To evaluate the results of surgical treatment of displaced acetabular fractures, and to discern which variables influence the final radiological and clinical outcomes.
MethodsWe retrospectively analysed 23 patients who underwent open reduction and internal fixation of acetabular fracture with a mean age of 40.4 years (17–72 years). Mean follow-up was 4 years (1.5–7.5 years). According to Judet and Letournel classification, we operated 10 simple fractures (43.5%) and 13 complex fractures (56.5%), with both-column fractures being the most common type (8 hips). We evaluated the quality of reduction achieved, the clinical results and the occurrence of coxarthrosis.
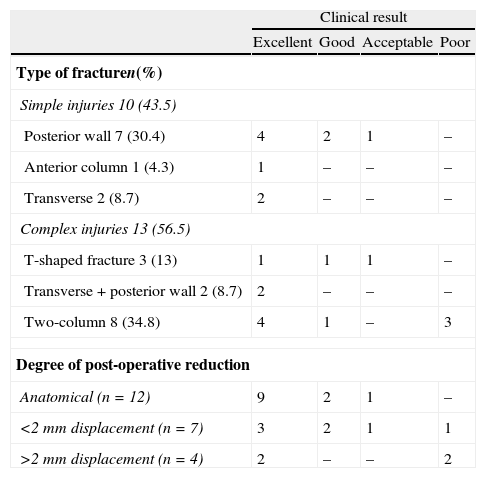
ResultsWe obtained anatomic reduction of the lesion in 12 cases (52%), in 7 patients (30%) residual displacement was less than 2mm, and in 4 patients (17%), it was greater than 2mm. According to Harris’ score, the clinical outcome was excellent or good in 18 cases (78%) and fair or poor in 5 (22%), getting worse in complex fractures and when we do not reach an anatomic reduction of the injury. Six patients (26%) developed moderate or severe degenerative changes during follow-up. The degree of postoperative reduction obtained was identified as the main predictor of the development of post-traumatic osteoarthritis.
Discussion and conclusionsThe acquisition by open reduction and internal fixation of an accurate congruence between the femoral head and acetabulum is essential to achieve good long-term results.
Evaluar los resultados del tratamiento quirúrgico de las fracturas desplazadas de acetábulo. Discernir que variables influyen en el resultado clínico y radiológico final.
Material y métodosAnalizamos de forma retrospectiva 23 pacientes intervenidos de fractura acetabular mediante reducción abierta y fijación interna, con una edad media de 40,4 años (17-72 años). El seguimiento medio fue de 4 años (1,5-7,5 años). Según la clasificación de Judet y Letournel intervenimos 10 fracturas simples (43,5%) y 13 complejas (56,5%), siendo la fractura de ambas columnas la más frecuente (8 casos). Valoramos la calidad de la reducción obtenida, los resultados clínicos y la aparición de coxartrosis.
ResultadosObtuvimos una reducción anatómica de la lesión en 12 casos (52%), en 7 (30%) el desplazamiento residual fue menor de 2mm y en 4 pacientes (17%) mayor de 2mm. Según la escala de Harris, el resultado clínico fue excelente o bueno en 18 casos (78%) y aceptable o pobre en 5 (22%), obteniendo peores resultados en fracturas complejas y cuando no alcanzamos una reducción anatómica de la lesión. Seis pacientes (26%) habían desarrollado cambios degenerativos moderados o severos al final del seguimiento. El grado de reducción postquirúrgica obtenida fue identificado como el principal predictor de desarrollo de coxartrosis postraumática.
Discusión y conclusionesLa obtención mediante reducción abierta y fijación interna de una correcta congruencia entre la cabeza femoral y el acetábulo es esencial para lograr buenos resultados a largo plazo.
Acetabular fractures are relatively uncommon injuries. With an approximate annual incidence of 3 cases per 100,000 inhabitants,1 they constitute 0.3–6% of all fractures.2 They are usually seen in the context of multiple trauma patients, the most common cause of which is traffic accidents.3
Although conservative treatment with traction and unloading may yield acceptable results in certain patients and fracture patterns,4,5 surgery is the treatment of choice in most cases,6–10 the indications for it being well-established: fractures with joint incongruence,6,8 with involvement of the weight-bearing surface (defined by acetabular roof arc measurements11 or their equivalent on axial slices of the computerized axial tomography [CAT scan]),12 or with associated coxofemoral instability.8,13 Functional results are closely tied to the degree of post-operative reduction obtained,6–10,14 but other factors, such as age,6–9 type of fracture,6–10,14 surgery delay time,6–9 and the presence of chondral damage to the femoral head6–10 have been suggested as variables that modify the final result.
Evolution toward post-traumatic osteoarthritis is the most common complication of acetabular fracture, with an incidence close to 27%.3 Other complications associated with this type of injury and its treatment are sciatic nerve paralysis, development of heterotopic ossifications, and necrosis of the femoral head.15
The objectives of this study were to analyse the results of surgical treatment in our first series of displaced acetabular fractures and to identify the variables that directly influenced these results.
Materials and methodsWe identified 30 consecutive patients who had undergone surgery for acetabular fracture between May of 2003 and June of 2009. Of these patients, 7 were excluded from the study—2 because of previous surgery on the same hip, 2 because they had moved away, and 3 because they had been transferred back to their referring hospital after the surgery. We are not aware that any patients excluded for lack of follow-up have suffered complications secondary to the acetabular fracture. Our series retrospectively analysed the clinical and radiographic results of the remaining 23 cases. Once the Ethics Committee at our hospital granted its approval, data was obtained by reviewing the medical records.
Demographic data and type of fractureOf the 23 patients, there were 15 males and 8 females, with a mean age of 40 years, the age range being 17–72 years. The mechanism of injury was high-energy trauma in 22 cases (14 traffic accidents and 8 falls from a height) and low-energy trauma in 1 case (a fall on the patient's own level).
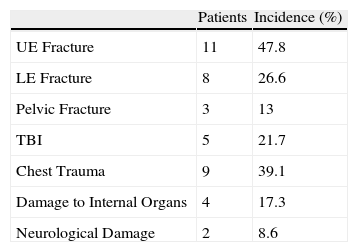
There were associated injuries in 69.5% of the cases (Table 1). Two patients had neurological symptoms upon admission: in 1 case, permanent damage to the sacral roots, with sphincter incontinance and patchy hypaesthesia at the L5-S1 radicular level, and in 1 case, sciatic nerve injury, from which the patient had fully recovered 3 months later.
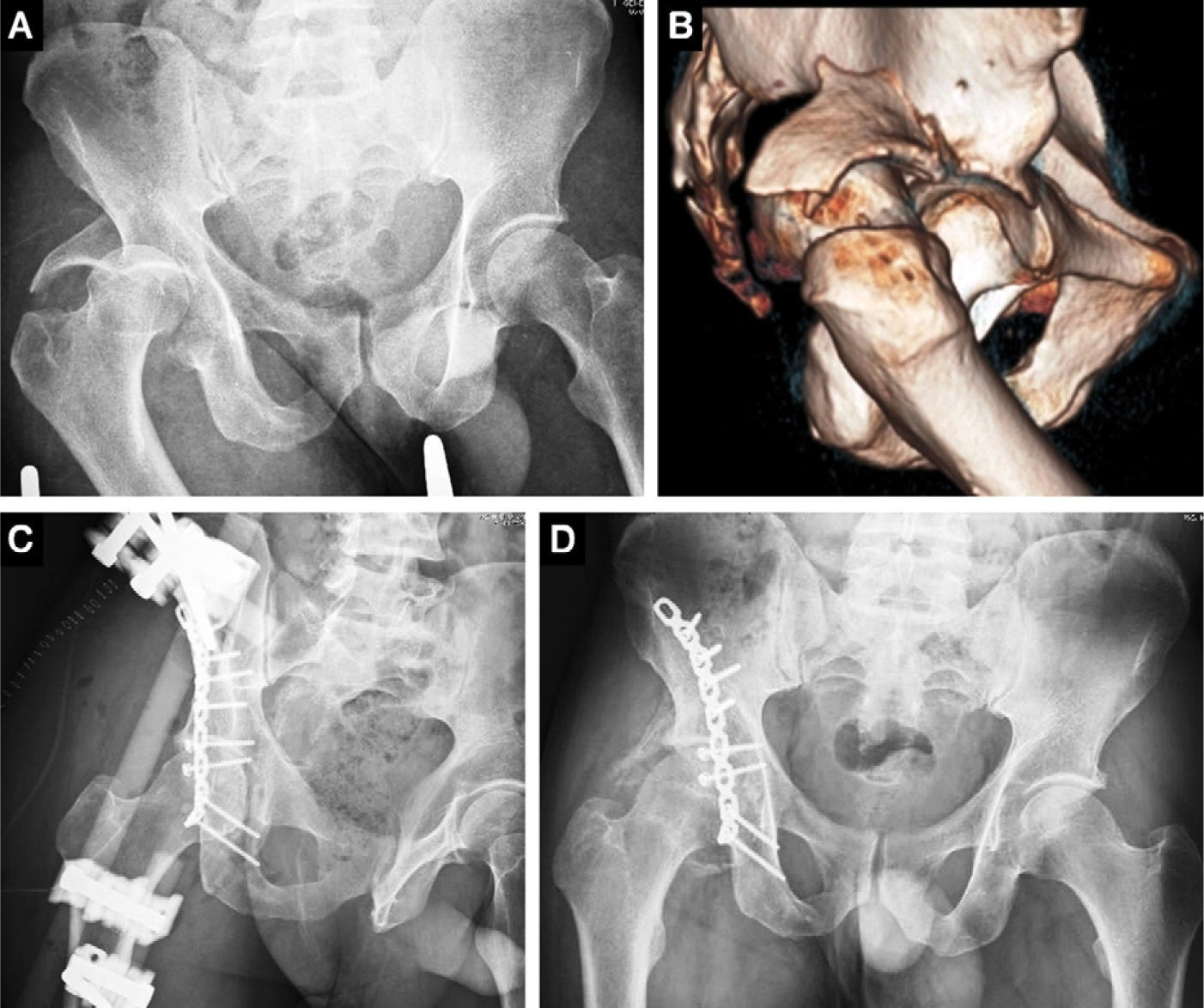
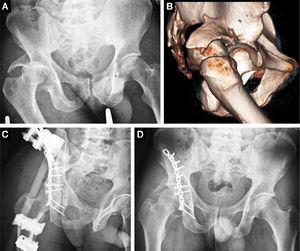
The right acetabulum was fractured in 12 cases and the left acetabulum in 11 cases. The fractures were classified according to Judet and Letournel16 using standard radiographic projections (anteroposterior, iliac oblique, and obturator oblique) and CAT scan (Table 2). In 7 cases (30%), the fracture was accompanied by hip dislocation—4 posterior and 3 central—of which 6 underwent closed reduction within 24h of admission. A case of posterior dislocation, 1 month old, transferred from another hospital, required open reduction and arthrodiastasis via external fixator in the same surgical procedure as osteosynthesis of the fracture (Fig. 1).
Distribution of clinical results by type of fracture and degree of post-operative reduction.
| Clinical result | ||||
| Excellent | Good | Acceptable | Poor | |
| Type of fracturen(%) | ||||
| Simple injuries 10 (43.5) | ||||
| Posterior wall 7 (30.4) | 4 | 2 | 1 | – |
| Anterior column 1 (4.3) | 1 | – | – | – |
| Transverse 2 (8.7) | 2 | – | – | – |
| Complex injuries 13 (56.5) | ||||
| T-shaped fracture 3 (13) | 1 | 1 | 1 | – |
| Transverse+posterior wall 2 (8.7) | 2 | – | – | – |
| Two-column 8 (34.8) | 4 | 1 | – | 3 |
| Degree of post-operative reduction | ||||
| Anatomical (n=12) | 9 | 2 | 1 | – |
| <2mm displacement (n=7) | 3 | 2 | 1 | 1 |
| >2mm displacement (n=4) | 2 | – | – | 2 |
(A and B) Posterior wall fracture with associated 1-month-old coxofemoral dislocation. (C) Post-operative obturator X-ray. An external fixator was added to the osteosynthesis. (D) 20-month post-operative anteroposterior X-ray of the pelvis, no osteoarthritis of the hip, Brooker II heterotopic ossifications.
The criteria used to establish the indication for surgery were fractures with joint displacement of more than 2mm or involving the weight-bearing area of the roof,6,8 fractures with associated posterior coxofemoral instability,13 and fractures with incarcerated fragments between the two articular surfaces.
The mean time elapsed between injury and surgery was 11 days (range: 5–31). In only 5 cases (22%), the surgery was delayed more than 2 weeks because of either severe multiple traumas involving a lengthy stay in Intensive Care or the patient being transferred from another hospital.
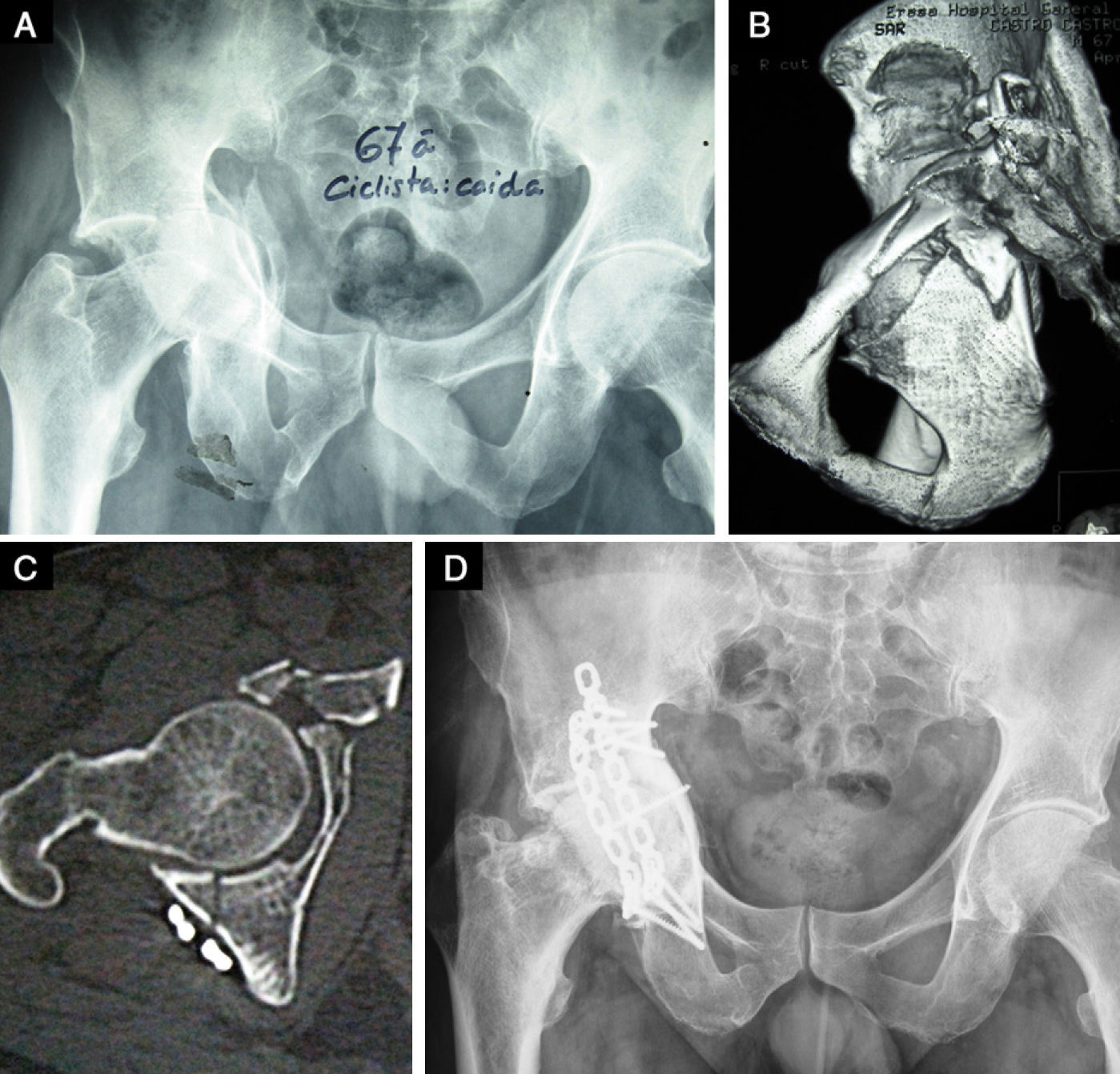
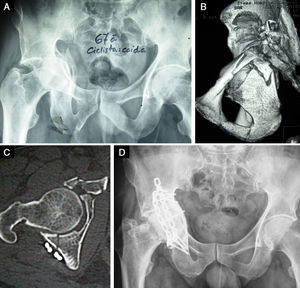
A posterior Kocher–Langenbeck approach was used in 11 cases (mean time: 116min), an anterior ilioinguinal approach in 7 cases (167min), and a combined anterior–posterior approach in 4 cases (230min). All patients on whom a combined approach was used had a both-column fracture (Fig. 2); the combined approach was done in a single surgical procedure in 2 cases and on a deferred basis in the other 2 cases. In a case of T-shaped acetabular fracture accompanied by sacral fracture, we performed a percutaneous fixation of both fractures. For the osteosynthesis, we used AO materials with reconstruction plates and 3.5-mm titanium screws. We did not use intra-operative neurophysiological monitoring.
(A) Both-column fracture in a 22-year-old female. The arrow points to the “spur sign” indicating the most distal part of the iliac wing that is still attached to the sacrum. (B) 3D reconstructions afford us an overall view of the injury. (C) Post-operative control at 36 months. Anatomical reduction. Mild osteoarthritis of the hip.
The mean length of admission was 23.6 days (12–53 days, median 19 days), and the mean length of stay post-operatively was 14.5 days (4–38 days, median 11 days). None of the patients received indomethacin prophylaxis or low-dose radiation to prevent the appearance of heterotopic ossifications. Progressive weight-bearing ambulation was initiated in the third month, depending on radiographic healing of the fracture.
Post-operative evaluationThe patients were clinically and radiographically evaluated at 4 weeks, 12 weeks, 6 months, and annually thereafter. The mean follow-up period was 4 years (1.5–7.5 years).
We used Harris’ functional evaluation scale for the clinical evaluation.17 The radiographic assessment included classic projections of the acetabulum. The degree of reduction achieved was divided into 3 categories18: anatomical reduction, displacement less than 2mm, and displacement more than 2mm. Heterotopic ossifications appearing were evaluated and classified according to Brooker et al.,19 and for the degree of radiographic osteoarthritis of the hip, the Tönnis classification was used.20
Statistical analysisWe used the SPSS program for Windows (version 15.0, SPSS, Chicago, IL). The non-parametric chi-square test and the T-test for independent data were used to detect possible association between variables. A P value of <.05 was considered statistically significant.
ResultsComplicationsIntra-operative: an injury due to traction on the femoral cutaneous nerve, from which the patient has not recovered, having an area of hypaesthesia on the lateral aspect of the thigh.
Post-operative: a superficial Staphylococcus epidermidis infection of the surgical wound and a generalized sepsis, the latter in a patient with both-column acetabular fracture and bilateral open humerus fractures. Both infections resolved with specific intravenous antibiotic therapy.
Post-operative reductionWe obtained anatomical reduction of the fracture in 12 cases (52%); in 7 patients (30%), the displacement was less than 2mm, and in 4 patients (17%) it was greater than 2mm.
We found an association between the type of fracture and the degree of reduction obtained, the probability of achieving an anatomical reduction being reduced in complex injuries (P=.019). Anatomical reduction was achieved in only 23% of complex injuries, compared to 90% of simple injuries.
The percentage of anatomical reductions was lower in patients over 40 years of age due to their poorer bone quality, but this was not a statistically significant difference (P=.059). Only 4 out of 12 fractures (33%) were anatomically reduced in patients over 40 years of age, compared to 8 out of 11 (73%) in patients under 40 years of age. We also found that, following injury, the surgery delay time made no significant difference in the degree of reduction obtained.
Clinical resultsAccording to the Harris scale,17 the results we obtained were excellent in 14 patients (61%), good in 4 patients (17%), acceptable in 2 patients (9%), and poor in 3 patients (13%) (Table 2). At the end of the follow-up period, 4 patients had moderate or severe pain (17%), 9 had limited mobility in the hip (39%), 5 were routinely using a cane (22%), and 16 were able to walk a distance of more than 6 blocks (70%).
In our study, simple fractures had a better functional prognosis than complex fractures: while the simple fractures scored a mean of 92 points on the Harris scale,17 the mean score for complex fractures was 84.5 points (P=.04).
The degree of reduction obtained was also a determining factor in the final clinical results (P=.016), the percentage of good and excellent results being higher for anatomically reduced fractures (Table 2). Neither the patient's age nor the presence of associated injuries made significant differences in the functional evaluation.
Radiographic resultsOf the 23 patients evaluated, 5 patients (22%) developed heterotopic ossifications that were Brooker class II or more. Heterotopic ossifications appeared more frequently in those cases where we approached the fracture via the external table of the ilium (Kocher–Langenbeck and combined approach). Of the 15 cases where we used one of these approaches, 8 (53%) developed heterotopic ossifications (3 Brooker class I, 3 class II, and 1 class III), compared with only 2 (28%) of the 7 cases where an ilioinguinal approach was used (1 Brooker class I and 1 class II).
On the final radiographic evaluation, no degenerative changes were seen in 12 cases (52%), minimal osteoarthritic changes (Tönnis I) in 5 cases (22%), moderate changes (Tönnis II) in 4 cases (17%), and complete loss of the joint space (Tönnis III) in 2 cases (9%).
Post-operative reduction of the fracture is associated with the development of osteoarthritis of the hip (P<.001). Only 2 out of 18 cases (11%) that had a satisfactory reduction (anatomical or displacement less than 2mm) developed moderate to severe degenerative changes, but all patients (100%) with a post-operative displacement of more than 2mm progressed toward an advanced osteoarthritis (Fig. 3).
Among our patients, there were no cases of avascular necrosis of the femoral head. At this time, none of the patients who have developed an obvious osteoarthritis of the hip are showing enough clinical signs to warrant replacement with a prosthesis.
DiscussionCongruence between the femoral head and the acetabulum is crucial to preserving good joint function and preventing the development of a post-traumatic osteoarthritis of the hip.7 The objective of surgical treatment should be to achieve a stable anatomical reduction of the fracture.6
Proper classification of the fracture is essential for surgical planning, has prognostic value, and facilitates the comparative analysis of results from different hospitals. The classification system proposed by Judet and Letournel16 is the most extensive and has good inter- and intra-observer concordance.21
There is no unanimity as to the appropriate length of time until surgery. There is evidence, however, that anatomical reduction is more difficult to achieve and that clinical results are worse if surgical treatment of the fracture is delayed more than 2 or 3 weeks after the initial trauma.22,23 In our series, the degree of reduction obtained was independent of how long it was delayed.
Of the 23 fractures, 19 (83%) were resolved via a single surgical approach. In the remaining 4 cases, we were not able to reduce all the fractures via a single approach and opted for a combined anterior and posterior incision, avoiding wide approaches such as the iliofemoral approach because of their higher morbidity.
In only 1 case was a CAT scan used to assess post-operative reduction (Fig. 3). This could constitute a limitation of our study, in view of the evidence that reductions classified radiographically as anatomical show displacement at the articular surface when evaluated by CAT scan.7 We achieved anatomical reduction of the fracture in 12 cases (52%). Although these results are slightly inferior to those of more extensive series that have been published,6–9 they are consistent with those published by Matta and Merrit,24 who report anatomical reductions in close to 50% of their first 20 surgical cases.
The development of osteoarthritis is the most common complication of acetabular fracture6 and is directly related to the post-operative reduction obtained. The incidence of moderate to severe osteoarthritis of the hip in our series was 26%—very close to the 26.6% published by Giannoudis et al.3 in their meta-analysis but lower than that in series with a lengthier follow-up, such as that of Briffa et al.,9 who report 38% having osteoarthritis at 11.3 years. We believe that, given a longer follow-up period, osteoarthritis of the hip may develop with perfectly reduced fractures.
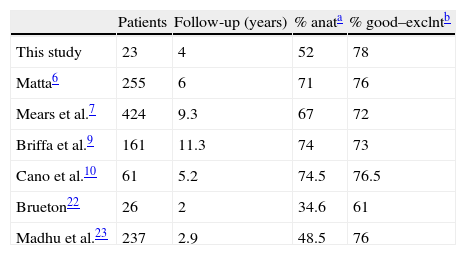
Our clinical results are comparable to those of other authors, even having achieved a lower rate of anatomical reductions (Table 3). We believe it is possible to obtain excellent functional results—even if the reduction is not satisfactory—as long as the joint displacement is situated outside the weight-bearing surface of the acetabulum. Some authors7,9 have suggested that an anatomical surgical reconstruction does not always correlate to a good clinical result, owing to factors beyond our control, such as chondral damage caused by the initial trauma.
ConclusionIn acetabular fractures, the primary objective of surgical treatment is anatomical reduction of the fracture. Added to the difficulty this involves is the relative infrequency of these fractures. Establishing referral centres specialized in the management of these patients should be a short-term priority, for this would facilitate the creation of treatment protocols and minimize the detrimental effects of the learning curve.
Level of evidenceEvidence Level IV.
Conflicts of interestThe authors have no conflicts of interest to declare.
Ethical DisclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors will declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors must have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Please cite this article as: Estrems-Díaz V, et al. Fracturas de acetábulo. Resultados a corto plazo. Rev esp cir ortop traumatol. 2012;56(1):17-23.