The objective of this study was to determine the major risk factors for bleeding in patients with a pertrochanteric fracture in order to plan the transfusion strategy and to overcome the problem of post-surgical anaemia. Various factors were analysed, including the taking of anticoagulant and/or anti-platelet treatment, the type of fracture, type of anaesthesia, and the type of osteosynthesis used.
Materials and methodsA retrospective study was performed on 307 patients over 75years old, operated on between the years 2005 and 2009.
ResultsBleeding was less in simple, non-comminuted fractures, in patients operated on using a mini-invasive screw-plate, in women, and in patients who did not take any anticoagulant or antiplatelet treatment. The only statistically independent factor associated with bleeding was fracture comminution.
DiscussionIn this study we have seen that patients operated on using a Gamma® and DHS® nail are transfused more than in those operated on using PPCP® and Traumax® plate. Evans fractures 1 or 2, A 2.2, or A 2.3, cervical-trochanteric or simple pertrochanteric fractures bled less than Evans 4 or 5, the rest of the type AO fractures, and the complex pertrochanteric fractures.
ConclusionsThe precise analysis of the type of fracture is important, particularly in older and fragile patients, to be able to anticipate the need for transfusion. Thus useless and costly, and sometimes dangerous transfusions may be avoided.
El objetivo de este estudio era buscar los factores de riesgo de sangrado mayor en pacientes con una fractura pertrocantérica para planificar la estrategia transfusional y luchar contra la anemia posquirúrgica. Se analizaron diferentes factores como: la ingesta de tratamiento anticoagulante y/o antiagregante, el tipo de fractura, el tipo de anestesia y el tipo de osteosíntesis empleada.
Material y métodosSe realizó un estudio retrospectivo sobre 307 pacientes intervenidos con más de 75 años de edad entre el 2005 y el 2009.
ResultadosEl sangrado fue menor en las fracturas simples no conminutas, en los pacientes intervenidos mediante un tornillo-placa miniinvasivo, en las mujeres y en los pacientes que no tomaban ningún anticoagulante o antiagregante. El único factor estadísticamente independiente relacionado con el sangrado era la conminución fracturaria.
DiscusiónEn este estudio hemos visto que los pacientes intervenidos con clavo Gamma® y DHS® se transfunden más que en los intervenidos con PPCP® y placa Traumax®. Las fracturas Evans 1 o 2, A 2.2. o A 2.3, las cervicotrocantéricas o pertrocantéricas simples sangraban menos que las Evans 4 o 5, el resto de los tipo AO y las fracturas pertrocantéricas complejas.
ConclusionesEl análisis preciso del tipo de fractura es importante, especialmente en los pacientes mayores y frágiles, para poder anticiparse a la necesidad de transfusión. Así se podrían evitar las transfusiones inútiles, costosas y a veces peligrosas.
Fractures of the upper femur are common in elderly patients1 and are seen more frequently in women. For a woman 75–85years of age, the risk of an upper femur fracture is 11/1000; for women over 85years of age, it is 33/1000.2,3
An upper femur fracture may make an already dependent patient even more dependent and may cause an autonomous patient who was living at home to become a dependent patient.4
Osteosynthesis is currently the predominant treatment for upper femur, wrist, and upper humerus fractures.3
The surgery-related factors that are essential to patients retaining their original autonomy are the promptness of treatment, the quality of the reduction, the stability of the mounting, and the absence of complications.5
The surgery is associated with significant blood loss, moderate tissue damage, and exacerbation of pre-existing conditions in these elderly patients.3,6
There is a high morbimortality associated with trochanteric fractures, the mortality rate for these patients being 15–25% within the first 6months.7
To limit these figures, the surgery should allow for a prompt recovery and early ambulation.
Among the numerous factors that could mean a delay in meeting these objectives is the development of marked post-operative anaemia.4
There are transfusion protocols for these cases, but they are costly and have side effects.
The objective of this study was to identify the factors that increase the risk of bleeding in patients with pertrochanteric fracture so that transfusion strategies may be planned and post-operative anaemia may be prevented.
Materials and methodsA retrospective, continuous study was conducted to analyse global blood loss in patients over 75years of age who had undergone osteosynthesis for a trochanteric fracture.
The study included isolated trochanteric fractures in subjects over 75years of age and excluded pathological fractures and high-energy trauma. A total of 307 patients (307 fractures) were evaluated, their mean age being 85.3±6.3years (75–100.3). The sample was made up of 240 women and 67 men.
The surgeries were performed by 4 senior traumatologists from the Orthopaedics and Traumatology Service at Hospital de Rangueil (Toulouse) between 2005 and 2009.
Our treatment protocol for elderly patients with hip fracture included blood tests (chemistries, CBC, coagulation studies), an electrocardiogram, a chest X-ray, and Anaesthesia and Geriatrics consults so that the patient could undergo surgery as soon as possible.
The patient was started on standardized antibiotic and antithrombotic prophylaxis.
We looked at whether the patient was on anticoagulant and/or antiaggregant therapy, the type of fracture per the Evans and AO classifications, the type of anaesthesia, and the type of osteosynthesis used (sliding screw-plate or endomedullary nailing).
The Evans classification identifies types I and II as stable fractures and types III, IV, and V as unstable or comminuted fractures.
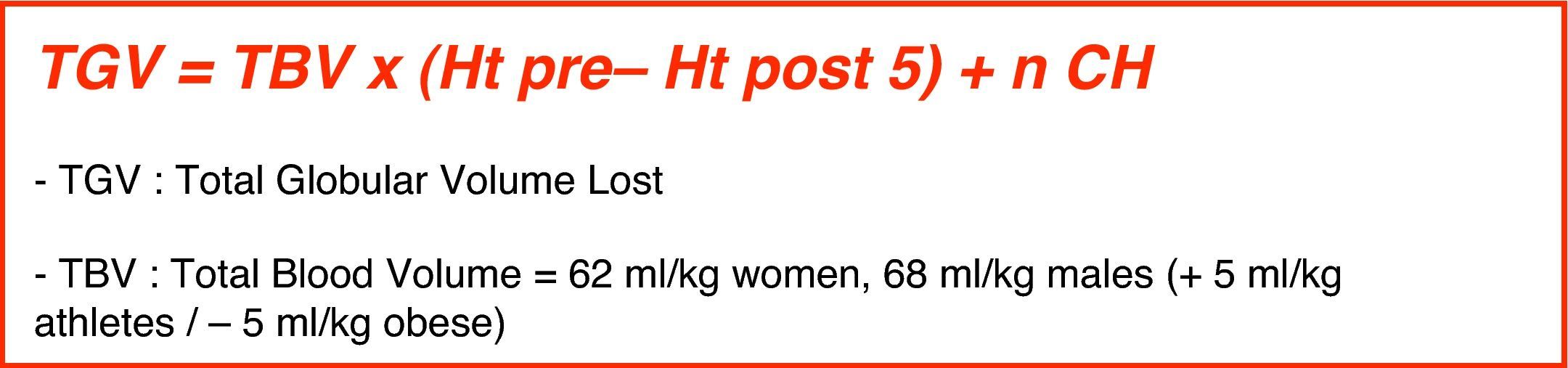
The total globular volume (TGV) lost was calculated using a standardized formula8 (Fig. 1) that took into account the patient's weight, the pre- and post-operative (on day 5) haematocrit, and the number of transfusions administered. The number of pre- and post-operative transfusions was recorded.
Calculation of the total globular volume lost using the Charrois et al.8 formula.
All the data were recorded and analysed using the SPSS® 17.0 statistics program.
Each variable was subjected to a descriptive and inferential study (mean, mode, median, standard deviation, confidence interval for the mean, minimum and maximum value) and a regression analysis (curvilinear model best fitting the time progression curve for each variable, coefficient of correlation, coefficient of determination, and predictability).
As a way to compare the 2 groups’ values for the same variable, we began with the Kolmogorov–Smirnov test to confirm that the variable fits a normal distribution and Levene's test to assess variance homogeneity. If a variable fits a normal distribution and was homogeneous, parametric tests were used to compare the 2 groups’ values for that variable.
If these 2 assumptions were not fulfilled, non-parametric tests for independent quantitative variables were used.
The degree of significance used in all cases was 95% (P<.05).
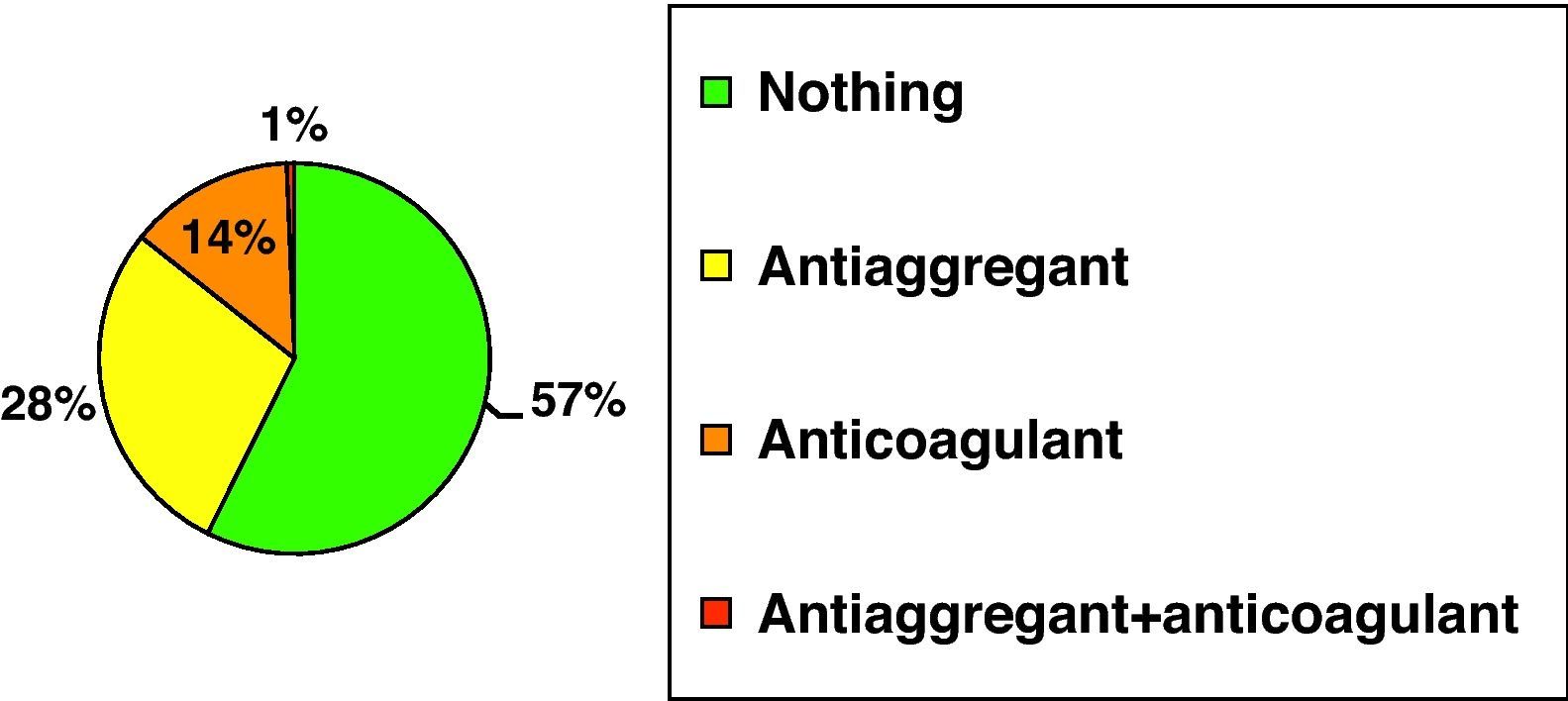
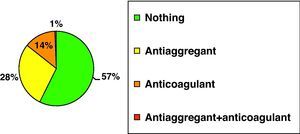
ResultsOf the patients studied, 43% were on antiaggregant and/or anticoagulant therapy (Fig. 2). It was considered antiaggregant therapy if the patient was taking acetylsalicylic acid (ASA), ticlopidine, or clopidogrel, and anticoagulant therapy if the patient was taking acenocoumarol or warfarin.
According to Ramadier's classification,9 24% of the patients had a complex pertrochanteric fracture, 24% a cervicotrochanteric fracture, and 52% a simple pertrochanteric fracture.
Based on the Evans classification, the fracture types were distributed as follows: Evans I (4%), Evans II (53%), Evans III (5%), Evans IV (17%), and Evans V (21%).
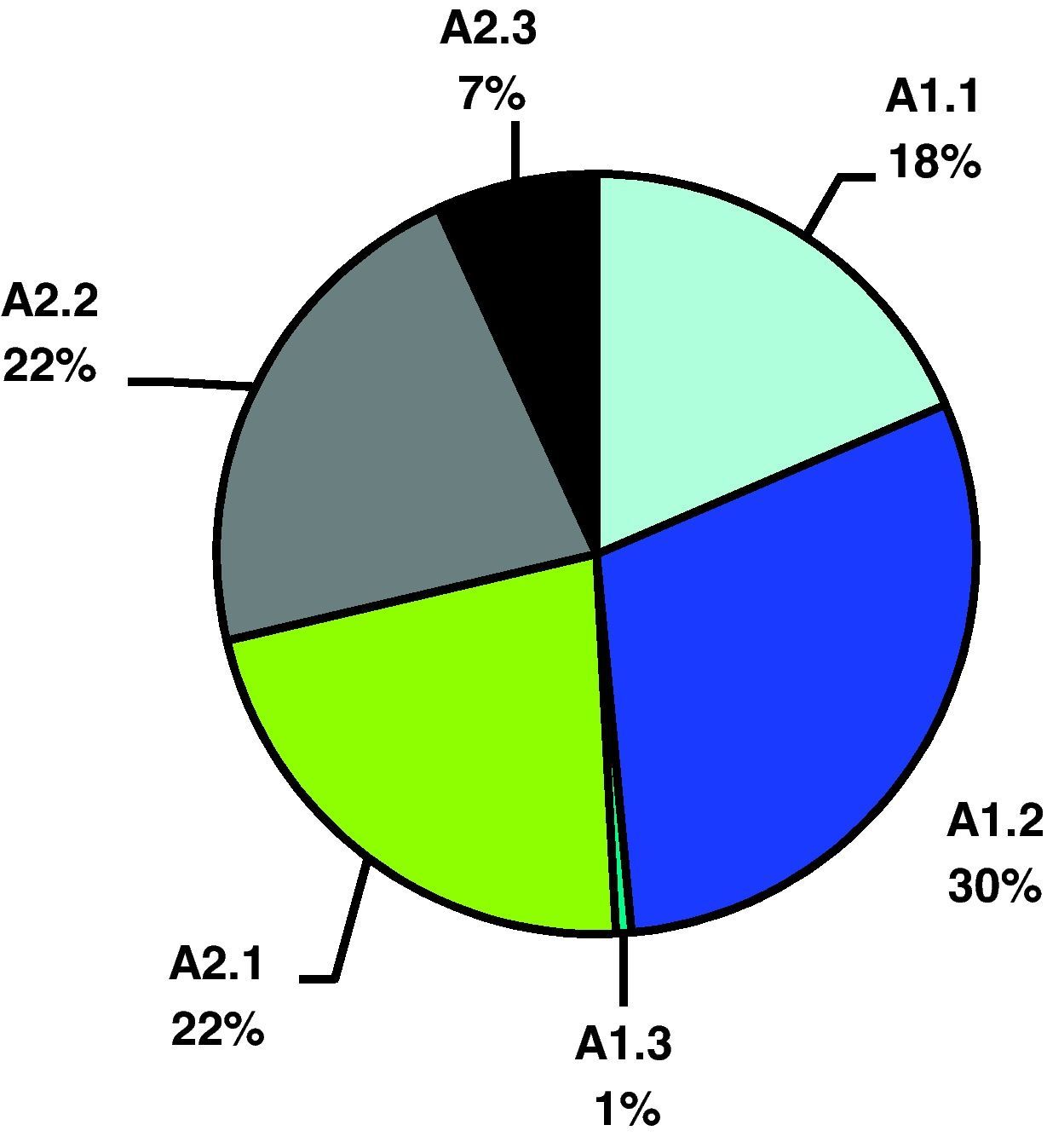
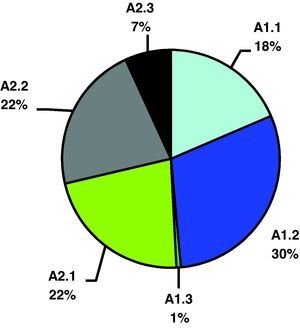
Using the AO classification for hip fractures, 19% of the fractures were A.1.1; 29% were A1.2; 1% was A1.3; 22% were A2.1; another 22% were A.2.2, and lastly 7% were A.2.3 (Fig. 3).
In close to 60% of cases, it was a displaced or non-displaced simple fracture; in 40%, it was a comminuted fracture, more or less displaced.
The patients were assessed for anaesthesia risk using the ASA classification, the results being distributed as follows: ASA 1=4%; ASA 2=52%; ASA 3=42%, and ASA 4=2%.
Spinal anaesthesia was used in 58% of cases, general anaesthesia in 24%, and 18% had spinal anaesthesia with an epidural catheter left in place for 24h.
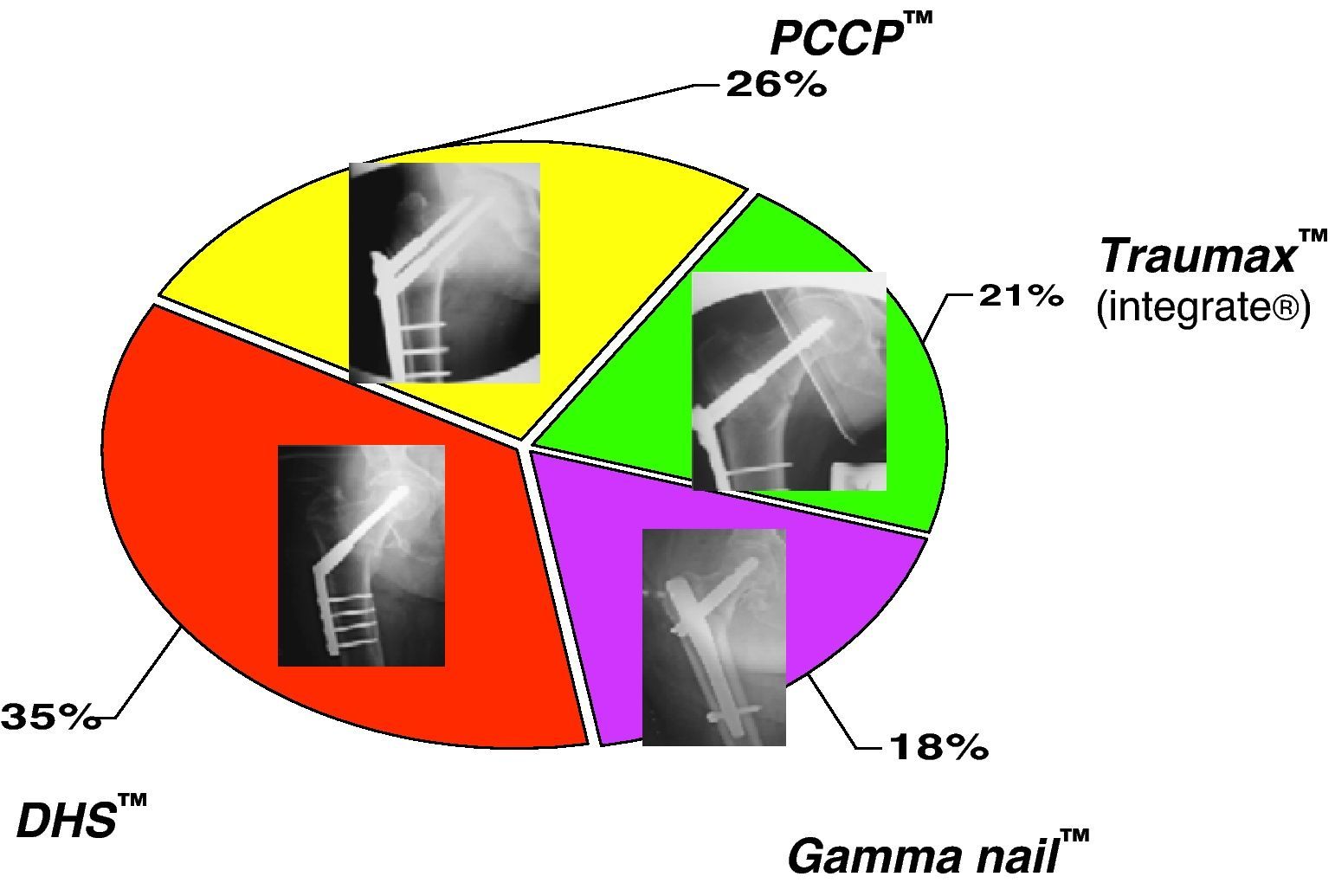
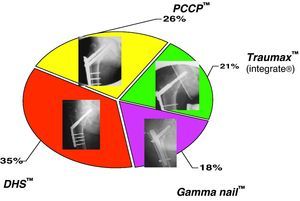
The following osteosynthesis methods were used (Fig. 4):
- -
Traumax® plate (21%)
- -
Gamma trochanteric nail® (18%)
- -
DHS® (35%)
- -
PCCP® (26%)
The univariate analysis found lower TGV losses in the women: 375±209ml (94–1.342), compared with 445±240ml (114–1.274) in the men.
Subjects who were not on antiaggregant and/or anticoagulant therapy had less bleeding (a mean of 360ml) than those who had previously been on this therapy (a mean of 460ml).
No significant differences were found in terms of ASA classification or type of anaesthesia (P>.05).
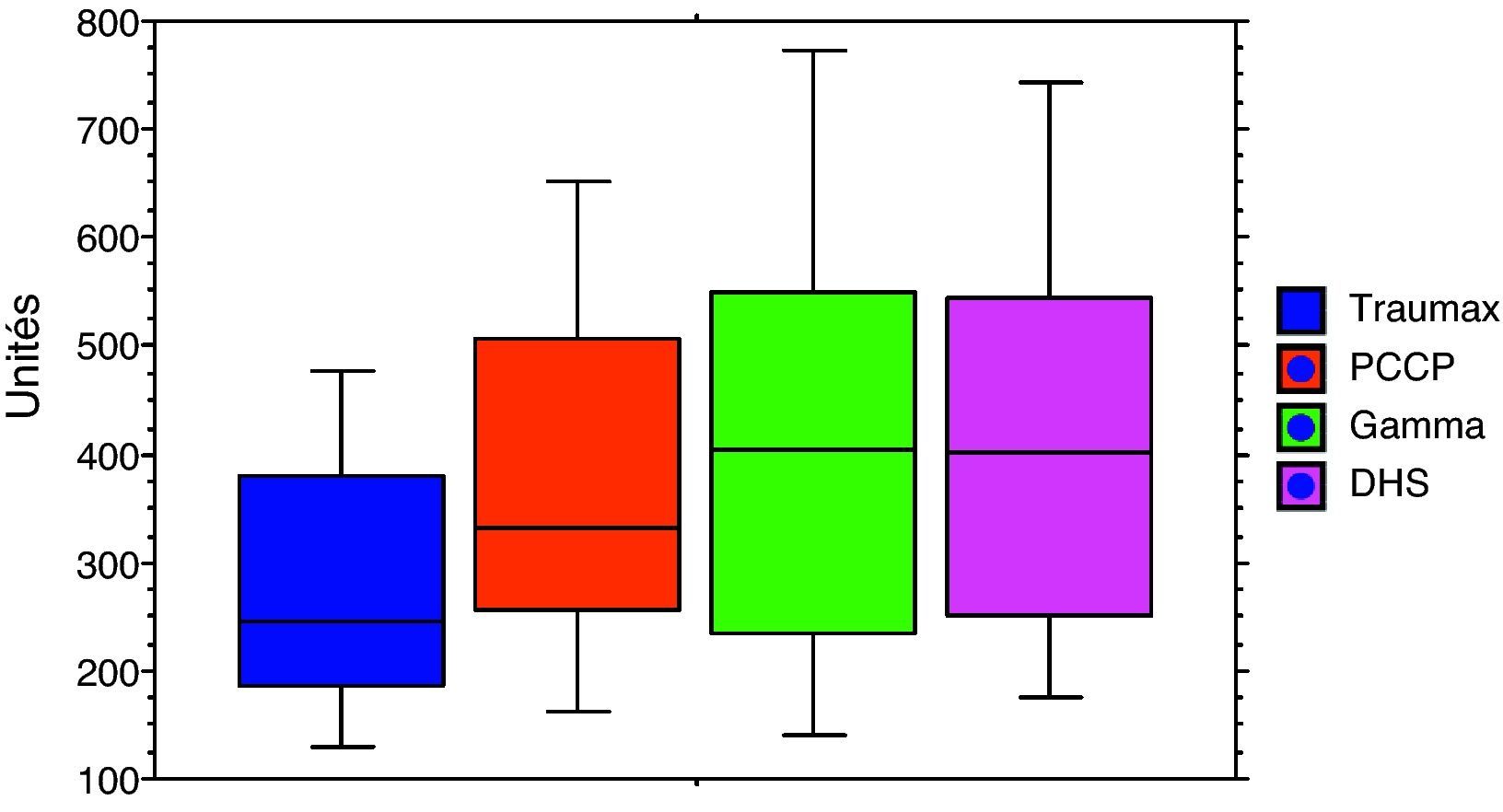
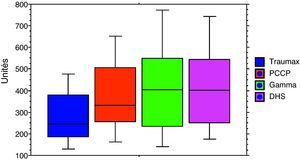
Evans I or II, A2.2 or A2.3, cervicotrochanteric, and simple pertrochanteric fractures bled less (330–360ml) than Evans IV or V, the other AO types, and complex pertrochanteric fractures (400–470ml) (Fig. 5).
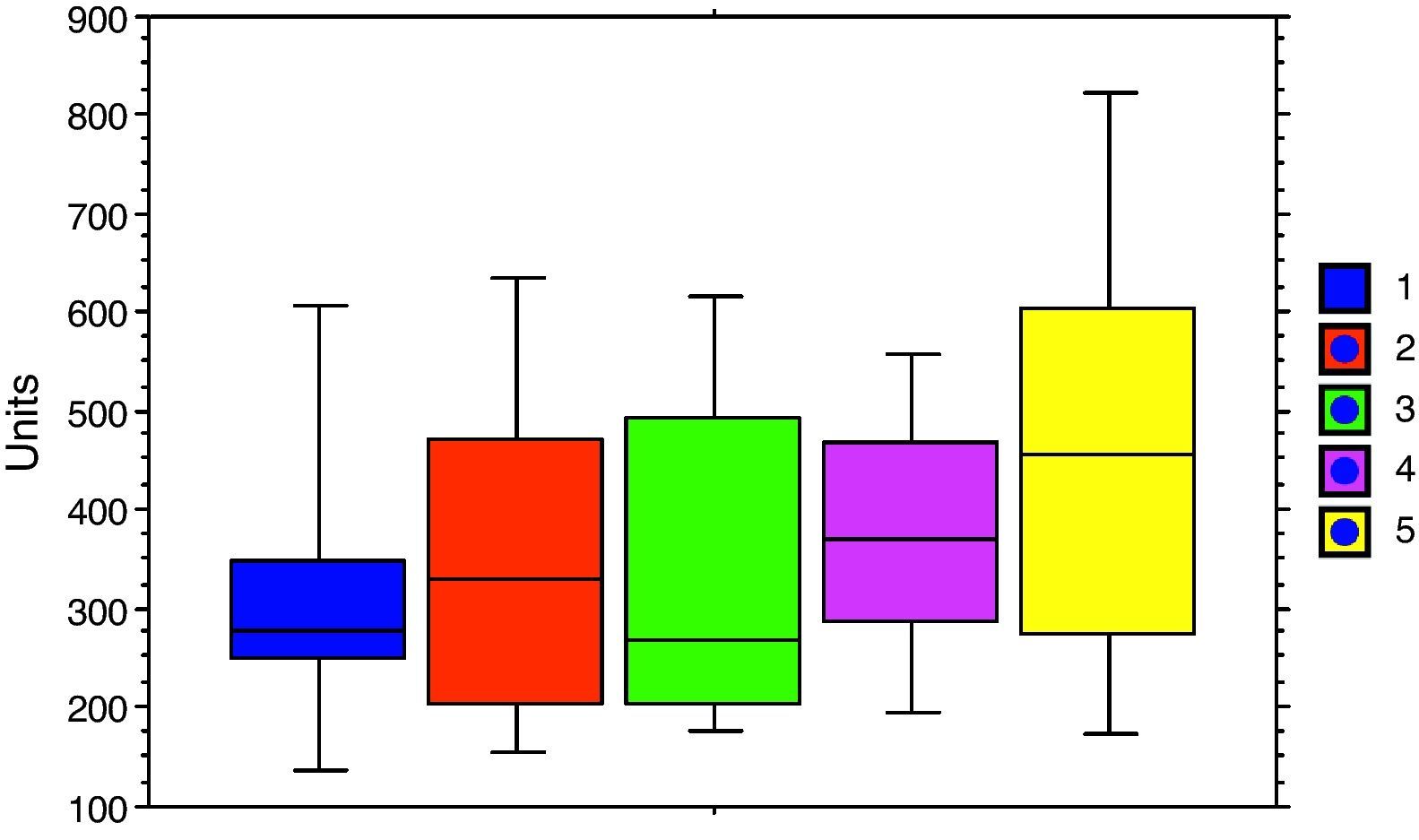
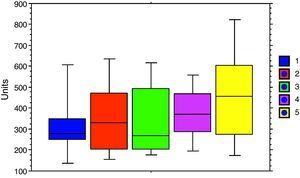
Patients in whom a Traumax® plate was used for the osteosynthesis had less bleeding (mean 270ml, range 180–380ml) than those in whom a Gamma nail® or a DHS plate® was used (mean 430ml, range 260–560ml) (Fig. 6).
The multivariate analysis found only 1 independent factor: fracture comminution (P<.05).
DiscussionAlthough the prognosis for trochanteric fracture has improved thanks to osteosynthesis techniques, quality of life for all these patients deteriorates upon diagnosis of this fracture, and close to 20% of these patients die during the first post-operative year.10–12
Anticoagulant and antiaggregant therapy increases intra-operative bleeding. This has been a known fact since Anekstein et al.13 reported it in their 2004 article published in the journal CORR, which supported the 1987 Modig et al. hypothesis.14 Although Anekstein et al.13 indicated that taking aspirin increased transfusion risk by 0.5units, according to them it was safe to operate on patients with a proximal femur fracture who were taking aspirin.
In our series, we found no statistically significant differences between the different types of anaesthesia. In 1987, Modig et al.14 reported that spinal anaesthesia reduced intra-operative bleeding.
The Wast et al. series2 included 475 pertrochanteric fractures in patients over 75years of age: 226 stable and 237 unstable fractures. They performed osteosynthesis with gamma nail in 237 patients, screw-plate in 230 patients, and nail-plate in 4 patients; 1 patient received a prosthesis, and 3 patients received orthopaedic treatment for the fracture. In one study, these authors concluded that the quality of the reduction and the positioning of the osteosynthesis are the factors that have the greatest impact on obtaining good post-operative results; in their opinion, the type of material implanted has little effect on the results obtained.
There were 307 patients in our series: 64 were treated with a Traumax® plate, 55 with a gamma® nail, 108 with a DHS®, and 80 with a PCCP® plate.
The patients treated with a screw-plate osteosynthesis were those who least required transfusion and had less blood loss.
In 2001, Dujardin15 compared bleeding in patients with DHS plate and bleeding in patients with a small-diameter nail implanted using a minimally invasive technique and found a decrease in bleeding with this technique.
In our series, the mean blood loss with a Traumax® plate was 270ml. Bensafi et al.16 reported a mean blood loss of 360ml in patients treated with a PCCP® plate, indicating that, compared to intramedullary nailing, using the plate reduced intra-operative bleeding and damage to muscles and tendons.
Some authors have stated that, with modern intramedullary osteosynthesis systems, there is less intra- and post-operative bleeding, patients require fewer transfusions, and surgery time is shorter than with classic extramedullary systems.5,17–19
Contradicting the above statements, other authors20 report a 35–60% incidence of transfusions with the gamma nail due to intra-operative and post-operative bleeding from damaged gluteal musculature, from the fracture site, and from the bone's medullary canal—especially if a power reamer was used.
Sadowski et al.21 compared bleeding in fractures treated with DHS® or with endomedullary nail and found that there were fewer transfusions in the latter group; however, their study included only AO classification types 31-A3 fractures.
In contrast to Sadowski,21 Aune et al.22 found less bleeding and fewer transfusions in the patients treated with DHS® compared to those treated with endomedullary nail.
In our study, we found that patients treated with DHS® were transfused more than those treated using PCCP® and Traumax® plate. This agrees with published results in the literature (Brandt et al.23 and Adans et al.17).
Peyser et al.24 do not mention post-operative transfusions in their study comparing patients with a PCCP® plate to patients with a DHS® plate, but they do indicate a decrease in intra-operative bleeding (PCCP®=161ml vs. DHS®=374ml).
Adans et al.17 found an increased risk of complications in patients with gamma nail compared with patients with DHS plate, but it was not a statistically significant difference.
Salido et al.25 identified a statistically significant correlation between the need for transfusion and the haemoglobin value reported on the pre-operative CBC in patients who underwent a total hip replacement.
This study has a large number of patients and evaluates different methods of osteosynthesis. The difficulty arises with studying the interaction between different variables and seeing whether there is a connection between these variables and peri-operative bleeding.
Within this study, the only independent risk factor found to be causing increased blood loss and requiring peri-operative blood transfusion was fracture comminution.
ConclusionFracture comminution constitutes the only independent risk factor where significant TGV is lost and peri-operative blood transfusion is required. There are numerous other factors, but these are related to each other.
Transfusion needs must be foreseen and optimised because of the risks associated with administering transfusions.
It is important that the type of fracture be accurately evaluated, especially in elderly and fragile patients, so that the need for transfusion may be anticipated. In this way, transfusions that are needless, costly, and sometimes dangerous (risk of haemodynamic overload) could be prevented.
Level of evidenceEvidence level III.
Conflicts of interestThe authors have no conflicts of interest to declare.
Ethical DisclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors will declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors must have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Please cite this article as: Torres A, et al. Análisis estadístico de los factores que aumentan el sangrado perioperatorio en las fracturas trocantereas. Rev esp cir ortop traumatol. 2012;56(1):11-16.