To review the indication of surgical treatment of solitary proximal end of femur osteochondromas, and present our experience as regards the approach for a complete and safe resection.
Material and methodA retrospective study of a series of 6 symptomatic solitary proximal end of femur osteochondromas treated by en bloc resection by means of a single anterior or posterior-lateral approach. The patients were followed up routinely, as well as contacted by telephone to find out their current status. The functional assessment was made using the Musculoskeletal Tumour Society (MSTS) scale. The main limitation of the study was the its low level of recommendation.
ResultsThere were no post-operative complications and, after a mean follow-up of 8 years (rang: 2–21 years), the clinical result was excellent or good in all cases, and there were no recurrences of the tumour.
DiscussionAlthough some authors have proposed femur head subluxation or luxation to expose the whole of the femur neck and head to facilitate the resection of the osteochondroma and the joint exploration, in our experience, this can be avoided in the majority of cases.
ConclusionsSurgical treatment of solitary proximal end of femur osteochondromas is mandatory, as is the detailed pre-operative study of each case. Depending on their implantation and extension, en bloc resection can be performed by a single wide approach without the need for hip luxation.
Repasar la indicación del tratamiento quirúrgico de los osteocondromas del extremo proximal del fémur y presentar nuestra experiencia con respecto al abordaje para una resección completa y segura.
Material y métodoEstudio retrospectivo de una serie de 6 osteocondromas solitarios sintomáticos del extremo proximal del fémur, tratados mediante resección en bloque a través de un único abordaje anterior o posterolateral. Los pacientes fueron seguidos rutinariamente, a la vez que contactados telefónicamente para saber de su estado actual. La evaluación funcional fue hecha según la escala de la Sociedad de Tumores Musculoesqueléticos (MSTS). La principal limitación del estudio fue su escaso grado de recomendación.
ResultadosNo hubo complicaciones postoperatorias y, al cabo de un tiempo medio de seguimiento de 8 años (rango: 2–21 años), el resultado clínico fue excelente o bueno en todos los casos. Tampoco hubo recidivas de la tumoración.
DiscusiónAunque algunos han propuesto la subluxación o luxación de la cabeza femoral para exponer la totalidad del cuello y la cabeza femoral y facilitar la resección del osteocondroma y la exploración intraarticular, en nuestra experiencia, en la mayoría de los casos puede evitarse.
ConclusionesEl tratamiento quirúrgico de los osteocondromas solitarios sintomáticos del extremo proximal del fémur es obligado, como lo es un estudio preoperatorio detallado de cada caso. Según su implantación y extensión, la resección en bloque del tumor puede realizarse a través de un único abordaje amplio sin necesidad de luxar la cadera.
Osteochondroma is the most common benign bone tumour. In the hip—whether solitary or in the context of multiple exostoses disease—these tumours represent 8% of the total1 and may be asymptomatic or symptomatic, in which case they must be removed.2–4 Sometimes they are treated to avoid the risk of a sarcomatous degeneration, which is relatively common at this seat.5 The purpose of this study was to review this condition on the basis of our experience, with its possible clinical manifestations and treatment.
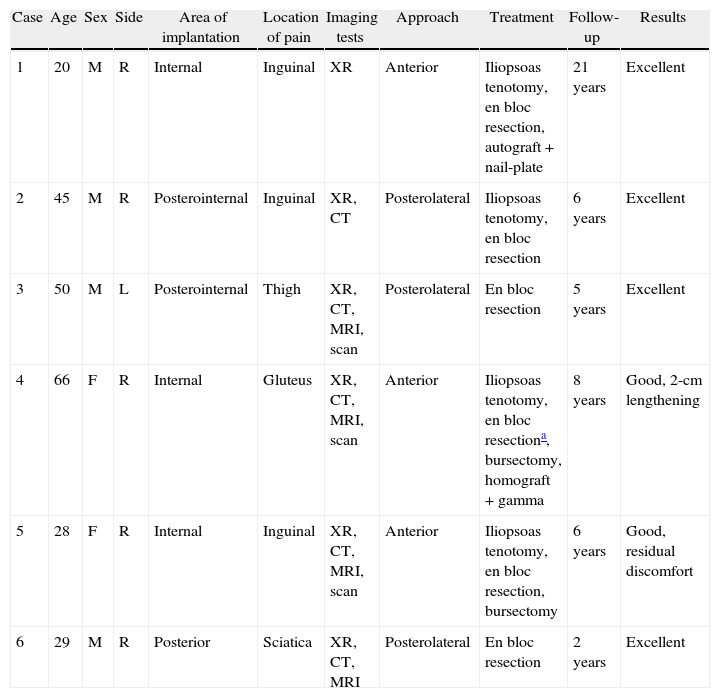
Materials and methodsWe conducted a retrospective review of a series of 6 symptomatic, solitary osteochondromas of the proximal femur treated between 1983 and 2007. There were 4 males and 2 females, ranging from 20 to 66 years of age (mean age: 39 years). Five of these were right-sided cases. Five of them also reported localised pain of mechanical rhythm and different intensities (2 due to iliopsoas bursitis), and 1 patient, the sixth, was reporting sciatica. The duration of symptoms varied from 5 months to 10 years, with a mean duration of 2 years. All patients had only slightly limited hip mobility on physical examination, although movement did increase the pain. Patient 6 showed abolition of the Achilles tendon reflex on the same side as the osteochondroma. The clinical data from the entire series are summarised in Table 1.
Summary of the series cases.
| Case | Age | Sex | Side | Area of implantation | Location of pain | Imaging tests | Approach | Treatment | Follow-up | Results |
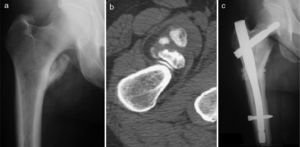
| 1 | 20 | M | R | Internal | Inguinal | XR | Anterior | Iliopsoas tenotomy, en bloc resection, autograft+nail-plate | 21 years | Excellent |
| 2 | 45 | M | R | Posterointernal | Inguinal | XR, CT | Posterolateral | Iliopsoas tenotomy, en bloc resection | 6 years | Excellent |
| 3 | 50 | M | L | Posterointernal | Thigh | XR, CT, MRI, scan | Posterolateral | En bloc resection | 5 years | Excellent |
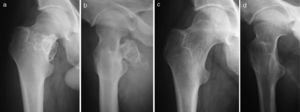
| 4 | 66 | F | R | Internal | Gluteus | XR, CT, MRI, scan | Anterior | Iliopsoas tenotomy, en bloc resectiona, bursectomy, homograft+gamma | 8 years | Good, 2-cm lengthening |
| 5 | 28 | F | R | Internal | Inguinal | XR, CT, MRI, scan | Anterior | Iliopsoas tenotomy, en bloc resection, bursectomy | 6 years | Good, residual discomfort |
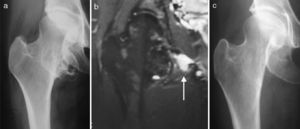
| 6 | 29 | M | R | Posterior | Sciatica | XR, CT, MRI | Posterolateral | En bloc resection | 2 years | Excellent |
MRI: magnetic resonance imaging; XR: X-rays; CT: computerised tomography.
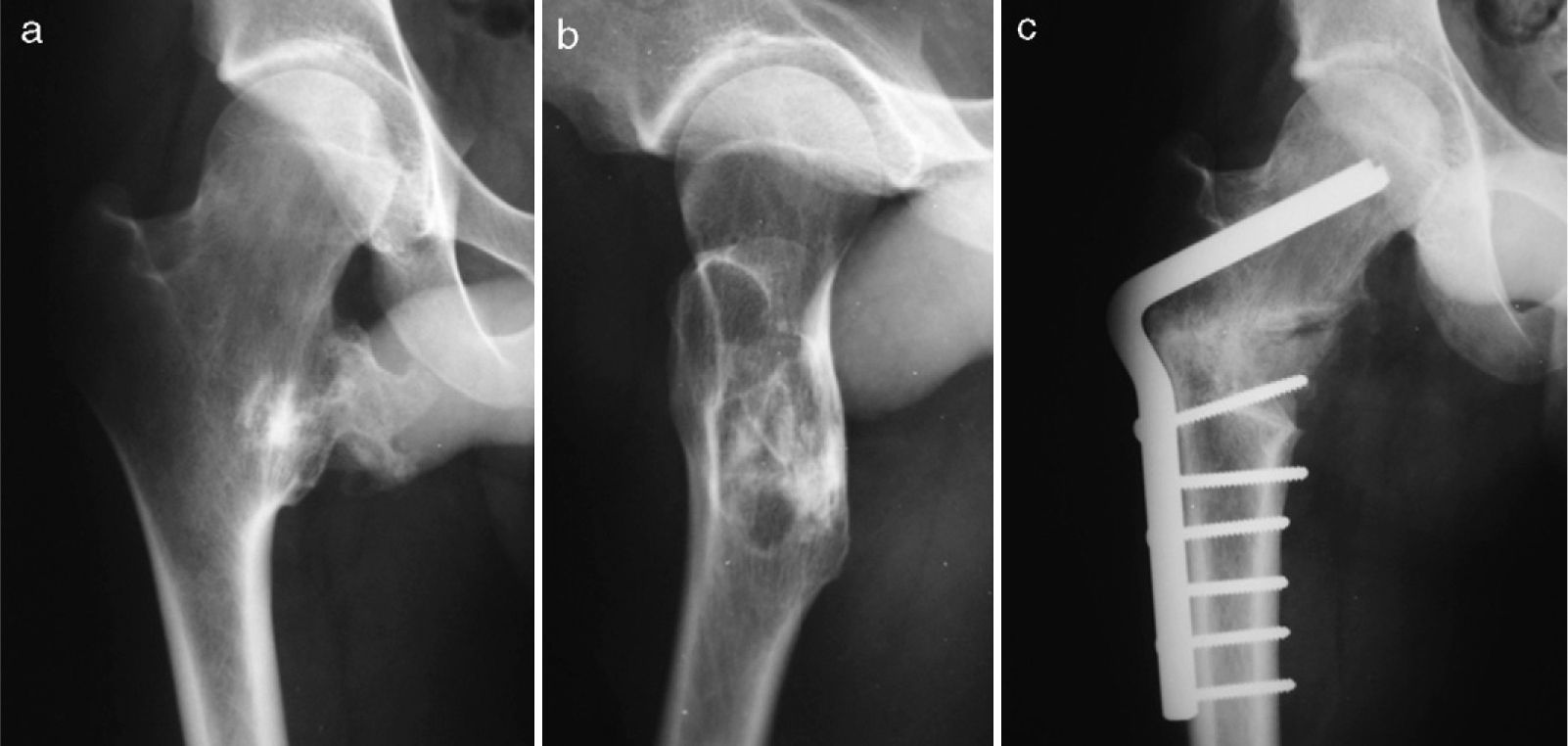
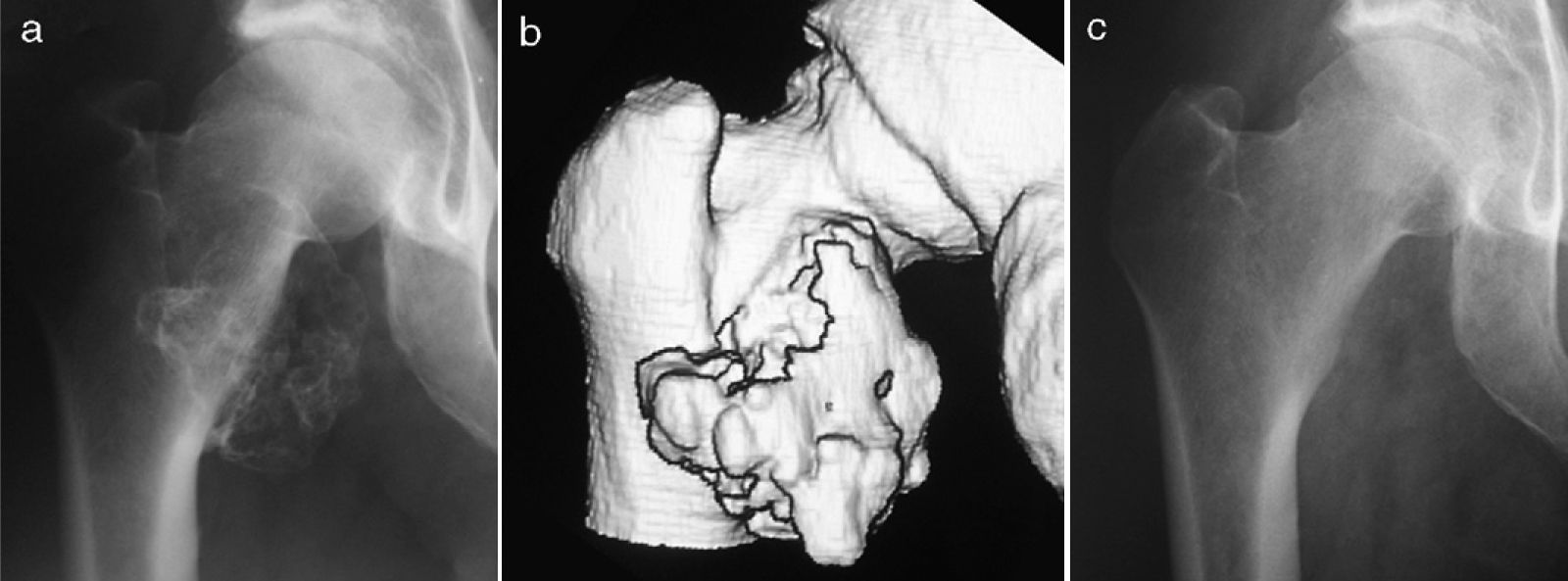
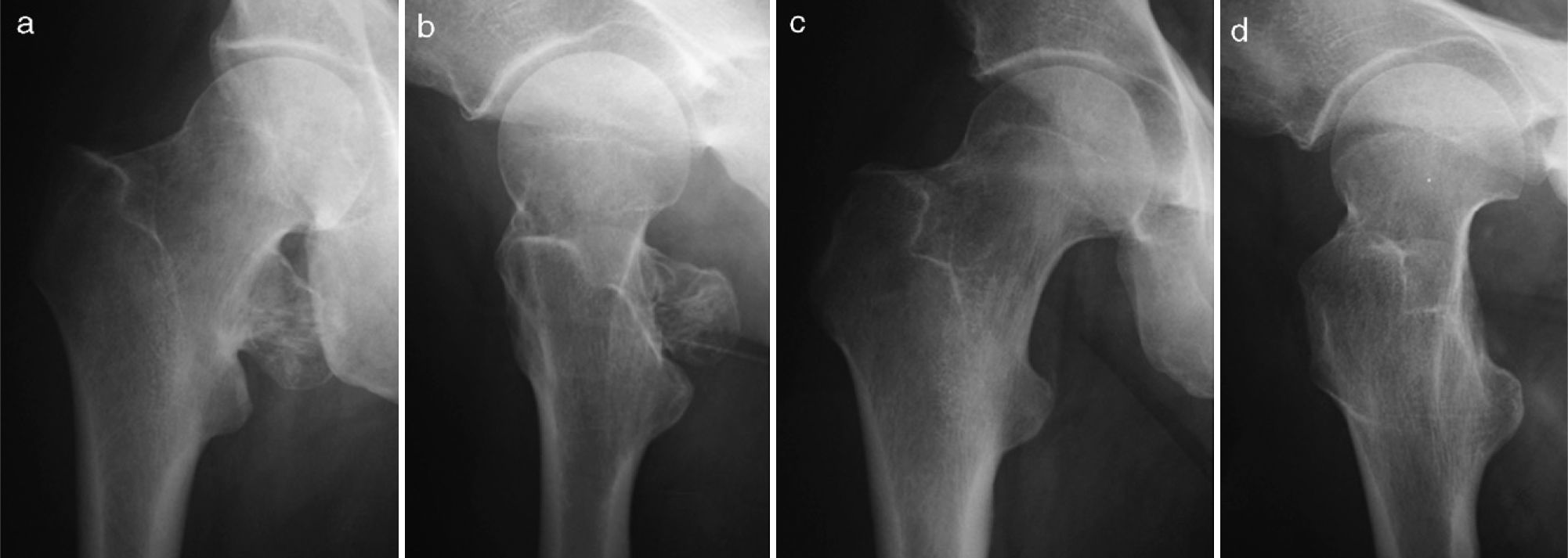
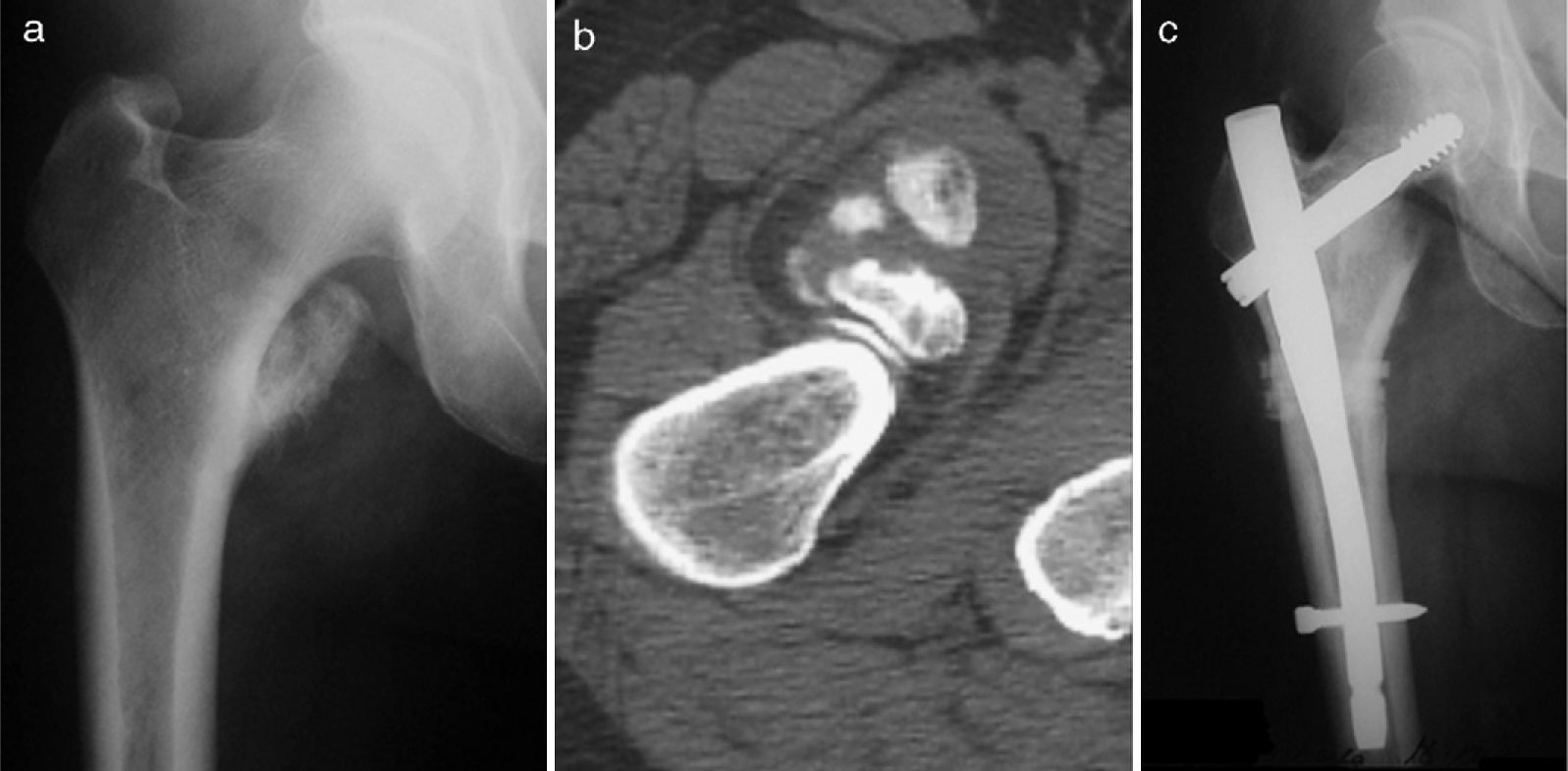
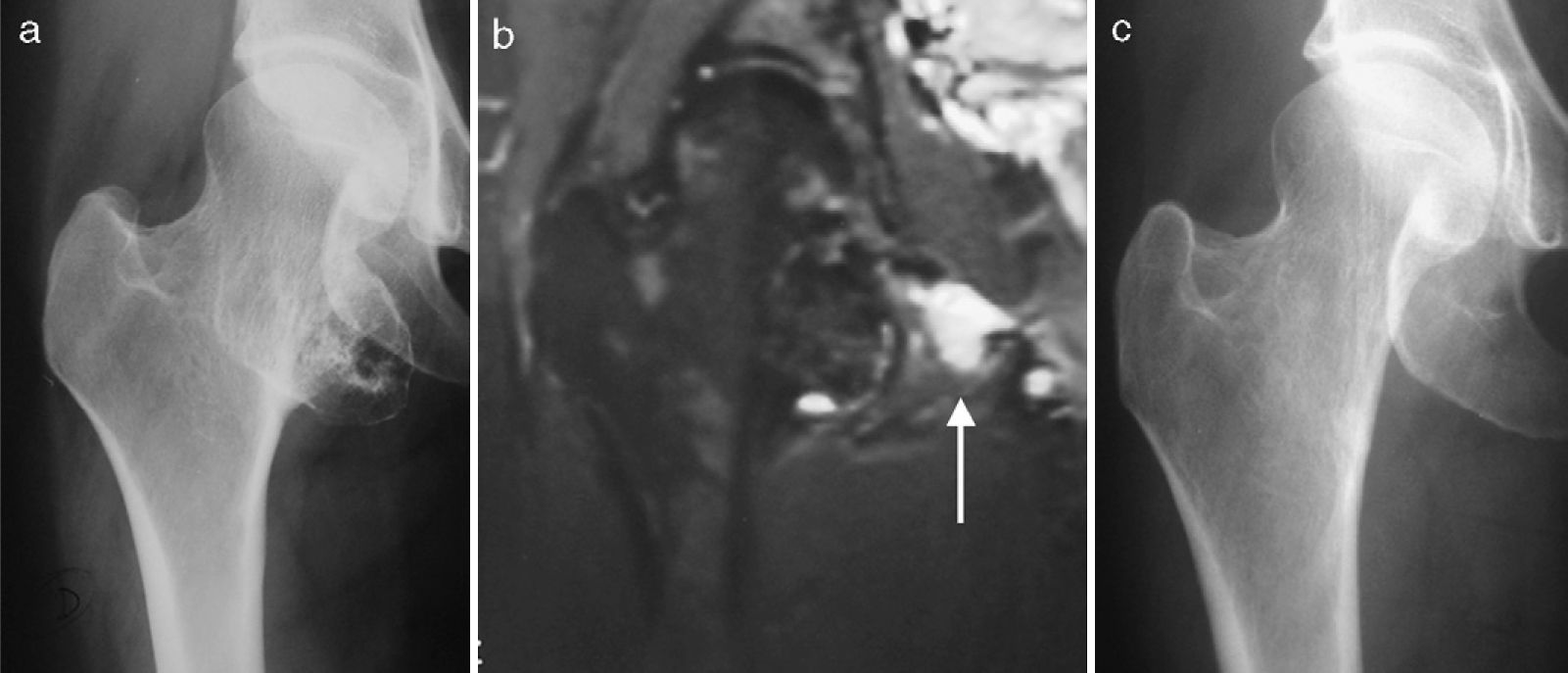
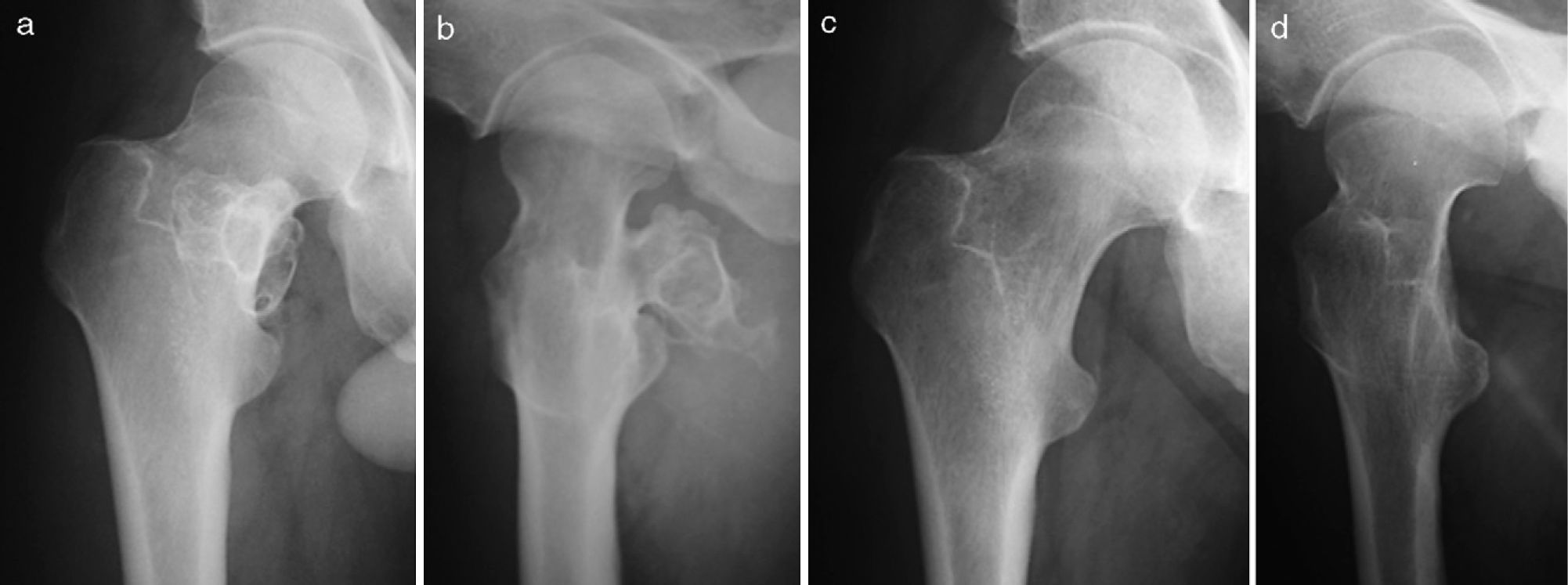
Conventional X-rays of the hip were taken on all patients, with complementary magnetic resonance imaging (MRI) and/or computerised tomography (CT) on the last 4 patients to confirm the diagnosis and accurately define the seat and extent of the lesion (Figs. 1–6). A bone scan was done on 3 patients. The images in all cases showed the typical osteochondroma pattern: sessile or pedunculated implantation in the internal (3 patients), posterointernal (2 patients) or posterior (case 6) area of the femoral neck and extending to the calcar area, all with the characteristic cartilaginous cap. One patient had a short, broad femoral neck with a 2.3-cm shortening of the leg (case 1) (Fig. 1), and 2 patients had coxa valga (cases 1 and 5) (Figs. 1 and 5). None of the patients showed any signs of degenerative osteoarthritis. Cases 4 and 5 had an iliopsoas bursitis on MRI which, in the former, because of its features—irregular edges and calcifications that appeared to be satellites (Fig. 4)—raised some doubt as to the diagnosis.
Having signed the informed consent, all patients were put under regional or general anaesthesia and placed in either prone decubitus, with a small bolster under the buttock on the same side, or lateral decubitus position, depending on the approach chosen. We made a single incision in all cases: anterior (in the 3 cases of primarily medial implantation) or posterolateral (in the 3 cases of posterior or posteromedial implantation). When the tumour was reached, its base of implantation was exposed via a longitudinal capsulotomy, separating and protecting the adjacent soft structures. The base of the osteochondroma was then resected using straight and curved chisels; the patient's leg was rotated to facilitate this, and the morphology of the femoral neck and its vascularisation was spared, as well as the tumour's cartilaginous cap, which was not breached in any of the cases. Once the osteotomy was completed, the osteochondroma was carefully removed by blunt dissection using the surgeon's fingers. The edges of the osteochondroma base protruding on the femur were removed using a gouge that we guided by feel. If, in any of the cases, the iliopsoas tendon was cut, it was never reinserted.
A marginal en bloc resection along the tumour's base of implantation was done on all patients. In 2 patients (cases 1 and 4), the resection was widened to the lesser trochanter, and a graft (autologous and homologous) with nail-plate (Fig. 1) and gamma nail (Fig. 4) fixation was used for reconstruction. In case 4, an incomplete basicervical fracture occurred, which was fixed with the previously mentioned gamma nail; in addition, 2 Partridge bands were used to ensure stability of the homograft. In cases 1, 2, 4, and 5, the iliopsoas tendon was cut, and in cases 4 and 5, there was an associated iliopsoas bursectomy. The pathologist confirmed the diagnosis of osteochondroma in all cases, as well as the bursitis in cases 4 and 5.
All patients were permitted partial-weight-bearing ambulation in the immediate post-operative period, with full weight bearing after the first month, except in case 4, where this was delayed until the third month. No external supports were used in any of the cases. The patients were followed at 1, 3, 6, 12, and 24 months, at the same time they were contacted by phone to find out about their current condition. The Musculoskeletal Tumour Society (MSTS) rating scale was used for the functional evaluation relative to pain, functional limitation, walking distance, use of supports, emotional acceptance, and limp.6
The study's primary limitation, arising from its small case series, was a low grade of recommendation (Grade C in the Oxford Centre for Evidence-Based Medicine (CEBM) document), and a low level of evidence (CEBM level 4). However, this methodological limitation is unavoidable in tumour pathology studies, where the incidence is very low, as was the case in our study. This would also explain why the seats, surgical approaches, and surgical techniques complementary to the tumour resection are heterogeneous—and this may be considered another limitation of the study. The final limitation would be the lack of standardisation in ancillary diagnostic testing. The reason for the inconsistency in testing was that a long period of time intervened between the first and subsequent cases, and some of the tests were not readily available more than 20 years ago at our medical centre; however, a good-quality, simple X-ray is enough to diagnose an uncomplicated osteochondroma, and this was done in all of our cases. Tests were lacking in other cases because, at that time, they were not considered necessary.
ResultsApart from the intra-operative fracture in case 4 mentioned above, none of the patients had any reportable complication during the immediate post-operative period. At the end of a mean follow-up period of 8 years (range: 2–21 years), all patients had excellent or good clinical results on the MSTS rating scale; case 5 had residual inguinal discomfort, and case 4—the one that suffered an intra-operative basicervical fracture—had leg lengthening due to valgisation of the femoral neck and, as a result, an imperceptible limp that was compensated for with a lift. All patients reported that they were satisfied with the treatment results and were currently living a normal life. There were no tumour recurrences. X-rays showed that there was a proper resection in all cases; graft consolidation in the 2 cases where grafting was used; and healing of the basicervical fracture. There were no signs of coxarthrosis or avascular necrosis of the femoral head.
DiscussionThe proximal femur is a relatively common site for benign bone tumours: giant cell tumours, chondroblastomas, simple and aneurysmatic bone cysts, and fibrous dysplasias may originate there. Osteochondroma is diagnosed as a solitary lesion or as part of a hereditary multiple osteochondromatosis involving the hip in 30–90% of patients.4 Approximately 25% of these patients have growth anomalies—medial hyperostosis, femoral lateralisation, coxa valga, and progressive acetabular dysplasia—with the possibility of subluxation and dislocation of the hip and progressive deformity of the femoral head.7
Osteochondroma is the most common bone tumour and may be diagnosed in 3% of the general population.8 They typically originate in long bone metaphyses, usually in the proximity of the knee or in the proximal metaphysis of the humerus, and normally stop growing when skeletal maturity is reached. There are asymptomatic cases that remain undiagnosed or are discovered by chance—the majority—and others that present with symptoms related to the mass effect that would result from the lesion. In these cases, mechanical problems in adjacent joints, bursitis, tendonitis, and compression of vessels and nerves may be seen. They may also become symptomatic due to fracture of the pedicle or because of a malignant transformation.
It is estimated that malignant transformation—usually to a low-grade chondrosarcoma, generally in the pelvis, the trunk, or the proximal femur—occurs in 0.4–2% of patients with solitary forms of osteochondroma5,9; in multiples, it occurs in 5–25% of cases.5 In the hip, the incidence of sarcomatous degeneration of a solitary osteochondroma is estimated at 13.1%,5 and it is suspected because of tumour surface irregularities, radiolucent areas, heterogeneous mineralisation, and soft tissue masses with patchy calcifications on X-ray, as at other sites. On bone scan, a non-specific increase in uptake would be observed on the tumour surface and, on MRI, a cartilaginous cap more than 2cm thick. All these data, correlated to the clinical and histopathology data, would establish the diagnosis of this complication. There were no cases of sarcomatous degeneration in our series, although it was suspected in case 4 because of tumour surface irregularities and the presence of calcifications.
The symptoms that may present in an osteochondroma of the proximal femur, as well as in a sarcomatous transformation, include pain, limp, and limitation of coxofemoral mobility due to tendonitis or iliopsoas or iliotibial band bursitis.10 Other times, there is joint blocking due to direct contact between the tumour and the pelvis; in addition, there may be femoral-acetabular impingement and labral injuries.4,11,12 Neurovascular compression and, rarely, urinary compression have also been described as complications. Arterial pseudoaneurysm, femoral artery occlusion and, in theory, injury of the branch supplying the femoral head would be possible, with the resultant avascular necrosis, as well as a compressive neuropathy, such as occurred in case 6 of our series.
One of the causes of mechanical pain—sometimes radiating along the anterior aspect of the thigh and occasionally associated with an audible click in the hip area, with or without limitation of hip mobility—is iliopsoas bursitis, often in conjunction with an iliopsoas tendonitis (“snapping hip syndrome”).13–15 This bursitis, which in some published articles was confused with a sarcomatous degeneration8,16—as it could have been in case 5 of our series—results from inflammation of the corresponding bursa. At 5–7cm long and 2–4cm wide, the iliopsoas bursa is the largest in the human body; it is situated between the iliopsoas musculotendinous junction and the pelvic ring, and it may extend distally to the lesser trochanter.17 It is present bilaterally in 98% of normal adults and communicates with the hip joint in 14% of them.13,14 In our series, 2 patients (cases 4 and 5) had an iliopsoas bursitis that was removed following a partial iliopsoas tenotomy—a procedure proposed by Schaberg et al.,15 which facilitates the bursectomy and is frequently required because the osteochondroma is inserted at that location.
A symptomatic osteochondroma of the proximal femur is always treated surgically, and the treatment is exactly the same no matter where in the skeleton this tumour occurs: a marginal en bloc resection along its base of implantation, which ensures good results in the absence of complications. To minimise the risk of local recurrence, effort should be made to avoid an intralesional “piecemeal” resection, which is sometimes performed because of the size of the tumour.18 For the same reason, arthroscopic tumour resection—recently proposed for an osteochondroma of the greater trochanter or a small osteochondroma with femoral-acetabular impingement and labral injuries,11,12 which could be repaired in the same surgical procedure—should be ordered with great caution and in very select cases. Other risks one should attempt to avoid, given this particular tumour location, are avascular necrosis of the femoral head, secondary to damage to its vascular supply, and iatrogenic fracture, which occurred in 1 of our patients but healed with no sequelae other than leg lengthening from valgisation of the femoral neck.
In every case, the surgical approach must expose the lesion well enough to facilitate its resection. Nowadays, CT scan and MRI are crucial as aids for not only the diagnosis but also the surgical approach because they give the exact implantation of the tumour and its relationships to adjacent structures.
Some have suggested that the femoral head be subluxed or dislocated to expose the entire femoral head and neck and facilitate resection of the osteochondroma and the intra-articular examination.4,18 In our experience, however, a single wide and precise incision, based on thorough study of the implantation and extent of the tumour, would suffice—with prior osteotomy of the greater trochanter and protection of the deep branch of the medial femoral circumflex artery, which would be achieved with a small posterior capsulotomy in select cases.4 In cases where the images appear to rule out femoral-acetabular impingement and there is no need to visually examine the labrum or the intra-articular condition of the hip, marginal en bloc resection of an osteochondroma of the proximal femur can be accomplished without dislocating the hip, in most cases, through use of the following important techniques: rotation of the leg during the procedure, blunt dissection with the surgeon's finger, and the use of curved instruments for the osteotomy. In any event, it has been demonstrated anatomically that the femoral head may be dislocated up to 11cm, leaving the external obturator muscle inserted on the femur, without significant vascular damage.
In conclusion, a solitary, symptomatic osteochondroma of the proximal femur must be treated surgically, with a detailed pre-operative workup in every case. Depending on its implantation and extent, en bloc resection of the tumour may be performed via a single wide surgical incision, in combination with intra-operative techniques and special curved instruments, with no need to dislocate the hip.
Level of evidenceEvidence Level IV.
Conflicts of interestThe authors have no conflicts of interest to declare.
Ethical DisclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidencialidad de los datos. Los autores declaran que han seguido los protocolos de su centro de trabajo sobre la publicación de datos de pacientes y que todos los pacientes incluidos en el estudio han recibido información suficiente y han dado su consentimiento informado por escrito para participar en dicho estudio.
Derecho a la privacidad y consentimiento informado. Los autores han obtenido el consentimiento informado de los pacientes y/o sujetos referidos en el artículo. Este documento obra en poder del autor de correspondencia.
Please cite this article as: Ramos-Pascua LR, et al. Osteocondromas solitarios del extremo proximal del fémur. Indicación y resultados de la resección en bloque sin luxación de la cadera. Rev esp cir ortop traumatol. 2012;56(1):24-31..