This study compares the efficacy in post-operative pain control of the intraarticular catheter compared to the epidural catheter after primary total knee arthroplasty.
Material and methodRandomised clinical trial consisting of two groups of patients. A control group with intradural anaesthesia and an intraoperative epidural catheter (ropivacaine) and an intervention group using the same anaesthetic technique and an intraarticular catheter with an elastomeric pump (ropivacaine+dexketoprofen). Data such as demographic, anaesthetic and surgical variables, pain intensity according to Verbal Rating Scale, opioid use and complications, joint balance, onset of walking and hospital stay were recorded.
ResultsA lower incidence and severity on Verbal Rating Scale and a better control of postoperative pain (p<.0014) were observed in the intervention group. Joint balance also presented significant results in flexion and 74% of these patients started walking before the first 36h and the control group had not yet done so. Regarding patient satisfaction, 54.1% of the patients were “very satisfied” with the use of the catheter (p>.001). Finally, the hospital stay decreased significantly, with 33.3% of intervention group patients discharged within the first 48h compared to none of the control group.
Discussion and conclusionsThe use of the intraarticular catheter as postoperative analgesia is a useful and safe alternative. It reduces the possibility of side effects. It helps in early improvement of joint balance, onset of walking and control of pain. All of which increase patient satisfaction and result in a shorter period of hospitalisation.
Comparar la eficacia en el control del dolor postoperatorio de pacientes sometidos a artroplastia total de rodilla primaria comparando catéter intraarticular versus epidural.
Material y métodoEnsayo clínico aleatorizado formado por dos grupos de pacientes: un grupo control con anestesia intradural y un catéter epidural (ropivacaína) y un grupo de intervención con la misma técnica anestésica, a la que se añadió un catéter intraarticular con bomba elastomérica (ropivacaína + dexketoprofeno). Se registraron variables demográficas, anestésicas y quirúrgicas, intensidad del dolor según Escala Verbal Numérica, consumo de opiáceos y complicaciones, balance articular, inicio de la deambulación y estancia hospitalaria.
ResultadosSe observó menor incidencia y severidad en la Escala Verbal Numérica en el grupo de intervención y mejor control del dolor postoperatorio (p<0,0014). El balance articular presentó resultados significativos en la flexión y el 74% de estos pacientes deambularon antes de las 36h cuando el grupo control aún no lo había hecho. El 54,1% de pacientes se mostraron «muy satisfechos» a favor del uso del catéter (p>0,001). Por último, la estancia hospitalaria disminuyó, siendo el 33,3% de los pacientes del grupo de intervención dados de alta a las 48h de la intervención, hecho que no sucedió en ninguno de los casos del grupo control.
Discusión y conclusionesEl uso del catéter intraarticular como analgesia postoperatoria es una alternativa válida y segura. Disminuye la aparición de efectos secundarios y mejora el balance articular, el inicio de la deambulación y el control del dolor y contribuye a una mayor satisfacción del paciente y a un alta más precoz.
Total primary knee arthroplasty (TKA) is one of the orthopaedic operations with the highest success rate, and leads to great satisfaction for both patient and surgeon. However, TKA is associated with considerable postoperative pain which is difficult to manage.1 The literature reports that 60% of patients have intense pain and 30% moderate pain after TKA. This pain is accentuated on moving the knee2 and as a result, patients tend to prefer to stay in hospital. This prolonged hospital stay increases medical costs and the risk of medical complications such as deep vein thrombosis or pulmonary embolism.3,4
Advances in pain management after TKA have been made to improve postoperative pain relief, with early mobilisation of the knee,5 and, in some cases, even the reduction in hospital stay.6 During the last decade, multimodal analgesia techniques have become an alternative to opioid painkillers alone for pain management after TKA.7,8
Numerous methods of adjuvant treatment for postoperative pain have been described. These include standard oral analgesics, periarticular infiltrations (with local analgesics and anaesthetics), regional anaesthesia with neuroaxial block (spinal or epidural), peripheral nerve blocks (femoral, sciatic or psoas) or a combination of various.9–11
The aim of this study is to compare two modalities in postoperative pain management as part of a multimodal pain protocol after TKA. It also assesses its impact on hospital stay, onset of walking and joint balance. To do this the use of the intraarticular catheter with elastomeric infusion (0.35% ropivacaine+5ml/h dexketoprofen) was compared with the epidural catheter (continuous perfusion of 0.2% ropivacaine at 8ml/h).
Material and methodA randomised non-blinded clinical trial was performed in patients who had undergone unilateral primary TKA who were divided into two groups: one intervention group (IG) with an intraarticular catheter and another control group (CG) with an epidural catheter. The study was approved by the Bioethics Committee and the Hospital Quality Commission and with the signed informed consent of the patients. The patients included in the study were those who had been diagnosed with tricompartmental gonarthrosis of the knee and referred for TKA. 108 patients were randomly selected from the two groups: CG and IG. The patients selected for the IG were those who had undergone surgery on even days and those of the CG on odd days. The exclusion criteria were as follows: patients allergic to NSAIDS or local anaesthetics, those who refused or had contraindications to intradural regional anaesthesia and those patients with mental, psychiatric or neuromuscular degenerative diseases.
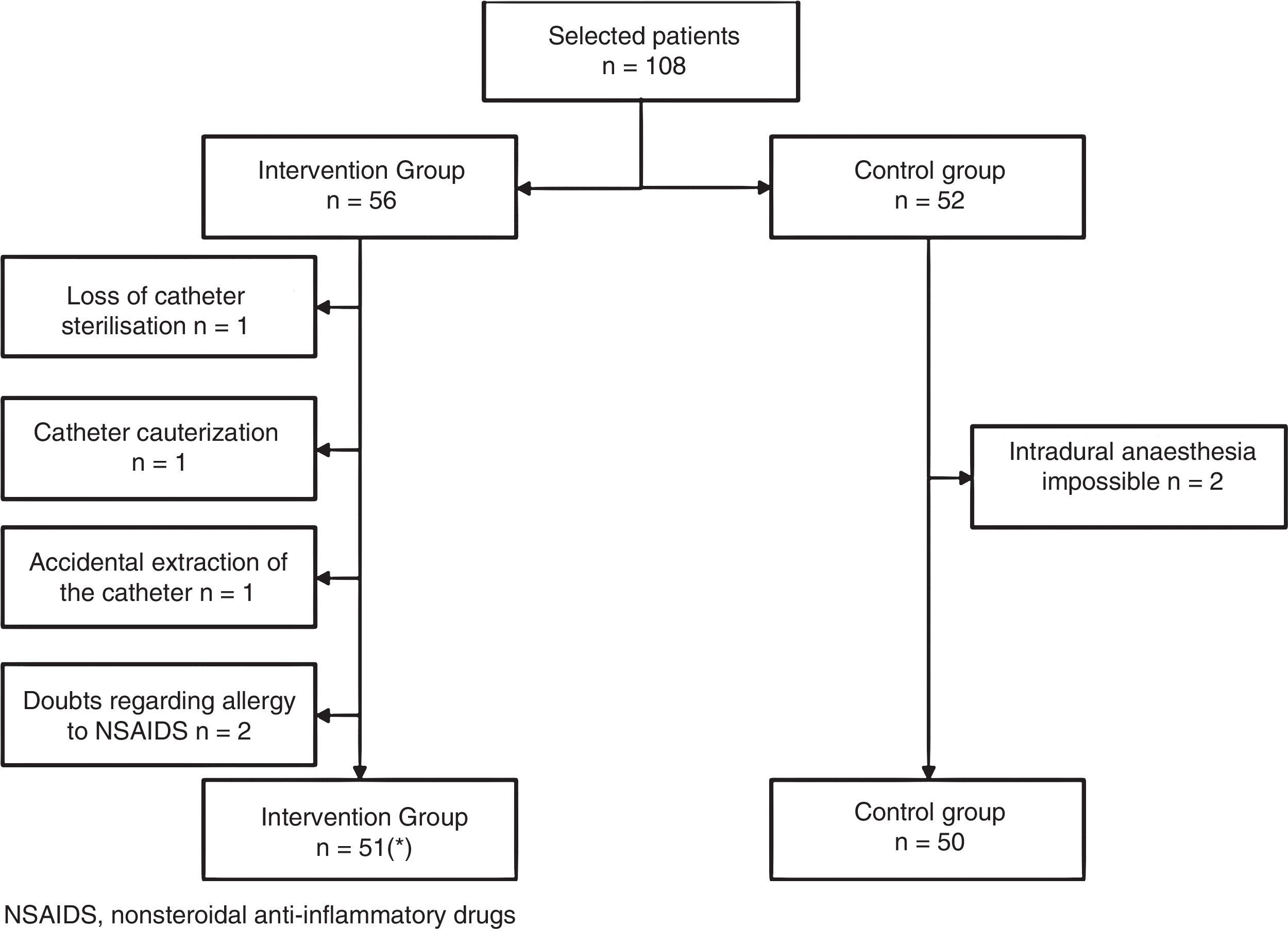
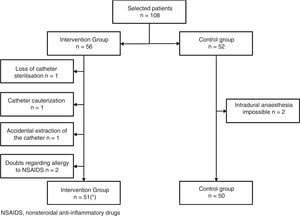
Of the 108 patients, in the CG, two had to abandon the study due to the technical impossibility of administering intradural anaesthesia. In the IG another five patients abandoned the study: three of them due to the failure of implanting the catheter in the operating theatre and two due to possible allergy to NSAIDS. This meant that the elastomeric pump could not be used in the anaesthesia recovery room. One catheter fell to the floor in the operating theatre and was no longer sterile, another was burned with an electric scalpel and in a third patient, a trocar was incorrectly removed and consequently rejected (Fig. 1).
The patients were operated on by the same group of orthopaedic surgeons and during the same period of time, which was between January and March 2016. Two knee arthroplasty models were used: PFC Sigma (Johnson & Johnson, Warsaw Ind.) and Advance Medial-Pivot (Wright Medical Technology, Arlington TN), in both study groups. The positioning of the patient, the approach and cementation type (third generation) was the same in all cases. Prophylactic ischaemia of the operated limb was used in all patients, and was removed after closing the surgical wound.
In the CG, after the intradural anaesthesia (9mg of 0.5% hyperbaric bupivacaine+10μg of fentanyl) an epidural catheter was inserted in the operating theatre with a continuous perfusion of 0.2% ropivacaine at 8ml/h. This was complemented with the intravenous administration of paracetamol and metamizol every 8h. If necessary, rescue analgesics of pethidine of 50mg were administered in intravenous boluses.
In the IG, with the same intradural anaesthesia as in the CG, the surgeon inserted an intraarticular catheter prior to closure of the arthrotomy. Following this, a continuous perfusion was initiated with an elastomeric pump composed of 0.35% ropivacaine+dexketoprofen at a constant speed of 5ml/h for 48h. This analgesic was complemented with the gradual intravenous administration of paracetamol and metamizol in the same doses as in the CG. Equally, the rescue analgesics were composed of pethidine in intravenous boluses of 50mg.
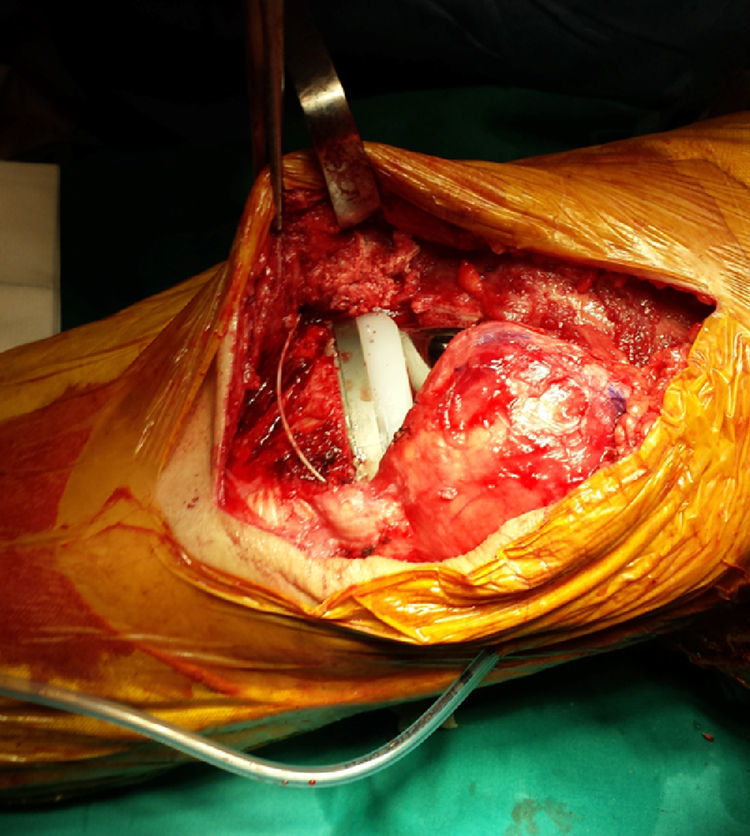
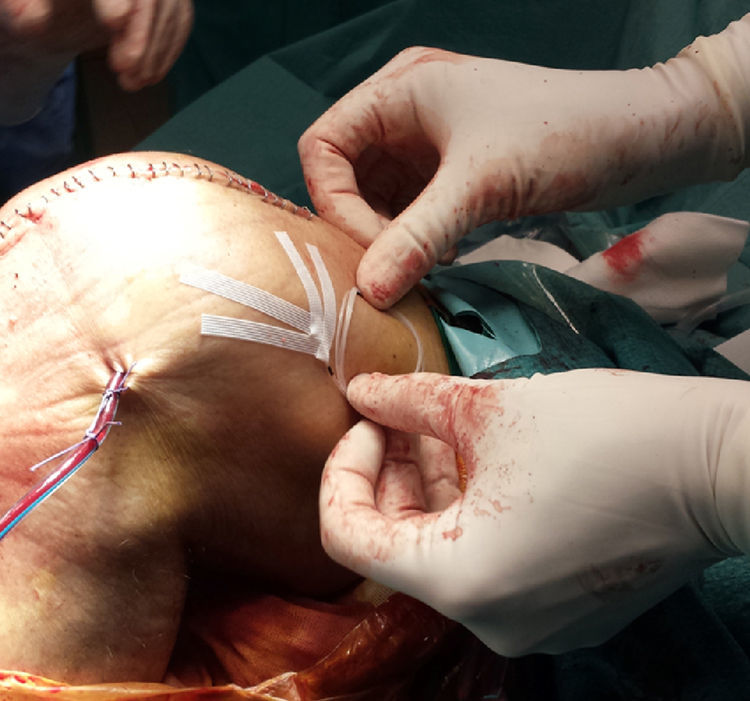
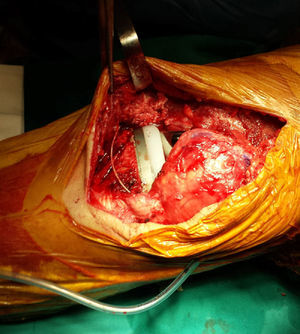
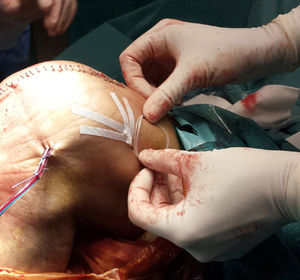
Intraarticular catheter insertion techniqueOnce the final TKA implants had been inserted and the haemostasis reviewed after removal of the prophylactic ischaemia, the intraartcular catheter was inserted (Braun Medical, Spain). The point of entry was located in the suprapatellar region external to the knee, 2–3cm proximal to the apical pulse of the kneecap, leaving the aspiration drainage exit point distal to this. The infusion segment of the catheter was positioned on the opposite side to the drainage, in the medial articular interlining (Fig. 2). After this, closure of the arthrotomy, subcutis and skin were performed. Next, the catheter was attached with an adhesive Skin-fixe Strip® (3MTM) cutaneous suture (Fig. 3). A 10ml bolus was then infused with 0.5% bupivacaine and the elastomeric pump sensor of the catheter was attached with non occlusive transparent plaster. Finally, the On-Q Pain Buster® (Lake Forest, CA, U.S.A) elastomer was attached, previously loaded with analgesia (Fig. 4). After the drainage route was opened, continuous perfusion was initiated.
Demographic variables (gender, age, side) were recorded. Pain intensity at rest and during movement was assessed after 24h and 48h using a verbal rating scale of 1–10, considering pain to be mild (under or equal to 3), moderate (from 4 to 6), and severe (over 7). Request for opioids was noted during the first 48h as were complications and side effects of each anaesthetic technique. We also recorded the degree of flexion of the operated knee, the onset of walking, the number of hospital stay days and the overall patient satisfaction on discharge (very satisfied, acceptable or dissatisfied).
For analysis of results obtained, the SAS statistical programme software version 9.4 was used (SAS Institute Inc. Cary, NC, U.S.A.). A descriptive statistic of the study variables was performed. The quantitative variables, depending on whether they followed a normal or non normal distribution, were summarised using the mean and standard deviation or the median and interquartile range, respectively. The qualitative variables were referred to in the form of a number (n) and percentage (%) using continguency tables and the X2 or exact Fisher test was applied in the case of low frequencies. Statistical significance level was established at p<.05.
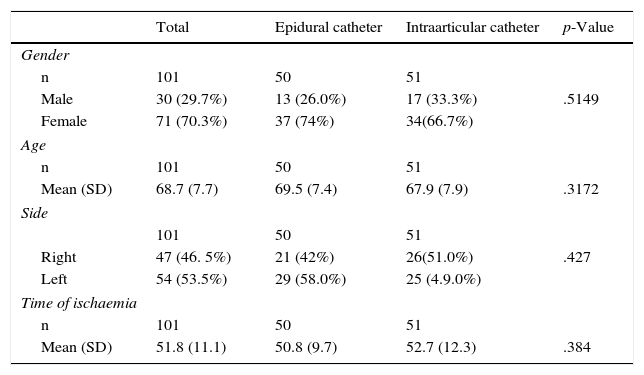
Results101 patients were included in the study, 51 (50.49%) in the case study group and 50 (59.50%) in the control group. With regards to the demographic variables studied, there were no significant differences in gender (p=.511), age (p=.317), side (p=.427) or ischaemia time (p=.384) (Table 1).
Demographic data of the study.
| Total | Epidural catheter | Intraarticular catheter | p-Value | |
|---|---|---|---|---|
| Gender | ||||
| n | 101 | 50 | 51 | |
| Male | 30 (29.7%) | 13 (26.0%) | 17 (33.3%) | .5149 |
| Female | 71 (70.3%) | 37 (74%) | 34(66.7%) | |
| Age | ||||
| n | 101 | 50 | 51 | |
| Mean (SD) | 68.7 (7.7) | 69.5 (7.4) | 67.9 (7.9) | .3172 |
| Side | ||||
| 101 | 50 | 51 | ||
| Right | 47 (46. 5%) | 21 (42%) | 26(51.0%) | .427 |
| Left | 54 (53.5%) | 29 (58.0%) | 25 (4.9.0%) | |
| Time of ischaemia | ||||
| n | 101 | 50 | 51 | |
| Mean (SD) | 51.8 (11.1) | 50.8 (9.7) | 52.7 (12.3) | .384 |
With regard to the number of requests for rescue opioid painkillers, there were no significant differences between both groups. The number of patients who required opioid rescue was 45.1% in the IG and 62% in the CG with p=.1116.
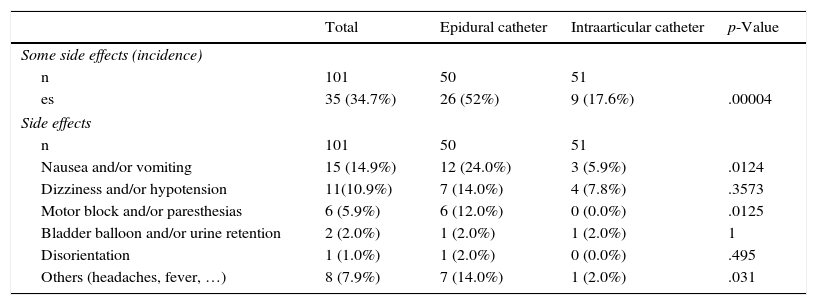
On comparing the onset of side effects, it was observed that there was a lower incidence in the IG (17.6%) than in the CG (52%), with statistically significant results (p=.00004). With respect to paresthesias/motor block, there were no cases in the IG compared with 6 (12.0%) patients in the CG. We found significant differences in the onset of nausea and/or vomiting with 12 (24%) patients in the CG compared with 3 (5.9%) in the IG. There were no differences in the rate of dizziness, low blood pressure, bladder balloon, or the onset of disorientation in space and time since the results were not statistically significant (Table 2).
Complications and side effects reported in the study.
| Total | Epidural catheter | Intraarticular catheter | p-Value | |
|---|---|---|---|---|
| Some side effects (incidence) | ||||
| n | 101 | 50 | 51 | |
| es | 35 (34.7%) | 26 (52%) | 9 (17.6%) | .00004 |
| Side effects | ||||
| n | 101 | 50 | 51 | |
| Nausea and/or vomiting | 15 (14.9%) | 12 (24.0%) | 3 (5.9%) | .0124 |
| Dizziness and/or hypotension | 11(10.9%) | 7 (14.0%) | 4 (7.8%) | .3573 |
| Motor block and/or paresthesias | 6 (5.9%) | 6 (12.0%) | 0 (0.0%) | .0125 |
| Bladder balloon and/or urine retention | 2 (2.0%) | 1 (2.0%) | 1 (2.0%) | 1 |
| Disorientation | 1 (1.0%) | 1 (2.0%) | 0 (0.0%) | .495 |
| Others (headaches, fever, …) | 8 (7.9%) | 7 (14.0%) | 1 (2.0%) | .031 |
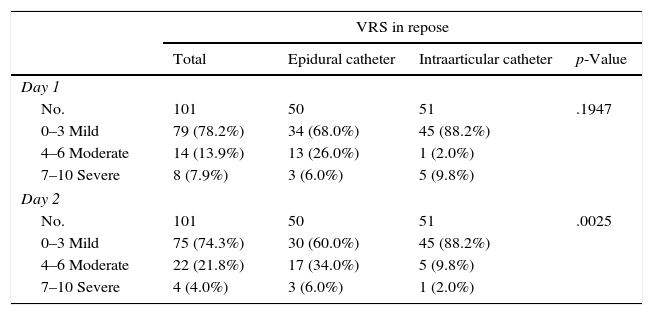
With regard to postoperative pain we observed from the verbal rating scale in the IG that there was a mean (SD) of 1.1 (1.9) compared with that of the CG with C 2.7 (2.4) on the 2nd postoperative day, with p=.0002. The following table shows the values collected on assessment of pain after 24 and 48h after TKA (Table 3).
Table with data collected regarding postoperative pain with the VRS. It was assessed after 24 and after 48h in repose and when moving.
| VRS in repose | ||||
|---|---|---|---|---|
| Total | Epidural catheter | Intraarticular catheter | p-Value | |
| Day 1 | ||||
| No. | 101 | 50 | 51 | .1947 |
| 0–3 Mild | 79 (78.2%) | 34 (68.0%) | 45 (88.2%) | |
| 4–6 Moderate | 14 (13.9%) | 13 (26.0%) | 1 (2.0%) | |
| 7–10 Severe | 8 (7.9%) | 3 (6.0%) | 5 (9.8%) | |
| Day 2 | ||||
| No. | 101 | 50 | 51 | .0025 |
| 0–3 Mild | 75 (74.3%) | 30 (60.0%) | 45 (88.2%) | |
| 4–6 Moderate | 22 (21.8%) | 17 (34.0%) | 5 (9.8%) | |
| 7–10 Severe | 4 (4.0%) | 3 (6.0%) | 1 (2.0%) | |
| VRS in movement | ||||
|---|---|---|---|---|
| Total | Epidural catheter | Intraarticular catheter | p-Value | |
| Day 1 | ||||
| No. | 101 | 50 | 51 | .3341 |
| 0–3 Mild | 51 (50.5%) | 21 (42.0%) | 30 (58.8%) | |
| 4–6 Moderate | 26 (25.7%) | 17 (34.0%) | 9 (17.6%) | |
| 7–10 Severe | 24 (23.8%) | 12 (24.0%) | 12 (23.5%) | |
| Day 2 | ||||
| No. | 101 | 50 | 51 | .0155 |
| 0–3 Mild | 48 (47.5%) | 18 (36.0%) | 30 (58.8%) | |
| 4–6 Moderate | 36 (35.6%) | 20 (40.0%) | 16 (31.4%) | |
| 7–10 Severe | 17 (16.8%) | 12 (24.0%) | 5 (9.8%) | |
On exploring the level of the articular balance of the operated knee, in the IG we observed greater knee flexion during the first 24h. 21.7° more in flexion (p<.0001) was achieved compared with the CG.
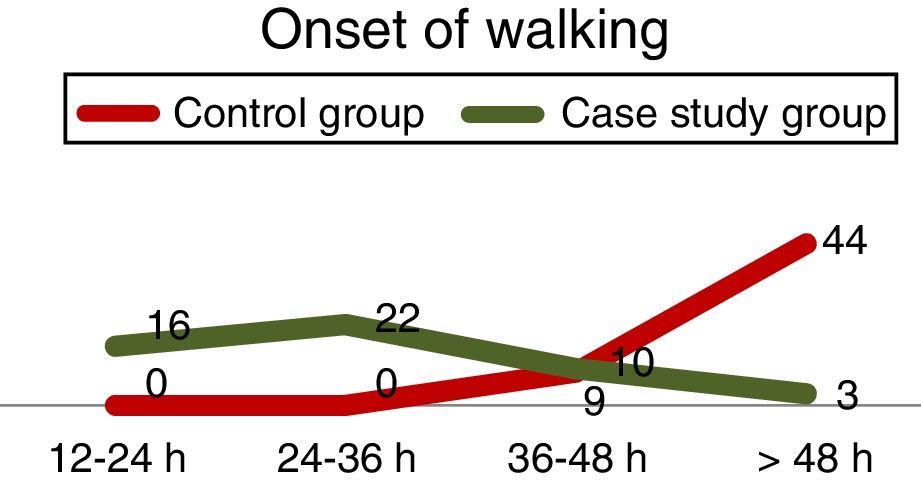
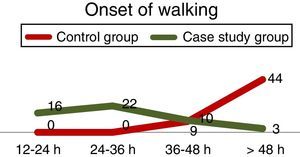
74% of patients with an intraarticular catheter, were able to walk when the CG patients had not started to do so (31.4% in the first 12h after surgery and 43.1% within 12 and 24h) with p<.001 (Fig. 5).
With regard to satisfaction, there were double “very satisfied” patients in favour of the use of the intraarticular catheter (28; 54.9%) compared with the CG (14; 28.8%).
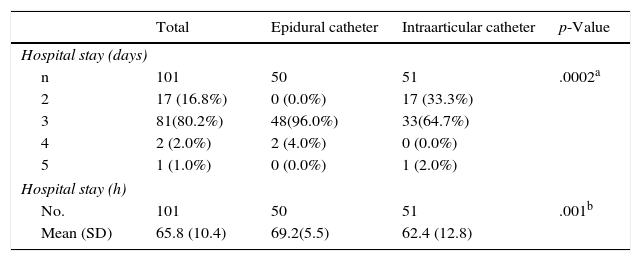
Lastly, hospital stay considerably dropped in the IG with a mean (SD) of 62.4 (12.8)h compared with 69.2 (5.6)h for the CG (p=.001), with 33.3% of patients being discharged within the first 48h, compared with 0% of the control group (Table 4).
Data on hospital stay in days and hours.
Postoperative analgesia after TKA is an essential part in achieving success, since it impacts posterior rehabilitation of the patient and the quality of this healthcare procedure. The result obtained in this work, with lower hospital stay, indicates that the use of the intraarticular catheter, and the postoperative analgesia is a highly appropriate technique for a rapid recovery system in knee arthroplasty. This entails saving money without increasing complications, as has now been internationally recognised.12,13
Primary TKA is one of the orthopaedic operations with the highest success rate and leads to great satisfaction for the patient and the surgeon. For this reason, postoperative analgesia using these processes is now an essential part of this success, since it has an impact on posterior rehabilitation of the patient and in the quality of this healthcare process.
After an exhaustive review of the literature, we found another study which compares the efficacy of postoperative control of pain of patients who underwent primary TKA with the use of the intraarticular catheter and the epidural catheter. A randomised study was carried out to this effect to compare postoperative pain, the use of analgesics, the functioning of the operated knee, the onset of walking, hospital stay duration and the appearance of complications immediately after surgery.
Pain assessment was made on a verbal rating scale on the first and second postoperative day, on the assumption that the highest differences would be found, since after the first 48h following surgery the effects of both analgesics would cease.9,14,15
Although no other study used the same pain management protocols, similar studies compared periarticular injection with nerve blocks and showed outcomes similar to our study. In a recent clinical trial Chaumeron et al.16 used a periarticular infiltration in a single dose, which was repeated through an intraarticular catheter on postoperative day 1 and was compared with a permanent femoral catheter (with no sciatic block) used from 48 to 72h. This study reported a lower pain score for the first 8h after surgery in the periarticular infiltration group and no differences after that, with improvement in quadriceps strength and mobility in the said group. Carli et al.17 compared local infiltration with femoral block and no significant differences were shown in pain intensity in repose or consumption of opioids after TKA. We did observe a reduction in pain when the patients started to walk with femoral block. In contrast, in Toftdahl et al.18 study they found better results in patients who received periarticular injection compared with those who received femoral nerve block during the first postoperative day.
When the studies with intraarticular injection and intraoperative periarticular infiltration were compared after the closure of the capsule, the consumption of narcotics was generally lower in intraarticular infiltration studies, although the difference tended to be greater for periarticular infiltrations. The differences of the pain scores are, generally, more inclined towards periarticular infiltrations.14,18
With regard to the need for opioid rescue, there was no significant difference between IG and CG in the first 48h after surgery. Vendittoli et al.19 compared the consumption of morphine during the first 24h after a TKA in 42 patients who had been randomly assigned to receive a mixture of perioperative articular infiltration with local anaesthesia and self-administered morphine or only self-administered morphine. As with our study, they observed that in the patient group with articular infiltration, pain lessened and side effects were minimalised.
The use of the intraarticular catheter, apart from improving postoperative analgesia, achieves a significant improvement in early onset of walking for the patient, and a reduction in hospital stay (2.6 days). In a transversal study carried out on a global scale, and by autonomous community out of the total primary arthroplasty of the hip (THA) and TKA reported by Allepuz et al.,20 the median stay was 9 days for THA and 8 days for TKA. Brunenberg et al.19,21 studied the cost-effectiveness of patients who underwent TKA and ATC. Mean hospital stay of the patients who were treated later with physiotherapy was lower than that of patients who did not receive this treatment (the difference was 4.1 days in hip and 6.9 days in knee, with statistically significant differences).
Several studies have shown that there is not a higher risk of infection when an intraarticular catheter is inserted up to 72h,19,22 and they may even be used for the treatment of prosthetic infection in the hip and knee with antibiotic infusion.23
Our study had several limitations. We could not prevent the patients and the staff being aware of the analgesic treatment received, since the presence of both the intraarticular catheter and the epidural catheter made it clear to which study group they belonged.
The patients were not operated on by the same surgeon, despite them all belonging to the same working team, and this was a limitation to the study. Moreover, for this study two different prosthesis models were used: PFC Sigma (Johnson & Johnson, Warsaw Ind.) and Advance Medial-Pivot (Wright Medical Technology, Arlington TN).
After the outcome obtained with data analysis, we may say that the use of the intraarticular catheter in patients who undergo a total primary knee arthroplasty as postoperative analgesia is a valid and safe alternative, with improvement in immediate postoperative pain. This means a better range of movement in the operated knee, that the onset of walking is earlier, there is a reduction in the onset of the before-mentioned side effects, patient satisfaction improves and hospital stay is reduced.
We therefore conclude that the use of the intraarticular catheter as a postoperative analgesic technique improves the outcomes compared with the use of the epidural catheter, and it is therefore an effective alternative in the treatment of postoperative pain after total knee arthroplasty.
Level of evidenceLevel of evidence III.
Ethical responsibilitiesProtection of people and animal subjectsThe authors declare that the procedures followed comply with the ethical regulations of the responsible human experimentation committee and with the World Medical Association Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have adhered to the protocols of their centre of work on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
This study has been possible thanks to the support and collaboration of all our colleagues of the Orthopaedic Surgery and Traumatology, Anaesthesiology and Nursing Services of the Hospital San Juan de Dios del Aljarafe, to whom I express my most sincere gratitude.
Please cite this article as: Cáceres-Sánchez L, García-Benítez JB, Coronado-Hijón V, Montero-Pariente M. Uso de cáteter intraarticular en fast track de artroplastia primaria de rodilla. ¿Supone un avance? Rev Esp Cir Ortop Traumatol. 2018;62:19–26.