Frailty scores have not been standardised for the preoperative assessment of patients undergoing total knee replacement (TKR). The aim of this study was to compare the efficacy of the American Society of Anesthesiology (ASA) score, the Charlson comorbidity index (ICC) and the simple frailty score (SSF) in predicting complications, hospital stay, readmissions and mortality after elective TKR.
Materials and methodsWe retrospectively studied 448 patients who underwent TKR for osteoarthritis at our institution between 2016 and 2019. They were divided into two groups: Group A (263 patients, <80 years) and Group B (185 patients, >80 years).). All were classified by ASA, ICC and SSF scores.
ResultsThe ICC was higher in Group B (median 5 [RI: 4–6] vs. 4 [RI: 3–5]; p<.001); however, it was not associated with a higher number of complications. When performing a logistic regression analysis we found, for complications: OR SSF=0.67; ICC=1.11; ASA 3 & 4=0.89 and age=1.04; while for readmissions: OR SSF=2.09; ICC=1.01; ASA 3 & 4=0.79 and age=1.
ConclusionsThe ICC and SSF scales showed no differences to the ASA scale in the prediction of readmissions, complications and hospital stay. However, the SSF seems to have a better correlation in predicting unplanned readmission.
Las escalas de valoración de fragilidad no han sido estandarizadas para la evaluación prequirúrgica de pacientes sometidos a un reemplazo total de rodilla (RTR). El objetivo de este estudio fue comparar la eficacia de la escala de valoración de la Sociedad Americana de Anestesiología (ASA), el índice de comorbilidad de Charlson (ICC) y la escala simple de fragilidad (SSF) en la predicción de complicaciones, estancia hospitalaria, reingresos y mortalidad después del RTR electivo.
Materiales y métodosEstudiamos retrospectivamente a 448 pacientes que se sometieron a un RTR por artrosis en nuestra institución entre 2016 y 2019. Estos se dividieron en dos grupos: grupo A (263 pacientes <80 años) y grupo B (185 pacientes >80 años). Todos fueron clasificados por escalas de ASA, ICC y SSF.
ResultadosEl ICC fue mayor en el grupo B (mediana: 5 [RI: 4-6] vs. 4 [RI: 3-5]; p <0,001); sin embargo, no se asoció con un mayor número de complicaciones. Al realizar un análisis de regresión logística encontramos, para las complicaciones: OR SSF=0,67; ICC=1,11; ASA 3 y 4=0,89 y edad=1,04; mientras que para los reingresos: OR SSF=2,09; ICC=1,01; ASA 3 y 4=0,79 y edad=1.
ConclusionesLas escalas ICC y SSF demostraron no presentar diferencias a la escala de ASA en la predicción de reingresos, complicaciones y estancia hospitalaria. Sin embargo, el SSF parece tener una mejor correlación en la predicción de la readmisión no planificada.
With increasing life expectancy in the general population has come increasing numbers of total knee replacements (TKRs). This trend is expected to continue over the next decade, although the most recent predictive models have shown less growth than predicted by Kurtz et al. in 2007 (3.48 million annual RTRs in the US by 2030),1 with a projection estimated by Shichman et al. of 791,760 annual TKRs by 2030.2
Comorbidities are defined as diseases or medical conditions unrelated to the principal diagnosis, but coexisting with the disease of interest. It is important to identify them in patients, and even more so in the elderly, as they can delay diagnosis, modify treatment, lead to predictable complications, and alter patient or implant survival.3 There is a strong correlation between comorbidities, complications,4 and mortality.5 In this regard, rating scales offering good reliability and validity have been proposed that assess comorbidities, estimating a degree of severity of the patient's health status.
The American Society of Anaesthesiologists (ASA) physical status classification is widely used, not only by anaesthesiologists, but also by physicians from other specialties, to determine the patient's intraoperative physical status.6 While this score has proven to be beneficial as a measure of the risk of intraoperative and postoperative non-orthopaedic complications,7 mortality, cost, and length of hospital stay,8 it can be inaccurate and unreliable.9,10
On the other hand, there are publications that report evidence concerning the use of frailty assessment scales in elderly subjects who will undergo TKR with good reliability.11–13 Frailty rating scales, such as the Simple Frailty Scale (SSF), have been implemented in the geriatric population for decades and have begun to gain importance to predict various kinds of complications.14
The Charlson Comorbidity Index (CCI) quantifies the impact comorbidities have on survival.15 It has been used extensively in large studies based on administrative data to predict functional outcome,16 mortality,17 and length of hospital stay, and resource use.18
We are unaware of any studies in the literature that compare these scores in elderly patients undergoing joint replacement. Therefore, the aim of this paper is to compare the accuracy of the ASA, CCI, and FFS score in predicting complications, contrasting a group of octogenarian patients with a group of septuagenarian patients who underwent elective TKR.
Material and methodsWe retrospectively analysed 448 patients who underwent TKR at our institution between January 2016 and December 2019. Only patients with a preoperative diagnosis of primary knee osteoarthritis were included. Patients who underwent bilateral TKR, a diagnosis of tumour disease, revision surgery, fractures, or a history of previous surgery were excluded. All information pertaining to this investigation was prospectively stored in the electronic medical record and reviewed by four researchers.
The participants were divided into a control group: individuals under the age of 80 years vs. the study group; i.e., those over the age of 80 years (control group A: 263 subjects vs. study group B: 185 patients, respectively). Preoperative assessment was carried out by clinicians specialised in elderly patients, as well as by anaesthesiologists. The ICC and SSF,13,19 as well as the preoperative ASA rating scale20 were used to define patients’ frailty. Comorbidities were divided into eight groups for further analysis: (1) Cardiovascular, (2) Respiratory, (3) Neurological, (4) Smoking, (5) Dyslipidaemia, (6) Oncological, (7) Diabetes, and (8) Other.
All patients received antibiotic (cefazolin at anaesthetic induction and 3 doses of 1g immediately postoperatively) and antithrombotic (subcutaneous enoxaparin, 40mg/24h during the first postoperative month) prophylaxis. All surgeries were performed in an operating theatre with laminar flow, under hypotensive spinal anaesthesia, via a medial parapatellar approach. After closure, the surgical site was infiltrated with a cocktail of ropivacaine, triamcinolone, morphine, adrenaline, and tranexamic acid. The dose was adjusted according to each individual's kidney function at the discretion of the anaesthesiologist.
The rehabilitation protocol included full weight-bearing mobilisation with walkers from the first postoperative day. Patients returned to normal daily activities within the first postoperative weeks, according to their clinical and radiographic evolution. Anteroposterior and lateral knee radiographs were obtained immediately postoperatively, at 6 and 12 months, and were analysed by the 4 investigators independently. All 4 observers analysed both groups of patients. In controversial cases where the review of the images could raise doubts about the outcome, an additional analysis by another observer was performed. However, the final decision was the responsibility of one of the principal investigators (JC). In all patients, the staples were removed 2 weeks after surgery.
The Visual Analogue Scale (VAS) and the Knee Society Score (KSS)21 were used to monitor postoperative clinical progress. These were completed by senior surgeons preoperatively and one month and one year after surgery.
Analysis of complicationsBoth medical and surgical complications were recorded and analysed. Comorbidities were categorised and defined into eight groups as detailed above.
Postoperative length of stay, need for blood transfusions, unplanned readmissions, and in-hospital and out-of-hospital complications within the first 90 postoperative days were evaluated. We used the modified Clavien–Dindo classification22 to capture complications and divided them into two classes according to severity: grades I and II include minor complications that require no treatment or only pharmacological intervention; grades III and IV are major complications, necessitating surgical intervention or life support; grade V complications result in patient demise.23,24
Statistical analysisPreoperative and postoperative scores were compared using the paired t-test for independent samples. Continuous variables are reported as medians and standard deviations, while categorical variables are expressed as absolute and relative frequencies. For statistical purposes, Student's t-test with a 95% confidence interval was used to calculate intergroup differences for both functional scores and complications. Statistical analysis was performed with IBM SPSS® Statistics 26.0 software (IBM Corp., Armonk, NY, USA). p values of less than 0.05 were regarded as statistically significant.
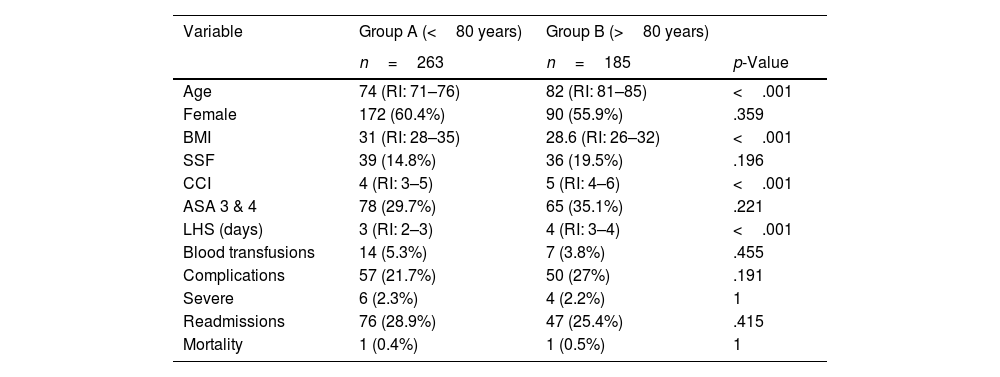
ResultsThe median age of group A was 74 years (interquartile range [IR]: 71–76) and for group B, it was 82 (IR: 81–85) years. Group A consisted of 60.4% women, whereas females accounted for 55.9% of group B (p=0.359). No patients were lost to 90-day follow-up.
Group B had an ICC score of 5 (IR: 4–6), while it was 4 (IR: 3–5) in group A; thus, it significantly higher in group B (p<0.001). Furthermore, a higher frailty index was recorded in group B: 36 (19.5%) were classified as frail, while 39 (14.8%) were classified as frail in group A (p=0.196). Seventy-eight (29.7%) and 65 (35.1%) patients were ASA 3 & 4 in group A and B, respectively, exhibiting no significant differences between the two groups (p=0.221). The rest of the demographic information is detailed in Table 1.
Demographic information.
| Variable | Group A (<80 years) | Group B (>80 years) | |
|---|---|---|---|
| n=263 | n=185 | p-Value | |
| Age | 74 (RI: 71–76) | 82 (RI: 81–85) | <.001 |
| Female | 172 (60.4%) | 90 (55.9%) | .359 |
| BMI | 31 (RI: 28–35) | 28.6 (RI: 26–32) | <.001 |
| SSF | 39 (14.8%) | 36 (19.5%) | .196 |
| CCI | 4 (RI: 3–5) | 5 (RI: 4–6) | <.001 |
| ASA 3 & 4 | 78 (29.7%) | 65 (35.1%) | .221 |
| LHS (days) | 3 (RI: 2–3) | 4 (RI: 3–4) | <.001 |
| Blood transfusions | 14 (5.3%) | 7 (3.8%) | .455 |
| Complications | 57 (21.7%) | 50 (27%) | .191 |
| Severe | 6 (2.3%) | 4 (2.2%) | 1 |
| Readmissions | 76 (28.9%) | 47 (25.4%) | .415 |
| Mortality | 1 (0.4%) | 1 (0.5%) | 1 |
ASA: American Society of Anaesthesiology; LHS: length of hospital stay; CCI: Charlson comorbidity index; BMI: body mass index; IR: interquartile range; SSF: simple frailty score.
When quantifying days of hospitalisation, we detected significant differences. The median was 3 (IR: 2–3) for group A and 4 (IR: 3–4) for group B, with a p<.001. We found no significant difference in the number of blood transfusions required between both groups (A=5.3 vs. B=3.5%; p=0.455).
On the basis of the Clavien–Dindo classification, there were 107 complications during hospitalisation. Fifty-seven (21.7%) in group A and 50 (27%) in group B with only 6 (2.3%) and 4 (2.2%) serious complications, respectively; in the former, there was one death (p=0.19). Perhaps some complications were over diagnosed relative to other studies.
There was no significant difference in 90-day unplanned readmissions for complications between the two groups, with 76 (28.9%) and 47 (25.4%) for groups A and B, respectively (p=.41). Ninety-day mortality was 0.4% for group A and 0.5% for group B, with one patient in each group (p=1).
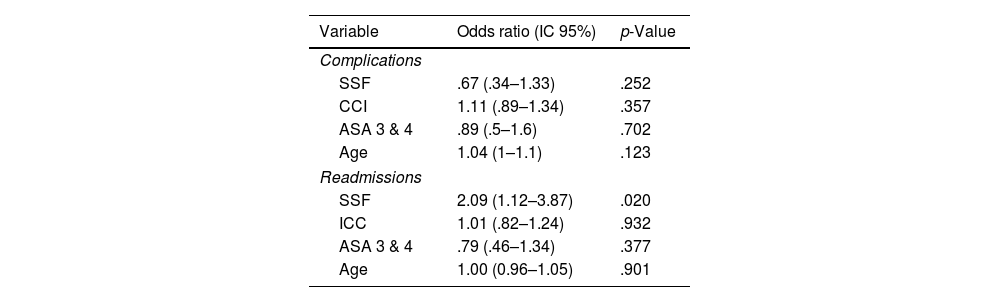
After performing logistic regression analysis, we found that none of the scales nor the parameter age proved to be superior to the other in predicting complications: SSF OR: 0.67 (0.34–1.33; p=.252), CCI OR: 1.11 (0.89–1.34; p=.357), ASA 3 & 4 OR: .89 (.5–1.6; p=.702), and age OR: 1.04 (1–1.1; p=.123).
However, when it came to predicting readmissions, the SSF (OR: 2.09 [1.12–3.87]; p=.020) was superior to the CCI (OR: 1.01 [0.82–1.24]; p=.932), ASA 3 & 4 (OR: 0.79 [0.46–1.34]; p=.377), or age (OR: 1 [0.96–1.05]; p=.901) (Table 2). We found that no score correlated with the number of days of hospitalisation or number of transfusions patients required.
Logistic regression of the three scales assessed (SSF, CCI, and ASA), and age on postoperative complications and readmissions.
| Variable | Odds ratio (IC 95%) | p-Value |
|---|---|---|
| Complications | ||
| SSF | .67 (.34–1.33) | .252 |
| CCI | 1.11 (.89–1.34) | .357 |
| ASA 3 & 4 | .89 (.5–1.6) | .702 |
| Age | 1.04 (1–1.1) | .123 |
| Readmissions | ||
| SSF | 2.09 (1.12–3.87) | .020 |
| ICC | 1.01 (.82–1.24) | .932 |
| ASA 3 & 4 | .79 (.46–1.34) | .377 |
| Age | 1.00 (0.96–1.05) | .901 |
ASA: American Society of Anaesthesiology; 95% CI: 95% confidence interval; CCI: Charlson comorbidity index; SSF: simple frailty score.
Based on this study and our experience with octogenarians and septuagenarians undergoing TKR at the Hospital Italiano de Buenos Aires (HIBA), high CCI and SSF scores are associated with higher mortality rates, and SSF is correlated with a greater risk of hospital readmission. The ASA score was not found to have any predictive value for either of these parameters; similarly, neither did the CCI, SSF, or ASA scores prove to be good predictors of blood loss or severity of complications.
The ASA rating scale continues to be used by many institutions to identify patients who may require further work-up or preoperative testing.25 Although it is a rating scale that aims to standardise the patient's physical status classification, in many cases it is open to subjectivity and there are discrepancies between clinicians as to which ASA value each patient belongs to.26
Other studies have attempted to determine the usefulness of frailty rating scales in predicting the outcome of patients undergoing surgery. For example, Traven et al. published an analysis of the modified 5-factor frailty index (mFI-5) in 2019. This includes the presence of congestive heart failure, diabetes mellitus, concurrent chronic obstructive pulmonary disease or pneumonia, hypertension requiring medication, and dependency for activities of daily living in the 30 days prior to surgery. Their results suggest that it is an effective tool for predicting complications including life-threatening complications, surgical site infections, readmission, and mortality in these patients.13
Runner et al. also conducted an analysis of the association of the modified frailty index (mFI) with outcomes after RTR in 2017.12 This study evaluated 90,260 patients from multiple institutions and found that the higher the mFI, the higher the risk of mortality, complications and hospital readmissions.
In contrast to the present study, in these two series, the participants were treated at different institutions by different teams, with only a 30-day follow-up period and lacking a standardised protocol to evaluate complications. In our series, we analysed subjects who belonged to the Health Plan of the HIBA, who were treated exclusively at our centre by the same team and who underwent evaluation up to 90 days following surgery. This may also account for the high rate of complications detected in our cohort. We recorded the various degrees of complications, major complications as well as minor complications that only required wait-and-see or medical-pharmacological treatment, and even readmission to hospital for any reason during the follow-up period.
Finally, McConaghy et al. conducted a study of 202,488 patients undergoing total hip replacement (THR) and 230,823 primary THR between 2011 and 2019, and rated the value of four scales (mCCI, ASA, ECM, and mFI-5) to predict mortality, the rate of both major and minor complications at 30 days, prolonged hospital stay (more than one day), and discharge care requirements (discharge to outside the home).27 In this study, they found that only the mCCI and ASA were good predictors of mortality, with all four scales being poor predictors for all other variables contemplated. The mFI-5 is of particular note, inasmuch as these findings are contradictory to those published by Traven et al. who stated that it is a robust predictor of all-complications, readmission, and 30-day mortality after THR and TKR, as detailed above. McConaghy et al. state that this difference may be due to the fact that Traven et al. did not calculate the C-statistic or other measures of discriminative ability, concluding that their assessment of the clinical usefulness of mFI-5 is limited.
Identifying low-risk patients has recently become increasingly important given the rise of joint replacement surgeries with a single day of admission or even same-day discharge. This upward trend, prompted by the needs of the healthcare system during the COVID-19 pandemic and the need to reduce the costs associated with this type of procedure, is underpinned by evidence that in suitably selected patients, it is a safe and effective procedure, as demonstrated by Bovonratwet et al. in their series of 1005 patients over 80 years of age with a rapid recovery protocol,28 and Varady et al. in their study population involving 1418 of the same age group who were discharged on the same day as surgery or the following day.29
The present study, thanks to the number of patients evaluated and the extended follow-up period (90 days), established that there is an association between complications, unplanned readmissions, and mortality with the CCI and the SSF. In contrast, the popularly used ASA rating scale failed to exhibit any relationship. It should be noted that, regardless of the fact that complications and unplanned readmissions are similar in both groups, our results demonstrate that patient age should not be regarded as a factor to be taken into account when contraindicating surgery.30
We believe our study has certain limitations: owing to its retrospective nature, it is prone to beta-errors. Nevertheless, the data were collected from an electronic medical record that captures data prospectively and with an anaesthesiology chart that monitors the patient's vital signs and events during surgery in real time. We believe that data loss errors are minimised. Although the sample is somewhat modest, we included all subjects who underwent surgery since the introduction of this electronic data collection system. No participants were lost to follow-up as they were all insured by the institutional health insurance and considered to be a captive population. Even when we evaluated emergency room readmissions, we believe that we have quantified more complications than other studies in the literature that did not take this type of readmission into account.
ConclusionThe CCI and SSF scales displayed no difference compared to the ASA scale when it comes to the prediction of readmissions, complications, and length of hospital stay. However, the SSF appears to correlate better when predicting unplanned readmission.
We believe that preoperative assessment in octogenarian patients should be completed with geriatric assessment scales such as the CCI and SSF, not only with the routine ASA.
FundingThis research has not received any specific support from public sector agencies, the commercial sector, or non-profit organisations.
Level of evidenceLevel of evidence iii.
Conflict of interestsThe authors have no conflict of interests to declare.
Right to privacy and informed consentThe authors have obtained informed consent from the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Ethics committee approvalApproved by the Ethics Committee for Research Protocols (CEPI) Registration No. #6184.