To evaluate the results of total hip arthroplasty in patients with osteoarthritis and to identify predictors of poor functional outcome.
Materials and methodsA prospective observational study in patients operated on in 2006 with total hip arthroplasty in 4 hospitals in Guipúzcoa, followed up for 1 year. Outcome variables: pain, physical function, complications, mortality, quality of life by WOMAC and SF-12 (at 0, 3, 6 and 12 months) and “Poor functional outcome” at one year (last quartile of the WOMAC in function area). Logistic regression was performed to examine predictors of poor functional outcome.
ResultsA total of 166 patients were followed up. The incidence of systemic and local complications was 6.3% and 14.5%, respectively, 4.3% readmissions and no deaths related to surgery. Close to 40 points improvement in pain, stiffness and WOMAC functional limitation was mainly in the first 3 months after surgery. A similar trend was seen, but lower in the physical and mental component of the SF12 (12 and 8 points, respectively). The previous score on the WOMAC function area and the physical component of SF-12, and the existence of any complications, are predictors of poor functional recovery.
DiscussionThe improvement experienced after the surgery is already very important before the third month. The functional status and physical status before surgery and possible complications of surgery are significant determinants of the results.
Evaluar los resultados del primer año en la artroplastia total de cadera de pacientes con osteoartritis e identificar los factores predictores de mala evolución funcional.
Material y métodoEstudio observacional, prospectivo en pacientes intervenidos en 2006 con artroplastia total de cadera en 4 hospitales de Guipúzcoa, seguidos durante un año. Variables de resultado: dolor, función física, complicaciones, mortalidad, calidad de vida mediante WOMAC y SF-12 (a 0, 3, 6 y 12 meses) y «mal resultado funcional» al año (último cuartil del WOMAC en área de función). Mediante regresión logística se estudiaron los factores predictores de mal resultado funcional.
ResultadosSe incluyeron 166 pacientes. La incidencia de complicaciones sistémicas y locales fue de 6,3 y 14,5%, respectivamente, con 4,3% de reingresos y sin fallecimientos relacionados con la cirugía. Mejoría cercana a 40 puntos en dolor, rigidez y limitación funcional del WOMAC, principalmente en los primeros tres meses postintervención. Evolución similar, pero inferior en el componente físico y mental del SF12 (12 y 8 puntos respectivamente). La puntuación previa en el área de función de WOMAC y en el componente físico del SF-12, así como la existencia de alguna complicación, son factores predictores de la mala recuperación funcional.
DiscusiónLa mejoría experimentada tras la intervención es ya muy relevante antes del tercer mes. La situación funcional y física previa a la intervención y las posibles complicaciones de la cirugía son factores determinantes de los resultados.
Hip and knee replacements are reportedly on the rise in various countries, owing to the aging of the population, on the one hand, with its attendant upsurge in degenerative diseases and, on the other hand, to widening of the spectrum of individuals in whom primary arthroplasty is indicated. In 1996 in the United Kingdom, it was estimated that hip replacements would increase by 40% over a 30-year period, based on demographic trends in the population and without taking into account possible changes in the indication criteria.1 In Spain, analysis of the evolution of arthroplasty rates in Cataluña revealed a 17% mean annual increase in knee replacements between 1994 and 2005 and a 9% increase in hip replacements between 1994 and 2000.2 In the Basque Country, there was a 37% increase in the number of total hip replacements (THR) between 1998 and 2008.3
Hip and knee replacements have proven to be effective as an intervention for pain relief and improved functioning in patients with OA (osteoarthritis) in these joints.4–6 They are also consistently reported to have a positive impact on health-related quality of life (HRQoL)—a term that includes not only pain but other aspects such as functional capacity (domestic chores, return to work), social integration, psychological well-being, bodily sensation, and satisfaction with life.7 Results vary, depending on a number of factors not necessarily intervention-related,8–15 and are good, generally speaking: about 90% of hip replacements end up pain-free and with no complications 10–15 years after the surgery,16 which is more cost-effective than other types of surgery.17 This type of surgery is not without risk, however: a 3-month mortality rate of 0.4–0.7% has been reported for hip replacement, as well as an incidence of about 4% for serious complications.18
The steadily increasing use of this intervention in conjunction with the expanding of patient profiles requires an evaluation of its risks and benefits as well as the factors associated with a poor prognosis. The objective of this study was to report the mortality, the incidence of complications, and the gains in HRQoL during the first year in patients with OA who have undergone THR and to analyse the predictive factors for a poor outcome.
Materials and methodsThis was a prospective observational study that included patients with OA of the hip who underwent primary total replacement of this joint in the year 2006 at public hospitals (1 tertiary and 3 regional) in Guipúzcoa.
The patients were identified from the surgical wait list (SWL); their consent to participate was obtained, and a pre-intervention questionnaire was completed for each one. To determine the representativeness of the patients included, their baseline characteristics were compared with those of the patients who chose not to participate and/or did not fill out the pre-intervention questionnaire.
Information was collected on the baseline pre-intervention circumstances, the characteristics of the intervention, any complications, and the results during the first year.
Pre-intervention variablesPre-intervention variables included
- •
sociodemographic (sex, age, body mass index (BMI));
- •
comorbidity (number of associated conditions);
- •
surgical risk per the ASA classification (low: I, II, and III/high: IV);
- •
involvement of another joint (contralateral hip, knee, spine, shoulder, elbow, wrist);
- •
time on the wait list (months);
- •
pain (walking and at rest);
- •
functioning (maximum ambulation, mobility on stairs, presence of a limp, and the need for assistive devices to walk or travel); and
- •
quality of life using the SF-12 and WOMAC (Western Ontario and McMaster Universities Index of Osteoarthritis), both translated to Spanish and validated.19,20
The SF-12 questionnaire measures generic health concepts and includes 12 items on pain, physical problems and their limitations, emotional problems, and mental health; physical and mental summary scores may be calculated ranging from 0 to 100, where 0 is the worst possible score and 100 is the best possible score. The WOMAC is a quality-of-life questionnaire that is specific for patients with OA of the hip or knee and consists of 24 items grouped into 3 scales—pain, stiffness, and functional capacity—with a range of 0 to 100, where 0 is the best health status and 100 is the worst health status. Characteristics of the intervention were type of anaesthesia, duration of the procedure, type of prosthesis fixation, length of hospital stay, and blood transfusion (pre-operative, intra-operative, or post-operative).
ComplicationsIntra-operative and post-operative complications through the first post-intervention year included local complications (infection, wound problems, dislocation, peri-prosthetic fracture, neurological injury, and prolonged bleeding), systemic complications (thrombophlebitis, deep vein thrombosis, pulmonary thromboembolism, pneumonia, cardiovascular complications, genitourinary complications, and others such as fever or drug reaction) and death.
Clinical and quality-of-life resultsPain (walking and at rest) and functioning (maximum ambulation, mobility on stairs, presence of a limp, and the need for assistive devices to walk or travel) were assessed by the surgeon prior to the intervention and 1 year later. The results for quality of life (SF-12, WOMAC) and patient satisfaction with his/her recovery were determined using a self-completed questionnaire (patients were considered to be feeling satisfied with the intervention if they reported that their symptoms of pain, stiffness, and functional limitation were “much better” than before the surgery and if they also remained stable until the end of the follow-up period). As a summary of results variable, “poor functional outcome” (PFO) was defined as a patient who, at 12 months, was in the last quartile in the functioning area on the WOMAC.
Data sourceData were obtained from the medical record and from the SF-12 and WOMAC questionnaires completed by the patient. Prior to and 1 year after the intervention, the traumatologist asked the patient about pain and functioning using a closed questionnaire that addressed the above-mentioned variables. The SF-12 and WOMAC questionnaires were either mailed to the patients or given to them in the clinic prior to the intervention (at the time the informed consent was obtained) and at 3, 6, and 12 months afterwards.
Analysis of the dataPatient characteristics and the main results measurements were described in terms of either mean and standard deviation or ratios. Differences in pain and functioning between the time prior to intervention and 1 year later were analysed using the McNemar's test for paired data. Changes in the HRQoL scales were analysed using repeated measures linear models. Kaplan–Meier (interval-censored) plots were used to represent the time elapsed to recovery. We looked for predictive variables for PFO by evaluating their association with baseline variables and complications, first through univariate analysis and then through multivariate logistic regression analysis; variables that turned out to be significant (P<.05) on the univariate analysis were included as predictive variables. The multivariate model is believed to have good predictive capability if the area under the ROC curve is >0.7. The SPSS v. 16 and R.9.1 programs were used to analyse the data.
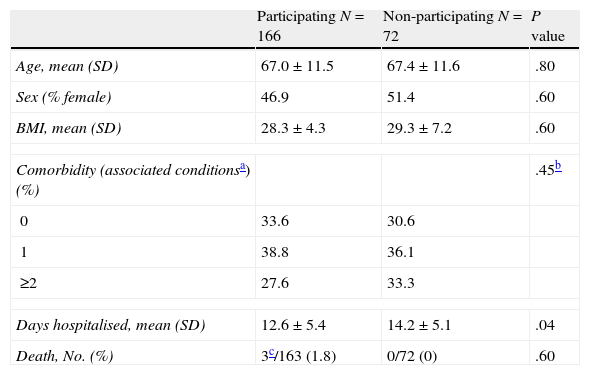
ResultsA total of 166 patients were operated on by 38 different surgeons. The following surgical approaches were used: 97 (58.4%) anterolateral, 29 (17.5%) transgluteal, 3 (1.8%) transtrochanteric, 17 (10.2%) posterolateral, and 20 (12%) approach unknown. Table 1 shows a comparison between the 166 participating and the 72 non-participating patients in terms of some baseline characteristics. No statistically significant differences were observed except in the case of the mean length of stay, which was 2 days longer for those who did not participate. No surgery-related deaths occurred, but there were 3 deaths from other causes in the participating patient group. Among those participating, 46.9% were female, and the mean age was 67±11.6 years with 30% over the age of 75. One or more associated conditions were present in 60.8%.
Baseline characteristics of participating and non-participating patients.
| Participating N=166 | Non-participating N=72 | P value | |
| Age, mean (SD) | 67.0±11.5 | 67.4±11.6 | .80 |
| Sex (% female) | 46.9 | 51.4 | .60 |
| BMI, mean (SD) | 28.3±4.3 | 29.3±7.2 | .60 |
| Comorbidity (associated conditionsa) (%) | .45b | ||
| 0 | 33.6 | 30.6 | |
| 1 | 38.8 | 36.1 | |
| ≥2 | 27.6 | 33.3 | |
| Days hospitalised, mean (SD) | 12.6±5.4 | 14.2±5.1 | .04 |
| Death, No. (%) | 3c/163 (1.8) | 0/72 (0) | .60 |
SD: standard deviation; BMI: body mass index.
Some joint condition in the back, knee, upper extremities, and/or contralateral hip, which could have interfered with the results of the intervention, was seen in 32.9% of patients. From the day they were put on the waiting list until they underwent surgery, 29.5% of patients waited more than 6 months; 42.4% waited 3–6 months; and only 28.1% waited less than 3 months. Surgical risk was low in 97.5%.
The mean duration of surgery was 115±27.2min, and 53.9% of patients required peri-operative transfusion. In 2 cases, the prosthesis was cemented, and in the rest (98.7%) the prosthesis was not cemented. General anaesthesia alone was used in 8.7%.
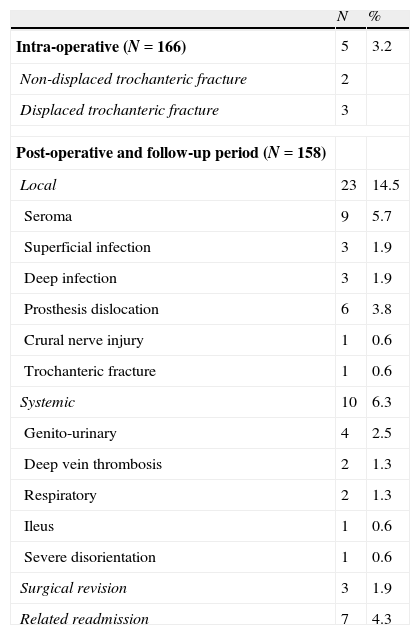
There were intra-operative complications in 3.2% of cases. During the admission and the first follow-up year, 14.5% had local complications and 6.3% had systemic complications (Table 2).
Complications.
| N | % | |
| Intra-operative (N=166) | 5 | 3.2 |
| Non-displaced trochanteric fracture | 2 | |
| Displaced trochanteric fracture | 3 | |
| Post-operative and follow-up period (N=158) | ||
| Local | 23 | 14.5 |
| Seroma | 9 | 5.7 |
| Superficial infection | 3 | 1.9 |
| Deep infection | 3 | 1.9 |
| Prosthesis dislocation | 6 | 3.8 |
| Crural nerve injury | 1 | 0.6 |
| Trochanteric fracture | 1 | 0.6 |
| Systemic | 10 | 6.3 |
| Genito-urinary | 4 | 2.5 |
| Deep vein thrombosis | 2 | 1.3 |
| Respiratory | 2 | 1.3 |
| Ileus | 1 | 0.6 |
| Severe disorientation | 1 | 0.6 |
| Surgical revision | 3 | 1.9 |
| Related readmission | 7 | 4.3 |
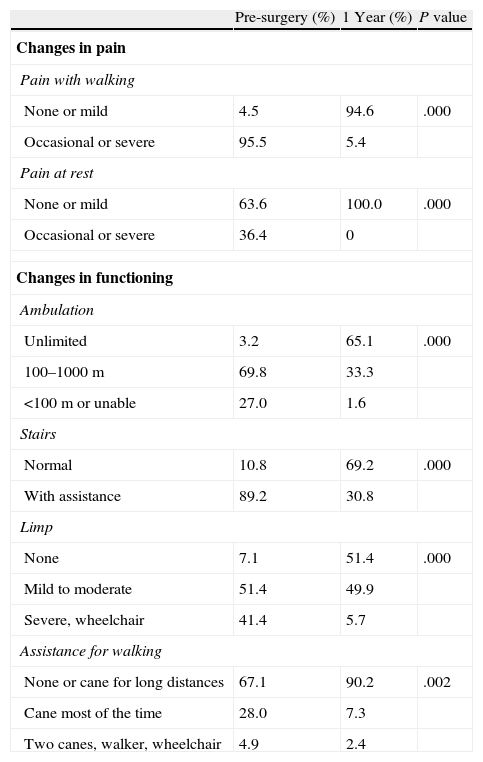
Changes in pain and functioning, as assessed by the clinician, were quite remarkable (Table 3). Pain with walking disappeared in 90% of patients; pain at rest disappeared in all those who had had it. Virtually all patients had gait limitations pre-operatively, but at 1 year, 65% had achieved a gait perimeter almost normal for their age. More than 1/3 of patients had walked with a severe limp or had been confined to a wheelchair, but after the surgery, this proportion dropped to 6%; in 50% of patients, however, a perception of limp during ambulation remained.
Changes in pain and functioning as assessed by the traumatologists.
| Pre-surgery (%) | 1 Year (%) | P value | |
| Changes in pain | |||
| Pain with walking | |||
| None or mild | 4.5 | 94.6 | .000 |
| Occasional or severe | 95.5 | 5.4 | |
| Pain at rest | |||
| None or mild | 63.6 | 100.0 | .000 |
| Occasional or severe | 36.4 | 0 | |
| Changes in functioning | |||
| Ambulation | |||
| Unlimited | 3.2 | 65.1 | .000 |
| 100–1000m | 69.8 | 33.3 | |
| <100m or unable | 27.0 | 1.6 | |
| Stairs | |||
| Normal | 10.8 | 69.2 | .000 |
| With assistance | 89.2 | 30.8 | |
| Limp | |||
| None | 7.1 | 51.4 | .000 |
| Mild to moderate | 51.4 | 49.9 | |
| Severe, wheelchair | 41.4 | 5.7 | |
| Assistance for walking | |||
| None or cane for long distances | 67.1 | 90.2 | .002 |
| Cane most of the time | 28.0 | 7.3 | |
| Two canes, walker, wheelchair | 4.9 | 2.4 | |
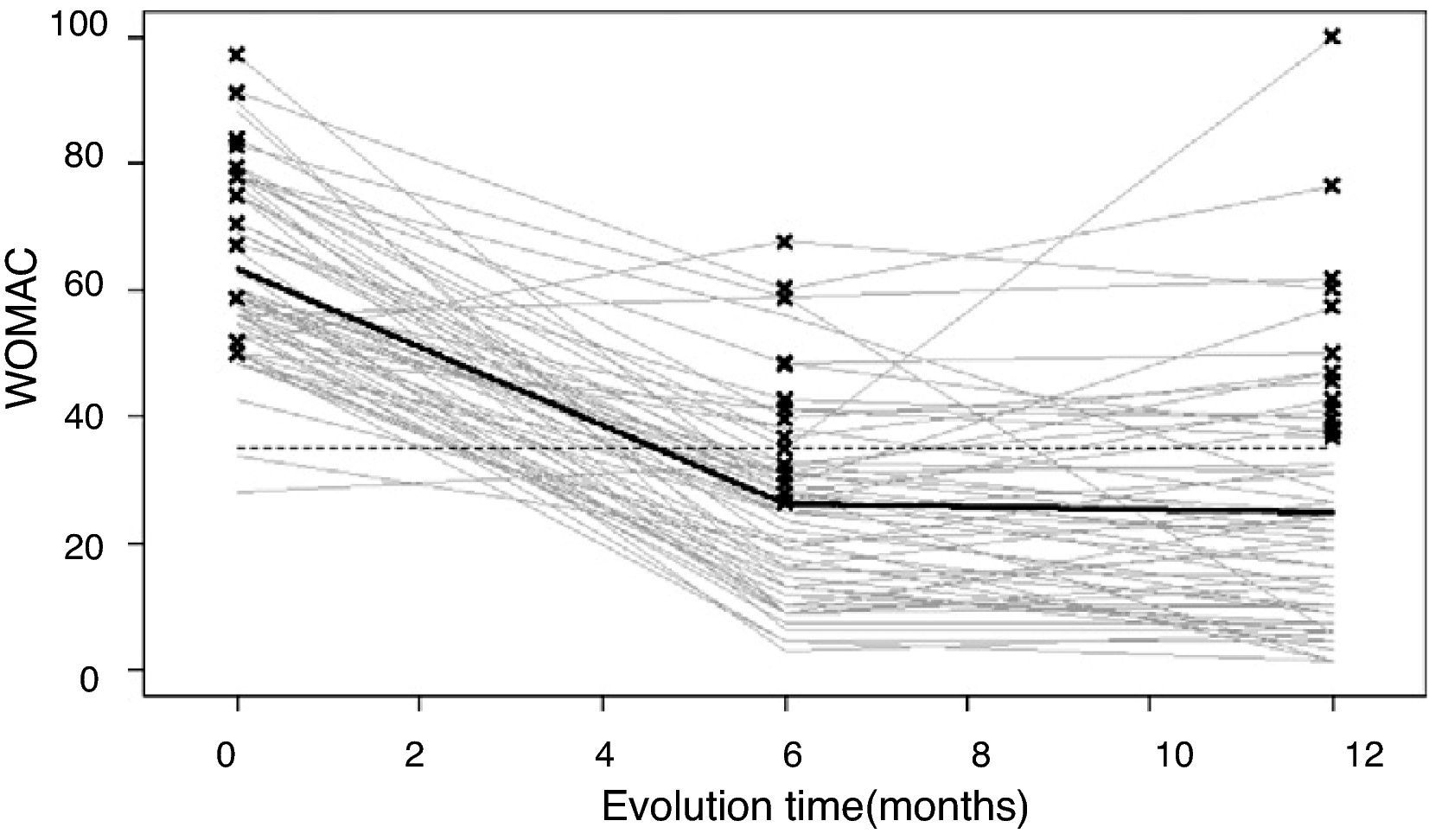
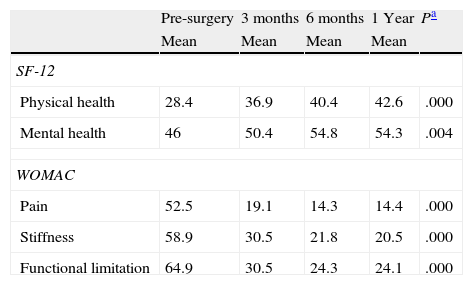
The rate of response to the HRQoL questionnaires during the follow-up period was 71%—that is, 29% of the patients did not respond to any of the questionnaires sent out during the first follow-up year. Table 4 shows the outcome in terms of general health from the SF-12 and in terms of pain, stiffness, and functional limitation from the WOMAC questionnaire. There was about a 40-point improvement in the 3 WOMAC dimensions, mainly in the first 3 post-intervention months, although significant improvement was seen up to 6 months (the changes in functional limitation are shown in Fig. 1). Similar changes were observed in the physical and mental components of the SF-12, although these were of lesser magnitude (a 12- and 8-point improvement, respectively).
Change in quality of life from before surgery to 3, 6, and 12 months.
| Pre-surgery | 3 months | 6 months | 1 Year | Pa | |
| Mean | Mean | Mean | Mean | ||
| SF-12 | |||||
| Physical health | 28.4 | 36.9 | 40.4 | 42.6 | .000 |
| Mental health | 46 | 50.4 | 54.8 | 54.3 | .004 |
| WOMAC | |||||
| Pain | 52.5 | 19.1 | 14.3 | 14.4 | .000 |
| Stiffness | 58.9 | 30.5 | 21.8 | 20.5 | .000 |
| Functional limitation | 64.9 | 30.5 | 24.3 | 24.1 | .000 |
Data shown in bold cells mean that there was a statistically significant difference between the determinations.
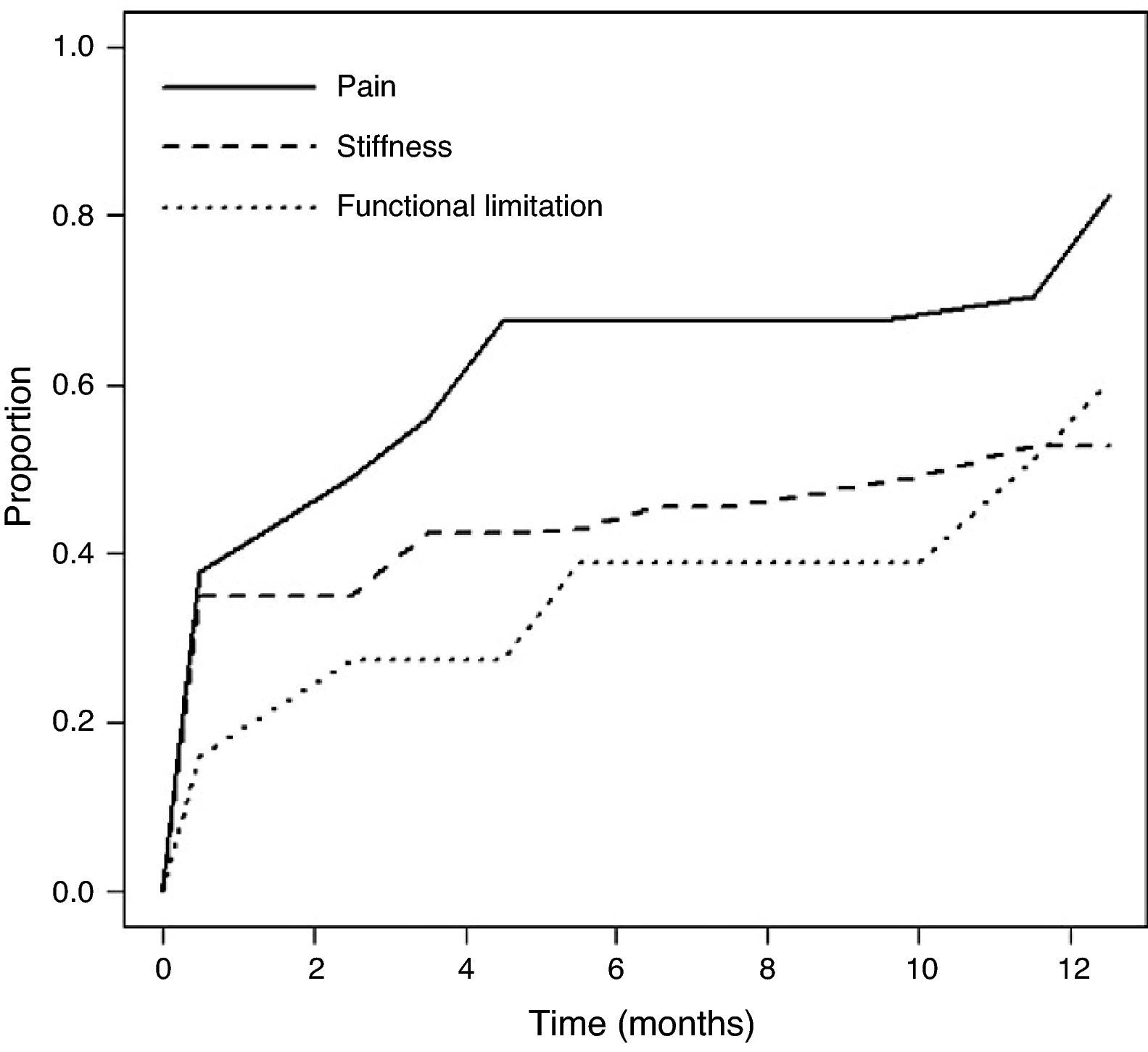
Fig. 2 shows the time elapsed post-operatively until the patient reported feeling “much better” than before the intervention in terms of pain and stiffness symptoms and functional capacity. With regard to pain, 2.5 months was the point at which 50% of the patients were reporting marked improvement; by the end of the follow-up period, this proportion had risen to 83%. Recuperation in terms of stiffness and functional capacity came later: 50% achieved this at 10 and 11 months, respectively, and by the end of the follow-up period, the proportion of patients reporting great improvement in stiffness and functional limitation was 53% and 60%, respectively.
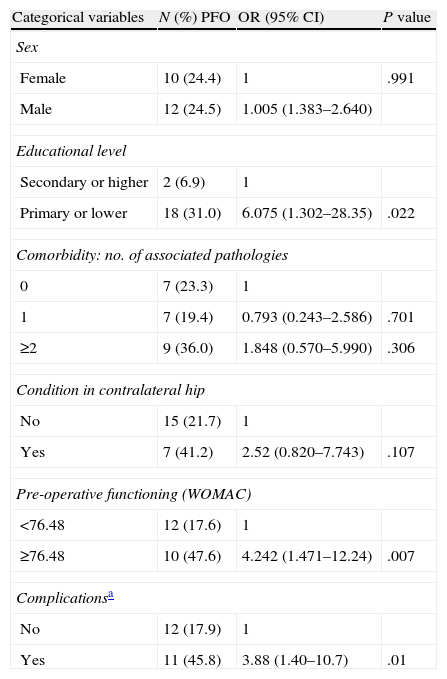
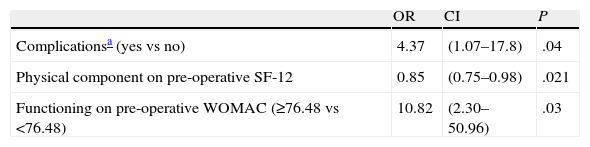
In the univariate analysis, no significant association was found between PFO and sex, age, number of associated conditions (0, 1, and ≥2), involvement of other joints (yes vs no), pre-operative pain (as continuous variable), and the SF-12 mental component (continuous). A significant association was found, however, with the functioning dimension on the pre-intervention WOMAC (≥76.48 vs <76.48); the physical component on the pre-intervention SF-12 (continuous); the existence of a complication intra-operatively or at any time during the follow-up period (yes vs no); and educational level (none/primary vs secondary/university) (Table 5). When a multivariate logistic regression model was fitted (Table 6), the association between PFO and educational level lost its significance. Of the 3 variables that retained their association with PFO, poor pre-intervention functional status had an OR of 10.8 (95% CI: 2.3–50.9); the SF-12 physical component had an OR of 0.85 (95% CI: 0.75–0.98); and the existence of any complication had an OR of 4.37 (95% CI: 1.1–17.8). The resulting model had good predictive capability, with an area under the ROC curve of 0.85 (95% CI: 0.75–0.95).
Predictive variables for PFO (univariate analysis).
| Categorical variables | N (%) PFO | OR (95% CI) | P value |
| Sex | |||
| Female | 10 (24.4) | 1 | .991 |
| Male | 12 (24.5) | 1.005 (1.383–2.640) | |
| Educational level | |||
| Secondary or higher | 2 (6.9) | 1 | |
| Primary or lower | 18 (31.0) | 6.075 (1.302–28.35) | .022 |
| Comorbidity: no. of associated pathologies | |||
| 0 | 7 (23.3) | 1 | |
| 1 | 7 (19.4) | 0.793 (0.243–2.586) | .701 |
| ≥2 | 9 (36.0) | 1.848 (0.570–5.990) | .306 |
| Condition in contralateral hip | |||
| No | 15 (21.7) | 1 | |
| Yes | 7 (41.2) | 2.52 (0.820–7.743) | .107 |
| Pre-operative functioning (WOMAC) | |||
| <76.48 | 12 (17.6) | 1 | |
| ≥76.48 | 10 (47.6) | 4.242 (1.471–12.24) | .007 |
| Complicationsa | |||
| No | 12 (17.9) | 1 | |
| Yes | 11 (45.8) | 3.88 (1.40–10.7) | .01 |
| Continuous variables | OR (95% CI) | P value |
| Body Mass Index | 0.992 (0.891–1.105) | .888 |
| Pre-operative pain (WOMAC) | 1.020 (0.987–1.055) | .232 |
| Age (years) | 1.015 (0.973–1.059) | .493 |
| Physical component on pre-operative SF-12 | 0.870 (0.783–0.968) | .010 |
| Mental component on pre-operative SF-12 | 0.985 (0.951–1.020) | .407 |
PFO: poor functional outcome (last quartile in the functioning area on the WOMAC at end of follow-up). Variables with statistical significance are shaded.
Predictive variables for PFO (logistic regression analysis).
| OR | CI | P | |
| Complicationsa (yes vs no) | 4.37 | (1.07–17.8) | .04 |
| Physical component on pre-operative SF-12 | 0.85 | (0.75–0.98) | .021 |
| Functioning on pre-operative WOMAC (≥76.48 vs <76.48) | 10.82 | (2.30–50.96) | .03 |
PFO: poor functional outcome (last quartile in the functioning area on the WOMAC at end of follow-up). Area under the ROC curve=0.85 (95% CI: 0.75–0.95).
This study analysed the results obtained 1 year after primary hip replacement in patients with OA; substantial, statistically significant improvements were observed. The score achieved on the physical component of the SF-12 was slightly lower than that observed in the general population, indicating that, while the improvement was significant, it did not reach the same level seen in the general population. However, the mean score achieved on the mental component was 4–5 points higher than that seen in the general population.21 This could be related to the fact that, as some data suggest, individuals who undergo arthroplasty are in better general health, have significantly fewer comorbidities, and have a lower mortality rate than individuals of the same sex and comparable age in the general population.22,23
Our results are corroborated by those previously reported in other studies.4–6 A review of 20 articles published between 1978 and 1995 evaluating changes in HRQoL following THR found that every article reported improvement and gain in quality of life, which occurs within the first 3 months, although some physical measurements take longer.24 These articles are also consistent with other more recent studies on the magnitude of the gain realized: differences of close to 40 points on pain, stiffness, and functional limitation scales4,25 and about 12 points on the physical component of the SF-36 and less than 10 on mental health.25 The physical health levels achieved at 6 months also remain below those seen in the general population; this is not the case for mental health, however, where levels similar to those of the general population are reported. Hamel et al. reported changes of a lesser magnitude, but their study population was made up of individuals 65 years of age or older; they observed no changes in mental health.26
The incidence of complications was within the range reported in other studies. Since the introduction of antithrombotic measures, the incidence of deep vein thrombosis (DVT) has dropped significantly, being reported recently between 1% and 3.6%.27–29 In a specific study on the diagnosis of DVT in hip and knee replacement, after a 3-month follow-up period, the incidence of DVT was 4.9% and 0.6% for pulmonary embolism.30 The incidences found for other complications were 1.7% for urinary infection, 2–4% for dislocations,27–29,31 and 0.2–3.5% for deep wound infections.28,31
The predictive factors found in our study had been previously reported,4,9 except for the complications. However, some of those reported in other studies could not be confirmed as predictive factors for poor outcome; this was the case with age,4,9 sex,9,12 BMI,4,14 and comorbidity,9,14,15 although in some of these studies, they lost predictive power when a multivariate model was fitted.4 The Barrera-Cadenas et al. study15 also found no association between post-surgical evolution and age or sex but did find an association between higher pre-operative comorbidity and better social functioning after the surgery; this association could not be confirmed in our study.
One limitation of our study could lie in a selection bias for the patients enrolled; we believe, however, that our results could be extrapolated to all primary THRs performed in the Guipúzcoa public hospital network because there were no statistically significant differences found with the patients not enrolled in the study in terms of baseline characteristics, such as sex, age, BMI, and comorbidity. However, interventions performed at private medical centres—which, in 2008, were 37.6% of the total number of THRs performed in Guipúzcoa3—would remain outside our study population. The follow-up period reduced to 1 year could also be a limitation, although a similar study—but with a 5-year follow-up period—concluded that the improvement realized in the first post-operative months remained stable during the subsequent follow-up years.32
It may be concluded from our study that, after a hip replacement, the pain disappears or becomes mild in 95% of patients; 2/3 of them achieve good functioning; and the risk of complications is low. Marked changes in quality of life are seen in relation to pain and functional capacity, and these are achieved mainly within 3 months after the intervention; changes seen in other areas, such as mental health, are of lesser magnitude. In terms of predicting long-term success with this intervention, important aspects are the patient's initial circumstances—in particular, his/her functioning and physical condition—and the lack of complications during the procedure and in the first 12 months thereafter.
FinancingThis study was funded by a grant from the Departamento de Sanidad del Gobierno Vasco [Vasco Government Department of Health].
Evidence levelEvidence level IV.
Conflicts of interestThe authors have no conflicts of interest to declare.
Ethical DisclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors will declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors must have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence must be in possession of this document.
The authors wish to thank Olga Gabaldón, Olatz Mokoroa y Maitane, and Maialen Salas for their assistance with the field work, and Pablo Martínez Camblor for editing the figures.
Please cite this article as: Sarasqueta C, et al. Artroplastia primaria de cadera: resultados en el primer año y factores predictores de mala evolución. Rev Esp Cir Ortop Traumatol. 2012;56(1):3-10.