Modular neck primary stems were introduced with the theoretical advantage of restoring the hip anatomy more precisely. However, the presence of a second junction has been associated with increased corrosion and release of metal debris. The objective of our study is to quantify of chromium and cobalt serum values, and to analyse their temporal evolution during five years.
Material and methodsWe present a prospective series of 61 patients who underwent primary total hip arthroplasty by implantation of the H MAX-M® stem (Limacorporate, San Daniele, Italy). Serum chromium and cobalt determinations were performed at six months, two years and five years.
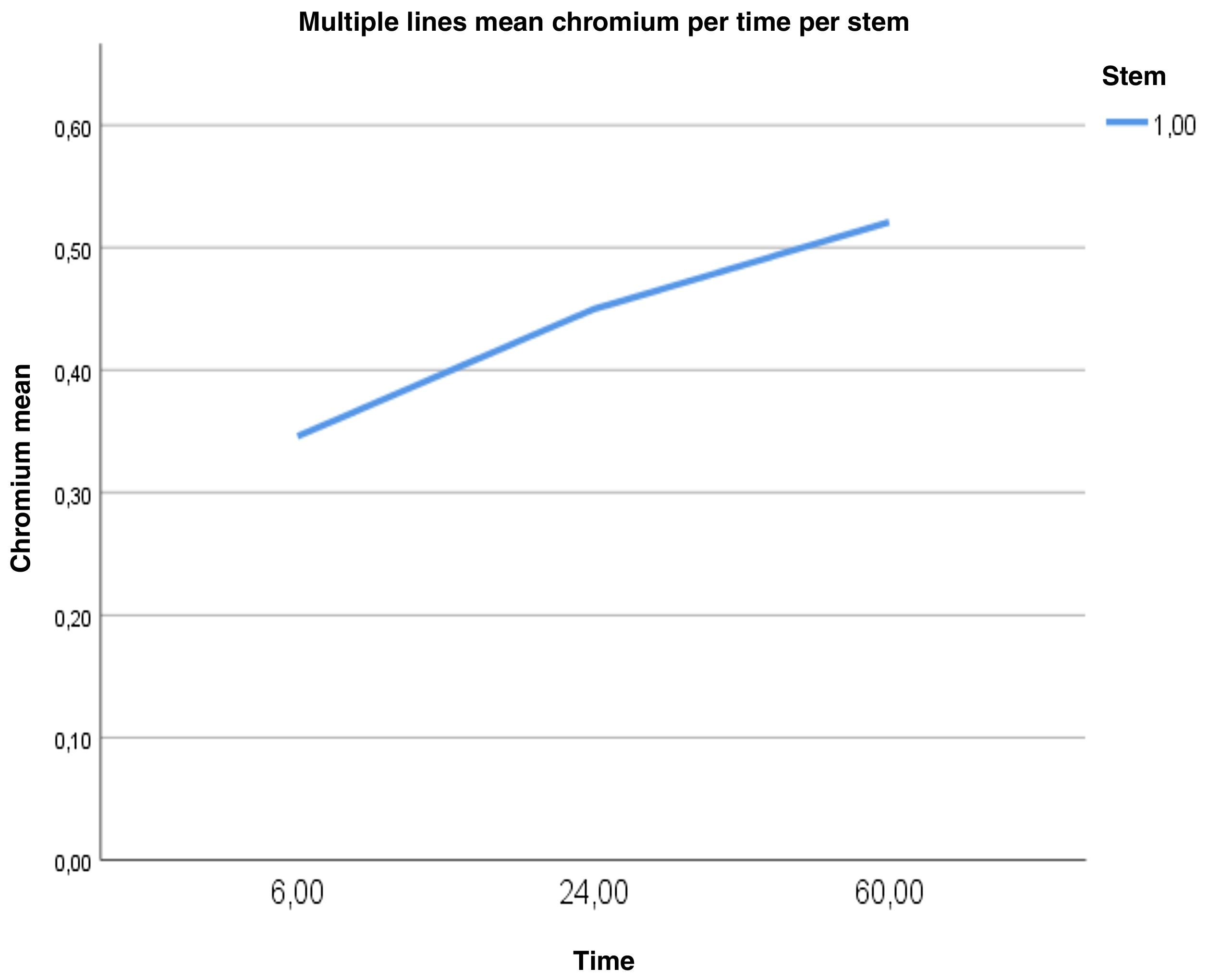
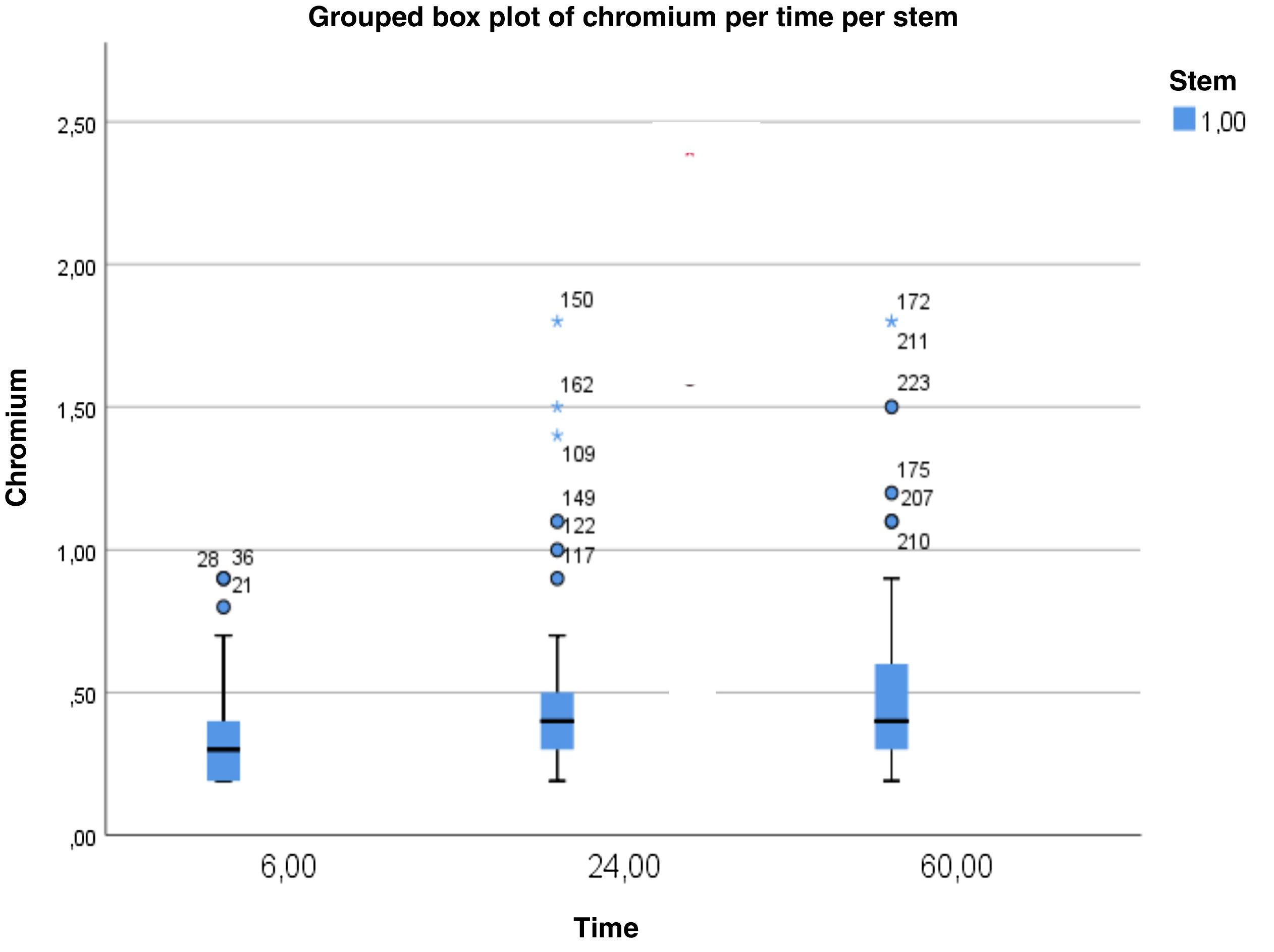
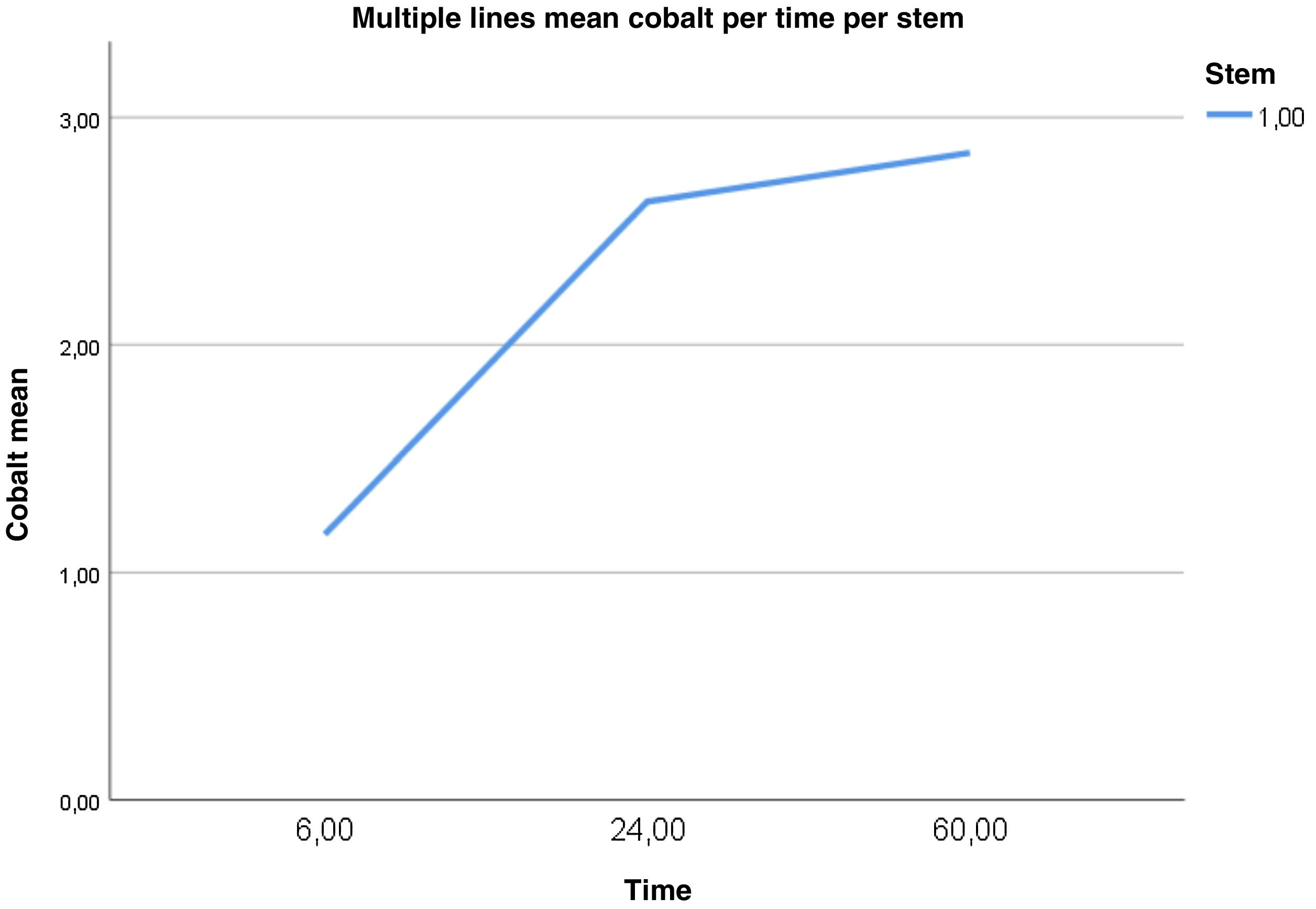
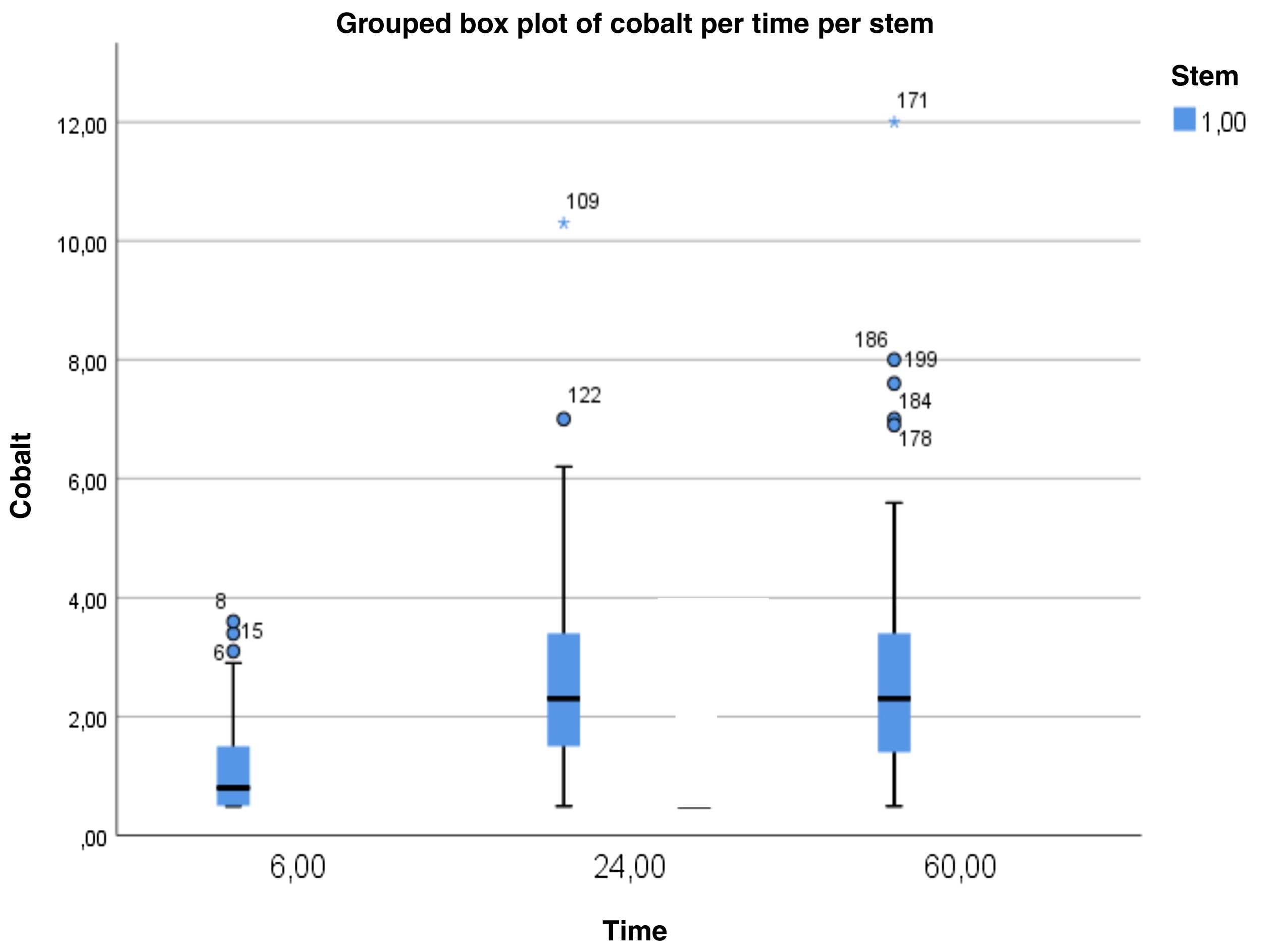
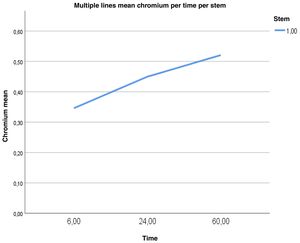
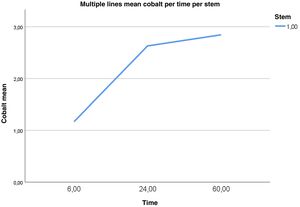
ResultsOur series shows a progressive elevation in chromium levels with a significant difference between chromium values at six months (0.35±0.18) and five years (0.52±0.36), p=.01. Regarding cobalt, a statistically significant elevation is observed between six months and two years and a subsequent stabilisation of values between two and five years, with a cobalt mean at six months (1.17±0.8) significantly lower than at two (2.63±1.76) and five years (2.84±2.1), p=.001.
ConclusionElevated serum cobalt levels have been observed in patients who underwent modular neck stem implantation. The results obtained in this study have limited the use of stems with a modular neck in our clinical practice.
Los vástagos primarios con cuellos modulares fueron introducidos con la ventaja teórica de restaurar la anatomía de la cadera de forma más precisa. Sin embargo, la presencia de un segundo encaje se ha asociado a una mayor corrosión y liberación de detritos metálicos. El objetivo de nuestro estudio es cuantificar los valores séricos de cromo y de cobalto, y analizar su evolución temporal durante cinco años.
Material y métodosSe presenta una serie prospectiva de 61 pacientes intervenidos de artroplastia total de cadera primaria mediante la implantación del vástago H MAX-M® (Limacorporate, San Daniele, Italia) en los que se realizó una determinación sérica de cromo y cobalto a los seis meses, a los dos años y a los cinco años.
ResultadosNuestra serie presenta una elevación progresiva de los niveles de cromo, con una diferencia significativa entre los valores de cromo a los seis meses (0,35±0,18) y a los cinco años (0,52±0,36), p=0,01. Respecto al cobalto, se observa una elevación estadísticamente significativa entre los seis meses y los dos años y una posterior estabilización hasta los cinco años, siendo la media de cobalto a los seis meses (1,17±0,8) significativamente menor que a los dos años (2,63±1,76) y a los cinco años (2,84±2,1), p=0,001.
ConclusiónSe ha observado una elevación de los niveles séricos de cobalto en aquellos pacientes a los que se les implantó un vástago con cuello modular. Los resultados obtenidos en este estudio han limitado el uso de vástagos con cuello modular en nuestra práctica habitual.
Joint replacement surgery is based on continuous modifications of designs and materials to maximise implant longevity and improve clinical–functional outcomes. In 1985, Cremascoli introduced the concept of the bimodular neck by designing the first stem with a double socket: head-neck and neck-stem. These stems with modular necks had the theoretical advantage of restoring the hip anatomy more accurately, through a more accurate adjustment of the hip centre of rotation and allowing intraoperative changes in angulation, version, and neck length.1 However, more recent publications have shown that bearing surfaces are not the only source of metal oxide debris, but that sockets between different parts are also susceptible to corrosion due to micromotions at the interface.2
On the one hand, solid metal particles are released, triggering an immune response that degrades the extracellular matrix.3 The adverse reaction to metal debris includes a wide spectrum of phenomena: fibrosis, metallosis, lesions associated with aseptic lymphocytic vasculitis, pseudotumours, and osteolysis.3,4 They are also capable of triggering delayed type 4 hypersensitivity reactions in susceptible patients. On the other hand, electrochemical changes occurring at the level of the modular sockets release metal ions in addition to those released by phagocytes after exposure of solid particles to the acidic pH of lysosomes. Corrosion phenomena at the level of the socket are more active because of the greater number of ionised residues.4 In the human organism, when present in high amounts, these metal ions are capable of triggering hypersensitivity reactions, as well as inducing cytotoxicity, oxidative stress, and cell death.5 In other words, cobaltism can affect different organs, leading to multi-organ failure and death of the patient.6
Several models of stems with modular necks have been withdrawn from the market due to pain, adverse reaction to metal debris (ARMD), and implant breakage.7 However, there are stems with modular necks that have shown satisfactory functional results and a low complication and revision rate. Therefore, we must take into consideration that not all designs and materials are the same and results should not be generalised.
The aim of our study is to quantify serum chromium and cobalt values and to analyse their temporal evolution over five years after the use of the H MAX-M® modular neck stem (Limacorporate, San Daniele, Italy).
Material and methodsThe investigators adhere to the Oviedo and Helsinki declarations on biomedical research. Our centre's clinical research ethics committee gave its approval (CEIC code 110/17). The patients included in the study gave their written consent for the processing of their data and participation in the study, and for the surgical intervention.
Patient selectionWe present a prospective series of 61 patients undergoing primary total hip arthroplasty by implantation of the H MAX-M® stem (Limacorporate, San Daniele, Italy), in whom serum chromium and cobalt testing was performed at six months, two years, and five years.
The inclusion criteria were patients diagnosed with coxarthrosis (primary, or secondary to avascular necrosis, Perthes disease, hip dysplasia, and epiphysiolysis) implanted with the H MAX-M® modular neck stem from January 2012 to December 2015. Exclusion criteria were any other diagnosis of coxofemoral pathology, presence of osteosynthesis or arthroplasty material, dental implants, heavy metal workers, chronic vitamin B12 intake, dietary supplements, alcoholism, or nephropathy.
Of a total of 638 patients who underwent total hip arthroplasty at our centre, 289 patients were included in the study after applying the inclusion and exclusion criteria. Subsequently, on an annual basis, an orthopaedic surgeon selected the first 18 patients undergoing surgery each year between 2012 and 2015 using a modular neck stem who met the inclusion criteria. The number of patients selected was based on the number of authorised tests, exceeding the pre-calculated minimum sample size. A total of 72 patients were obtained; after accounting for loss due to complications, loss to follow-up, and contralateral surgery, 61 patients completed the study.
It should be noted that in our centre we use the homologous monobloc HMAX-S® stem (Limacorporate, San Daniele, Italy). The decision to implant a stem with a modular neck depended on preoperative planning, intraoperative manoeuvres to check implant stability, soft tissue tension, and limb length, as well as the surgeon's preferences.
Surgical techniqueA four-member surgical team performed the surgical procedure. Two acetabular component designs made of titanium alloy were used, one of hydroxyapatite-coated porous titanium (Delta PF) and the other of trabecular titanium (Delta TT). The femoral head was ceramic, and the insert used was ceramic or polyethylene. The femoral component used was the H-MAX-M® modular neck stem (Limacorporate, San Daniele, Italy) made of Ti6Al4V with a hydroxyapatite coating. The interchangeable necks used in the modular implants are made of a cobalt-chromium-molybdenum alloy and have a 12/14 taper with a double radius cross-section and two lateral grooves or channels. They are available in two lengths, in two neck-diaphysis angles and in three different versions.
Measuring techniqueA 1ml serum sample is taken from each patient and sent in a suitable trace-metal-free polypropylene transport tube to an external laboratory. When received by the external laboratory, the samples were stored in a refrigerator at 4°C. The serum samples were analysed by inductively coupled plasma-mass spectrometry. The limits of quantification of the system are .5μg/l for cobalt and .3μg/l for chromium. All tests were performed in a single external laboratory.
Follow-upThe protocol recommended by the Spanish Society of Hip Surgery (SECCA) was followed in all patients. The SECCA accepts cobalt values of ≤2μg/l and serum chromium ≤5μg/l in patients with unilateral metal-on-metal hip prostheses. Cobalt values between 2μg/l and 10μg/l and chromium values between 5μg/l and 12μg/l are considered risky and complementary explorations should be considered, and cobalt values ≥10μg/l and chromium ≥12μg/l should prompt short-term surgical treatment in the case of surface prosthesis.8 In outpatient consultations, check-ups were performed at six months, and then annually, with radiographic control (anteroposterior pelvis and axial hip) at each visit, and the patient was given a numerical pain classification scale, considering pain to be that present in the groin, thigh or buttock area with or without muscle weakness and limp. Patients with pain ≥4 were considered symptomatic.9 Symptomatic patients underwent CT and MRI scans to look for signs of loosening and pseudotumours.
Statistical analysisThe sample size was based on preliminary results from 2012 on our study population (five patients) indicating that chromium varied with a mean of .34 and a standard deviation of .11 and cobalt with a mean of 3.68 and a standard deviation of .77. Assuming the standard deviation of cobalt, which is the most demanding situation, and accepting an alpha risk of .05 and a beta risk of .20, the minimum required sample size was 47 patients.
Descriptive statistics were calculated for each of the variables. Qualitative variables were described as frequencies and percentages. For quantitative variables, the normality of the distribution was assessed using the Kolmogorov–Smirnov test and the homogeneity of variance test or Levene's test was applied to verify the assumption of equality of variances. In the case of the ions, the values were described by mean and standard deviation, and by median and range to facilitate comparison with the literature. Given the non-normality of the distribution, the Mann–Whitney U test was used for comparison. An assessment over time was made for chromium and for cobalt using simple linear regression. A p-value of <.05 was considered significant.
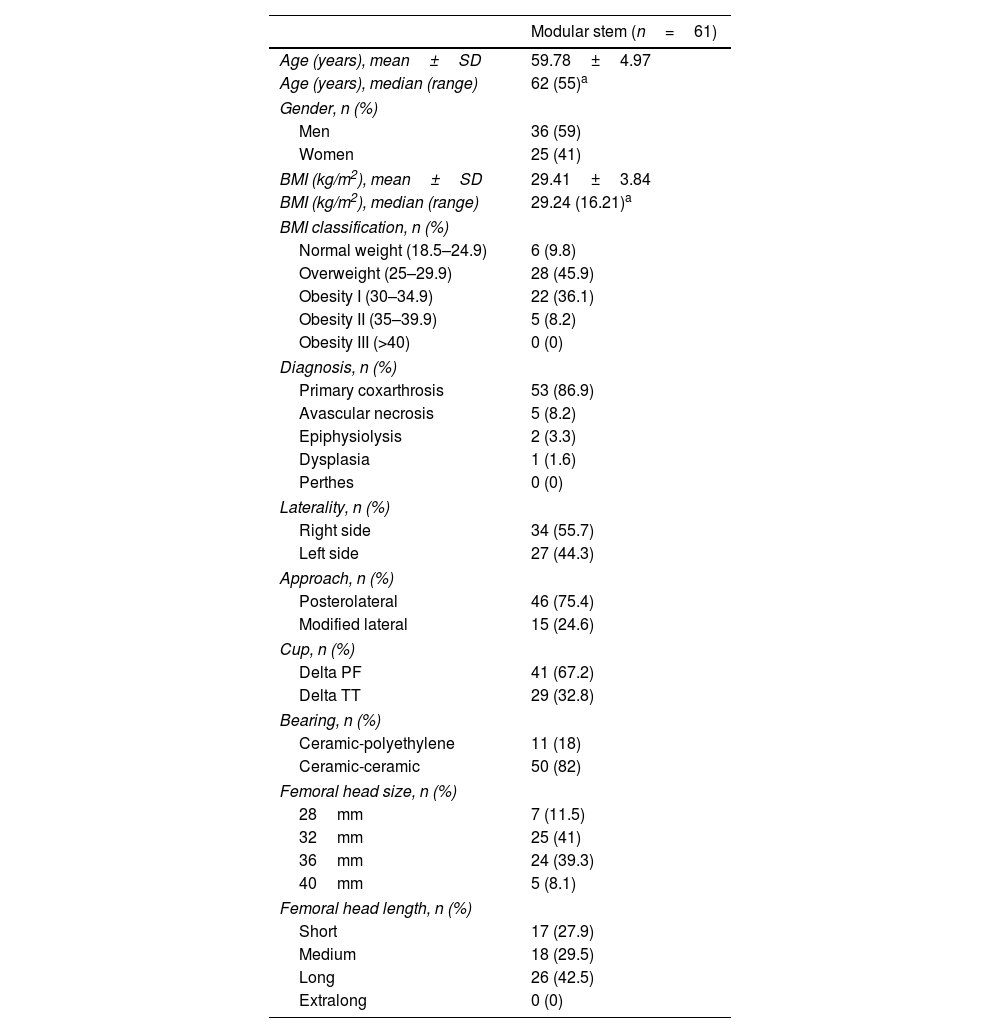
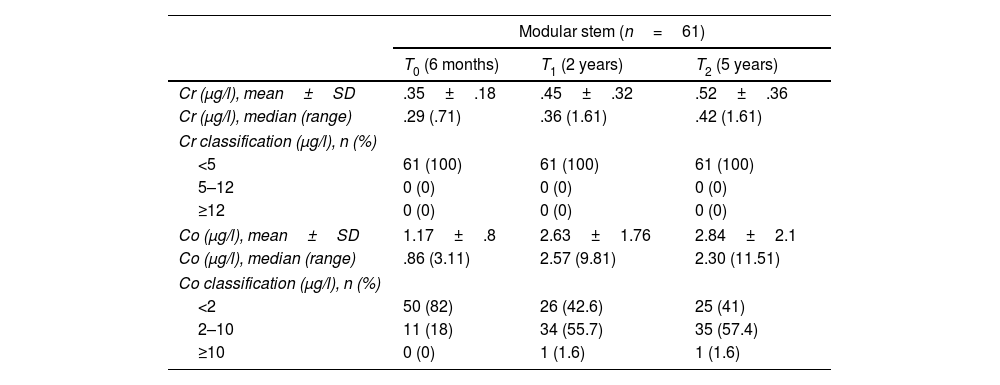
ResultsTable 1 shows the baseline characteristics of our study population. Table 2 shows the serum chromium and cobalt values over the three testing periods.
Baseline characteristics of patients implanted with modular stem.
| Modular stem (n=61) | |
|---|---|
| Age (years), mean±SD | 59.78±4.97 |
| Age (years), median (range) | 62 (55)a |
| Gender, n (%) | |
| Men | 36 (59) |
| Women | 25 (41) |
| BMI (kg/m2), mean±SD | 29.41±3.84 |
| BMI (kg/m2), median (range) | 29.24 (16.21)a |
| BMI classification, n (%) | |
| Normal weight (18.5–24.9) | 6 (9.8) |
| Overweight (25–29.9) | 28 (45.9) |
| Obesity I (30–34.9) | 22 (36.1) |
| Obesity II (35–39.9) | 5 (8.2) |
| Obesity III (>40) | 0 (0) |
| Diagnosis, n (%) | |
| Primary coxarthrosis | 53 (86.9) |
| Avascular necrosis | 5 (8.2) |
| Epiphysiolysis | 2 (3.3) |
| Dysplasia | 1 (1.6) |
| Perthes | 0 (0) |
| Laterality, n (%) | |
| Right side | 34 (55.7) |
| Left side | 27 (44.3) |
| Approach, n (%) | |
| Posterolateral | 46 (75.4) |
| Modified lateral | 15 (24.6) |
| Cup, n (%) | |
| Delta PF | 41 (67.2) |
| Delta TT | 29 (32.8) |
| Bearing, n (%) | |
| Ceramic-polyethylene | 11 (18) |
| Ceramic-ceramic | 50 (82) |
| Femoral head size, n (%) | |
| 28mm | 7 (11.5) |
| 32mm | 25 (41) |
| 36mm | 24 (39.3) |
| 40mm | 5 (8.1) |
| Femoral head length, n (%) | |
| Short | 17 (27.9) |
| Medium | 18 (29.5) |
| Long | 26 (42.5) |
| Extralong | 0 (0) |
BMI: body mass index; SD: standard deviation.
Serum metal ion testing.
| Modular stem (n=61) | |||
|---|---|---|---|
| T0 (6 months) | T1 (2 years) | T2 (5 years) | |
| Cr (μg/l), mean±SD | .35±.18 | .45±.32 | .52±.36 |
| Cr (μg/l), median (range) | .29 (.71) | .36 (1.61) | .42 (1.61) |
| Cr classification (μg/l), n (%) | |||
| <5 | 61 (100) | 61 (100) | 61 (100) |
| 5–12 | 0 (0) | 0 (0) | 0 (0) |
| ≥12 | 0 (0) | 0 (0) | 0 (0) |
| Co (μg/l), mean±SD | 1.17±.8 | 2.63±1.76 | 2.84±2.1 |
| Co (μg/l), median (range) | .86 (3.11) | 2.57 (9.81) | 2.30 (11.51) |
| Co classification (μg/l), n (%) | |||
| <2 | 50 (82) | 26 (42.6) | 25 (41) |
| 2–10 | 11 (18) | 34 (55.7) | 35 (57.4) |
| ≥10 | 0 (0) | 1 (1.6) | 1 (1.6) |
Co: cobalt; Cr: chromium; SD: standard deviation.
All variables show a non-normal distribution in all subgroups.
Fig. 1 shows a tendency for chromium metal ions to rise over time from the first measurement at six months to the third measurement at five years, only the difference between six months and five years being significant (p=.01).
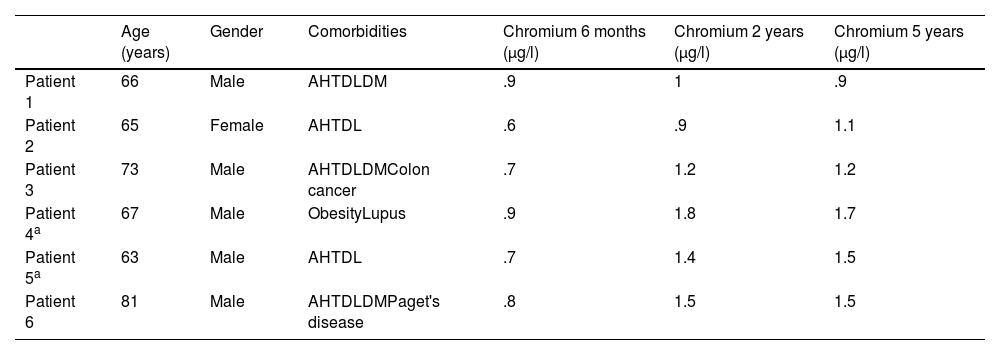
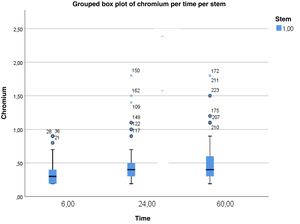
Fig. 2 shows how, at the six-month testing, no patient presented levels higher than 1μg/l. At two years, three patients presented values outside the distribution of the sample studied, known in the field of statistics as outliers. These were values between 1 and 1.5μg/l (patients number 1, 2, and 3) and chromium values higher than 1.5μg/l (patients number 4, 5, and 6), whose data are shown in Table 3. We did not find, therefore, any patient with levels above 2μg/l in any test.
Patients with chromium values outside the distribution of the studied sample.
| Age (years) | Gender | Comorbidities | Chromium 6 months (μg/l) | Chromium 2 years (μg/l) | Chromium 5 years (μg/l) | |
|---|---|---|---|---|---|---|
| Patient 1 | 66 | Male | AHTDLDM | .9 | 1 | .9 |
| Patient 2 | 65 | Female | AHTDL | .6 | .9 | 1.1 |
| Patient 3 | 73 | Male | AHTDLDMColon cancer | .7 | 1.2 | 1.2 |
| Patient 4a | 67 | Male | ObesityLupus | .9 | 1.8 | 1.7 |
| Patient 5a | 63 | Male | AHTDL | .7 | 1.4 | 1.5 |
| Patient 6 | 81 | Male | AHTDLDMPaget's disease | .8 | 1.5 | 1.5 |
AHT: arterial hypertension; DL: dyslipidaemia; DM: diabetes mellitus.
Fig. 3 shows an upward trend in cobalt values from the first measurement at six months to the third measurement at five years, with a slight tendency to stabilise between the values at two years and five years. The mean cobalt at six months was significantly lower than at two and five years (p=.001 for both comparisons), while no statistically significant differences were found between two and five years (p=.415).
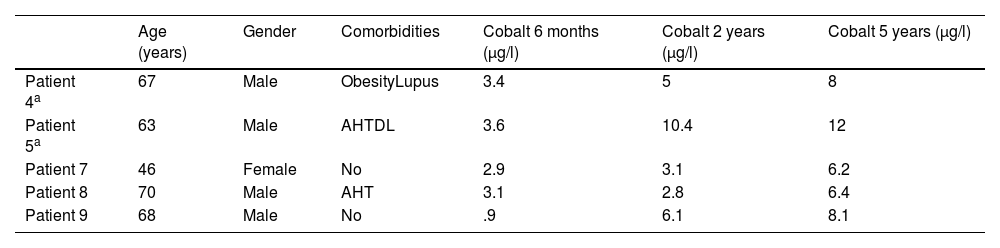
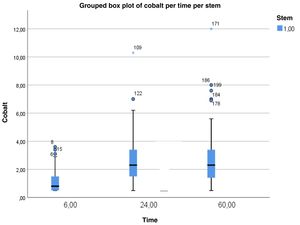
Fig. 4 shows five patients who presented values higher than 2μg/l. Of these, three patients had outliers or values outside the distribution below 4μg/l at six months, which remained in an elevated range (below 8μg/l) at five years (patients number 4, 7, and 8). The other two patients had striking elevation of serum cobalt levels, greater than 8μg/l, at two years (patient number 5), and at five years (patient number 9). The data for these patients are presented in Table 4.
Patients with cobalt values outside the distribution of the studied sample.
| Age (years) | Gender | Comorbidities | Cobalt 6 months (μg/l) | Cobalt 2 years (μg/l) | Cobalt 5 years (μg/l) | |
|---|---|---|---|---|---|---|
| Patient 4a | 67 | Male | ObesityLupus | 3.4 | 5 | 8 |
| Patient 5a | 63 | Male | AHTDL | 3.6 | 10.4 | 12 |
| Patient 7 | 46 | Female | No | 2.9 | 3.1 | 6.2 |
| Patient 8 | 70 | Male | AHT | 3.1 | 2.8 | 6.4 |
| Patient 9 | 68 | Male | No | .9 | 6.1 | 8.1 |
AHT: arterial hypertension; DL: dyslipidaemia; DM: diabetes mellitus.
It should be noted that all the patients with elevated ion values were asymptomatic and without radiographic abnormalities at the time of writing this paper and continue to be monitored by the traumatology and orthopaedic surgery department.
DiscussionThanks to the development of metallurgy, orthopaedic implants are highly resistant to surface corrosion phenomena due to exposure to an aqueous environment. At socket level, multifactorial corrosion has been described involving galvanic corrosion when different metals are in contact, crevice corrosion, and mechanically assisted crevice corrosion. Mechanically assisted crevice corrosion, specifically facilitated by the micromotions occurring between the assembled parts, has been found to be the main corrosion mechanism at these modular interfaces.2,10 The emergence of implants with a second socket at the level of the stem-neck, the modular neck stems, has increased concern about these phenomena.11
Corrosion at the level of the socket, also known as trunnionosis, is the source of metal waste products in the form of ions that can either remain soluble or react with organic anions, such as phosphate, to create insoluble precipitates.3,10 Cr3+, released in greater proportion than Cr6+, can form insoluble precipitates in the socket zone11 or remain in the extracellular medium as an unstable product unable to cross the cell membrane, binding to the serum protein transferrin and, to a lesser extent, to albumin.12 For its part, Co2+ can enter cells through membrane receptors such as calcium pumps, or it can remain in the extracellular compartment, where it binds to albumin and, to a lesser extent, remains a free ionic product.13
In our study, we assessed the evolution of chromium and cobalt ions in the serum of patients with modular neck stems and ceramic-ceramic or ceramic-polyethylene bearings. We used one particular stem, the HMAX-M® design (Limacorporate, San Daniele, Italy), which has a negative socket angle with an initial contact and locking in the distal area.14 In addition, the 12/14 taper used in this design is one of the tapers with the lowest corrosion described.15 The most important feature of this stem model is the asymmetric double-radius design with two lateral grooves in the taper cross-section, which in in vitro studies provides higher mechanical strength and reduces corrosion phenomena compared to other symmetric taper designs. However, the in vivo translation of these properties could not be confirmed in our study, since, as we have already explained, in patients implanted with HMAX-M® stems (Limacorporate, San Daniele, Italy), cobalt levels in the blood are found to be initially elevated and then tend to stabilise.
There are no studies that analyse serum metal ion levels in patients with the HMAX-M® modular neck stem, although we did find results for other prostheses with modular neck stems and ceramic-ceramic bearings. In this regard, Somers et al.16 based their study on the Profemur Xm modular neck stem model (MicroPort Orthopedics Inc., Wright Medical) with a CoCrMo neck and obtained median serum cobalt values of 1.71μg/l (range .49–3.70μg/l) and chromium values of .49μg/l (range .49–6.2μg/l) at eighteen months of mean follow-up. Our study presents higher values than those reported by Somers et al.16 Laurençon et al.17 analysed the SPS modular neck stem (Symbios INC, Yverdon-les-Bains, Switzerland), observing chromium values of 1.12±.52μg/l and cobalt levels of 1.54±2.80μg/l, with lower cobalt levels than in our study.
It is very important to note that we found no studies that perform an evolutionary analysis of ion levels in patients implanted with a modular neck stem. Results have only been presented on arthroplasty with a monobloc stem and metal-on-metal bearing that includes release from the bearing surfaces and head-neck socket, and therefore the results are not comparable to ours. Nevertheless, we present possible trends observed with these implants as they relate to human ion metabolism.
Some authors report a progressive increase in chromium values.18–20 Our result on serum chromium is in line with that published by these authors. One justification for this result can be found in the persistence of micromotion at the level of the socket, which produces a constant release of chromium anions that form insoluble precipitates in this area11 or remain in the extracellular medium.12 Numerous authors have observed an initial increase and subsequent stabilisation.18,21,22 We observed this same trend in cobalt values, and one reason for this finding could be, as with chromium, the metabolism of cobalt, given that it achieves a rapid intra-extracellular equilibrium and renal elimination is accelerated when values increase.23 The study by DeSouza et al.24 is worth mentioning, they observed a second peak of elevation between five and ten years.
It should be borne in mind that the medical literature includes different prosthetic models, bearings, and samples that are tested, and therefore the comparison may not be entirely correct, as mentioned above. Even so, the importance of serial testing to evaluate a trend in the values is evident, and it is this trend that will allow comparisons, even if different samples and different implants have been tested. Isolated metal ion values have poor sensitivity, specificity, and predictive values.25
The increase in cobalt, together with the growing number of publications on failures in other models and the lack of difference in radiographic corrections with respect to its monobloc counterpart,26,27 has led to a decrease in the use of stems with modular necks in our centre. However, we consider implants that allow precise intraoperative adjustments an interesting possibility and, therefore, it is not unreasonable to believe that there may be a breakthrough in these designs in the future that avoid the potential risks from corrosion phenomena.
As limitations of our study, we believe it would be of interest to increase the follow-up time to assess whether chromium levels continue to rise, stabilise, or whether there is a further upturn in cobalt values, as described by DeSouza et al.24 The information provided by this author and the trend observed in our result prompted us to keep our study series open for a further measurement of metal ions at ten years. Similarly, the small sample size prevents us from analysing individually the different neck options and size or length of head. On the other hand, the lack of a comprehensive analysis of clinical–functional outcomes in terms of serum ion levels may limit the generalisability of our results.
ConclusionIn our study we observed a progressive elevation of serum chromium levels and an elevation and subsequent stabilisation of serum cobalt levels in patients implanted with a modular neck stem. The results obtained in this study have limited the use of modular neck stems in our routine practice.
Level of evidenceLevel of evidence iii.
FundingNo funding was received for this work.
Conflict of interestsThe authors have no conflict of interests to declare.