of more than 2 groups, we chose the Kruskal–Wallis non-parametric test.
ResultsTable 1 summarises data on demographics, type and mechanism of injury, and treatment modality. Table 2 summarises the outcome of procedures at the end of follow-up together with the patients’ characteristics.
Characteristics of the fractures, associated injuries and treatment.
| Case | Fracture of the acetabulum | Pelvic ring injury (Young-Burgess/Tile) | Other fractures | Access approacha | Implants |
|---|---|---|---|---|---|
| 1 | T fracture | – | – | – | PRO + Matta |
| 2 | Anterior column and posterior hemitransverse | – | 5 metacarpal | – | PRO |
| 3 | Anterior column and posterior hemitransverse | – | – | – | PRO + screws |
| 4 | Two columns | VS/C2 | L1 burst with spinal cord injury | Ilioinguinal | Matta |
| 5 | Column and posterior wall | – | – | – | PRO + screws |
| 6 | Transverse and posterior wall | AP-II/B1 | – | – | PRO + Matta |
| 7 | Anterior column and posterior hemitransverse | – | – | – | PRO + screws |
| 8 | Transverse | – | Proximal humerus | – | PRO |
| 9 | Two columns | – | – | Lateral window | PRO + Matta |
| 10 | Anterior column and posterior hemitransverse | – | Trapezium and semilunar | Lateral window | PRO + Matta |
| 11 | Anterior column and posterior hemitransverse | – | Distal radius | – | PRO + screws |
| 12 | T fracture | AP-II/B1 | Lumbar transverse processes | – | PRO |
| 13 | Anterior column and posterior hemitransverse | – | – | – | PRO |
| 14 | Two columns | – | 1 st finger phalanges | Lateral window | PRO + Matta |
| 15 | Anterior column and posterior hemitransverse | LC-II/B2 | – | – | PRO |
| 16 | Column and posterior wall | – | – | – | PRO |
Matta: pelvic osteosynthesis plates of Matta®, Stryker® system; PRO: endopelvic anatomical plate of the PRO®, Stryker® system; screws: use of screws to inter-fragments not connected to plates.
Patient characteristics, complications and results.
| Case | Age (years) | McPherson | Complication; treatment | X-ray reduction (Matta) | Radiological osteoarthritis | Inguinal pain | Hip prosthesis | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|
| 1 | 28 | A | – | Anatomical | No | No | No | 23.5 |
| 2 | 56 | A | – | Poor | Yes | No | No | 14.5 |
| 3 | 28 | A | Pseudoarthrosis; arthroplasty | Poor | a | a | Yes | 15.2 |
| 4 | 38 | A | Superficial infection; antibiotherapy | Imperfect | No | No | No | 12.4 |
| 5 | 47 | B | – | Anatomical | Yes | Yes | No | 12.3 |
| 6 | 71 | C | – | Poor | Yes | Yes | Yes | 23.5 |
| 7 | 27 | A | – | Anatomical | a | a | a | Loss |
| 8 | 81 | C | – | Anatomical | No | No | No | 15.0 |
| 9 | 51 | A | Neuroapraxia of external sciatic popliteal; self-resolving | Anatomical | No | No | No | 12.3 |
| 10 | 38 | A | Seroma; negative pressure device | Anatomical | a | a | a | Loss |
| 11 | 72 | A | – | Anatomical | No | No | No | 5.3 |
| 12 | 55 | A | – | Poor | a | a | a | Loss |
| 13 | 73 | A | Haematogenous infection on avascular necrosis of the head of the femur; 2-stage arthroplasty | Imperfect | a | a | Yes | 11.6 |
| 14 | 54 | C | Acute infection; debridement and retention of the implantNeuroapraxia of the obturator; self-resolving | Imperfect | a | a | a | 2.3 |
| 15 | 41 | A | – | Anatomical | a | a | a | 1.4 |
| 16 | 70 | C | Acute infection; debridement and retention of the implant | Anatomical | a | a | a | 2.1 |
This was a sample of 16 patients, 11 males and 5 females. The mean age was 52 (range 28–81). Road traffic accidents and falls were the most common causative mechanisms. Falls from a height are a common cause of fracture in elderly patients. Fifteen of the 16 fractures were associated, the most frequent being association of a line in the anterior column with a posterior hemitransverse line. All the transverse lines were transtectal or supratectal. In the only case with a line in the posterior wall, the stability of the joint made it possible to dispense with a posterior approach. All 2 column fractures required an extended approach. The operating time was an average of 214 min. An increase in operating time was observed for fractures of 2 columns and patients with associated pelvic ring instability, these differences were not significant. The mean time from admission to surgery was 9.4 days (range 2–18). The mean total length of admission was 19.5 days (range 13–84, the latter being a patient with a spinal cord injury admitted to complete an intensive physiotherapy regimen). All the patients, with the exception of one who disregarded their surgeon’s instructions, maintained non-weight bearing on the operated limb for at least 10 weeks. The mean duration of follow-up was 12 months (range 2–24). There were 3 losses to follow-up.
The mean reduction in haemoglobin was 2.1 g/dl, and 8.9% in the haematocrit. Six patients required a postoperative transfusion. The quality of reduction was anatomical in 9 cases, imperfect in 3 and poor in 4. A concentric, congruent and competent reconstruction of the hip joint was achieved in all cases. Seven patients had some complication related to the procedure, and 4 required additional surgical procedures. There was one case of avascular necrosis of the femoral head that was superinfected by haematogenous seeding of urinary origin. A 2-stage hip arthroplasty was performed. In the first stage, an attempt was made to remove the osteosynthesis material, which was impossible for technical reasons. The patient is currently free of signs of periprosthetic infection. There was no case of hernia, heterotopic ossification, vascular or genitourinary injury. A greater aggregation of complications was found in patients operated using an extended approach compared to those who did not require this, the difference was statistically significant (p = .032).
At the end of the study, 3 of the 10 patients with prolonged follow-up were implanted with a prosthesis: due to complications in 2 cases and only in one case due to a symptomatic post-traumatic arthropathy. Of the 7 patients who kept their own joint, 3 developed a coxarthrosis, 2 of which were symptomatic.
DiscussionInvolvement of the quadrilateral plate is frequently associated with compound fractures of the acetabulum with lines in the anterior column, especially in the elderly. It is not a component located in the weight-bearing area, but it affects outcome as it implies greater difficulty in reconstruction and its reduction is essential to achieve adequate joint congruence.11–13 It is difficult to manipulate through an ilioinguinal approach. By contrast, with a modified Stoppa approach it is possible to expose 80% of its surface, as well as the greater part of both columns and the anterior wall of the acetabulum14 (also both acetabula with a single incision). Anatomical plates have been developed with support on the quadrilateral plate for specific use in this approach11–15 and were used in 15 of the 16 cases of the study.
Unfortunately, not all fracture components can be, managed using this technique, it is not feasible to reduce, stabilise fractures of the iliac fossa or fractures that run very high in the anterior column. Therefore it is essential to create the first window of the classical ilioinguinal approach.9 In recent studies, the combination of the lateral window has been reported with a frequency from 40% of surgeries to its systematic use.15–20 In our study, this was only the case for 19% of procedures. The patients who underwent an extended approach suffered more complications, which is probably attributable to greater complexity of the injuries (3 of them were fractures of the 2 columns) and greater surgical exposure. With an anterior intrapelvic approach it is also not possible to manipulate fractures of the posterior wall. In this sample it was not necessary to combine a posterior approach, which is logical given the inclusion criteria (involvement of the quadrilateral plate; much more frequent in predominantly anterior patterns). However, it has been used in up to 32% of cases by other authors.5,21
We could not relate greater bleeding and transfusion requirement with delay until surgery, complexity of the fracture or operating time. The mean duration of the procedure was 214 min, this is consistent with those previously reported which range from 183 to 263 min.5,16,17,19,21
We experienced a high rate of complications (44% of the total). In previous publications, the frequency of complications ranged from 7% to 33%; including those of the approach itself (injury to the obturator nerve, large vessels, genitourinary structures and hernias) and those common to any osteosynthesis in the hip joint (infection, loss of reduction, pseudoarthrosis, thromboembolism, arthropathy, avascular necrosis, etc.5,11,15–24). We should point out that almost all the fractures were associated and more than half of the patients were referred to us because of their particular complexity, biases that might have affected this result. No relationship was found between the onset of complications and theoretical risk factors. The high incidence of infections (25%) is remarkable: 3 in relation to the procedure and one haematogenous infection over an avascular necrosis, whereas it ranges from 2% to 13% in the literature.5,11,15–20,23,24 Methicillin-sensitive Staphylococcus aureus, the most commonly reported germ in the literature,25,26 was isolated in the intra-operative cultures of 3 surgical bed infections. In the remaining case, a gram-negative bacillus of urinary origin was found. Different risk factors have been postulated whose increase or presence raises the likelihood of infection after osteosynthesis of the acetabulum: operating time, body mass index, length of admission in intensive care, bleeding, and transfusion requirement, abdominal or genitourinary trauma and Morel–Lavallée seroma.25,26 In our case, it was not possible to find a connection with any of these.
Poor quality reduction has been associated with poor function, radiological progression of osteoarthritis and the need for arthroplasty.8,23,27,28 In the literature, the proportion of cases in which an anatomical reduction is achieved (maximum separation in weight-bearing area <1 mm) using a Stoppa approach ranges from 40% to 83%.4,5,11,15–19,21–23,29 In our series, we achieved a reduction of anatomical quality in 56% of the patients. We were unable to associate data on reduction quality of progression of osteoarthritis or pain.
This paper has various methodological limitations: its retrospective nature, small sample size, large dispersion of independent variables, absence of a control group to compare the technique with other available techniques, uneven follow-up of cases, absence of functional tests and radiological assessment by a single observer. In particular, the low number of patients made it difficult to find statistically significant differences. However, as far as we know, this is the first report in Spanish on a series of fractures of the acetabulum with involvement of the quadrilateral plate operated using a modified Rives-Stoppa approach.
To conclude, in our study we experienced a high rate of complications, which we attributed to the process of adaptation to a new technique and to the special complexity of the fractures in the sample. However, we consider that the Stoppa approach is a valid and recommendable alternative given its technical advantages: easy, wide and safe exposure; ability to manipulate the fracture and quadrilateral plate to enable anatomical joint reduction, and the existence of specific instruments and implants.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Andrés-Peiró et al. Estudio retrospectivo sobre 16 fracturas de acetábulo con afectación de la lámina cuadrilátera tratadas con un abordaje anterior intrapélvico de Rives-Stoppa modificado. Rev Esp Cir Ortop Traumatol. 2019;63:416–423.