Osteoarthritis is a disabling pathology characterised by joint pain and stiffness. A prevalence of coxarthrosis of 7.4% is reported in our country. Total hip joint replacement is indicated in advanced stages, a procedure that is not free of complications, the most frequent being prosthetic dislocation, which can be prevented with dual mobility systems. The following study aims to determine the rate of complications and clinical outcomes in dual mobility systems in primary coxarthrosis.
Materials and methodsA retrospective study included 120 cases in 114 patients diagnosed with grade III coxarthrosis, mean age was 62.43 years, with a mean follow-up of 4.5 years. Joint replacement was performed by Hardinge approach. All cases were assessed clinically using the Harris Hip Score (HHS) and radiologically to demonstrate mid-term results.
ResultsThe preoperative value on the HHS scale had a mean of 56.45, postoperative at one month 74.23; 6 months 85.40; 1 year 94.01 and at 5 years 94.84 points, representing a functional improvement of 17.78 postoperative month; 28.95 at 6 months postoperative; 37.56 at one year postoperative and 38.39 points at 5 years postoperative. A complication rate of 3.44%; 0.86% of complications were associated with the prosthetic components.
ConclusionThe dual mobility system should be considered as a therapeutic option in primary hip joint replacement due to excellent functional results and low complication rates.
Evidence levelIV. Retrospective observational case series study.
Introducción La osteoartritis es una patología incapacitante caracterizada por dolor y rigidez articular. En nuestro país se reporta una prevalencia de coxartrosis del 7,4%. El reemplazo articular total de cadera está indicado en etapas avanzadas, procedimiento que no está exento de complicaciones, la más frecuente es la luxación protésica, que puede ser prevenida con sistemas de doble movilidad (DM). El siguiente estudio tiene como objetivo determinar la tasa de complicaciones y los resultados clínicos en los sistemas de DM en coxartrosis primaria.
Materiales y métodosEstudio retrospectivo donde se incluyeron 120 casos en 114 pacientes con diagnóstico de coxartrosis grado III, la media de edad fue de 62,43 años, con seguimiento medio de 4,5 años. El reemplazo articular se realizó mediante abordaje de Hardinge. Todos los casos fueron valorados clínicamente mediante la escala de Harris Hip Score (HHS) y radiológicamente para demostrar los resultados a mediano plazo.
ResultadosEl valor preoperatorio en la escala HHS tuvo una media de 56,45, posquirúrgica al mes 74,23; seis meses de 85,40; un año de 94,01 y a los cinco años de 94,84 puntos, representando una mejoría funcional de 17,78 mes posquirúrgico; 28,95 a los seis meses posquirúrgicos; 37,56 al año posquirúrgico y 38,39 puntos a los cinco años posquirúrgicos. Una tasa de complicaciones de 3,44%; 0,86% de las complicaciones se asociaron a los componentes protésicos.
ConclusiónEl sistema de DM debe ser considerado como una opción terapéutica en reemplazo articular primario de cadera debido a los resultados funcionales excelentes y bajas tasas de complicaciones.
Nivel de evidenciaIV. Estudio observacional retrospectivo tipo serie de casos.
Coxarthrosis is a disabling condition. The highest prevalence is reported in Europe (12.59%), while in Ecuador it is 7.4%.1–3 Total joint replacement is the definitive treatment in advanced stages of the condition, which is a procedure not free of complications such as prosthetic dislocations or periprosthetic fractures.4
Dislocation in primary total hip arthroplasty, one of the most frequent complications, has an incidence of 2–10%.5
Patient-dependent risk factors associated with prosthetic dislocation are described as follows: age>70 years, low income, white ethnicity compared to Asians, drug users, body mass index≥30kg/m2, neurological disorders, psychiatric diseases, previous surgeries including spinal fusion and previous hip interventions, avascular necrosis of the femoral head, rheumatoid arthritis, inflammatory arthritis, and osteonecrosis, and factors associated with surgery such as posterior approach without capsular repair or short external rotator repair, lack of abductor muscle tension, small diameter femoral heads, thin polyethylene liner, single mobility cups, non-cemented fixations, non-standard femoral neck length, low surgeon experience, and low volume of surgeries.5
For this reason, the dual mobility (DM) prosthesis was developed in France in 1974 by Gilles Bousquet, on the dual principle of a small articulation to minimise wear problems, coupled with a large articulation to stabilise the hip and prevent instability. There are two distinct articulations: a small articulation between the head and the polyethylene shell, and a large articulation between the polyethylene head and the acetabular shell. Most of the movement occurs at the small articulation. Movement of the large articulation only occurs when the neck of the stem comes into contact with the polyethylene head6 (Fig. 1).
Diagram of dual mobility component.6
The main advantage of DM systems is the reduced risk of dislocation. Other advantages are reported such as less impingement, low friction, low wear, and increased ranges of motion. However, a unique disadvantage is intra-prosthetic dislocation requiring surgical re-intervention. Other reported disadvantages include the absence of acetabular fixation screws and wear of the polyethylene liner.7,8
The following is a retrospective observational case series study of patients diagnosed with primary coxarthrosis treated with total hip arthroplasty with second-generation DM system in primary surgery, assessing functional outcomes and complications with a medium-term follow-up. The aim of the study was to demonstrate that the second-generation DM system as a treatment for primary coxarthrosis is a valid therapeutic option with excellent functional results and low complication rates in the medium term.
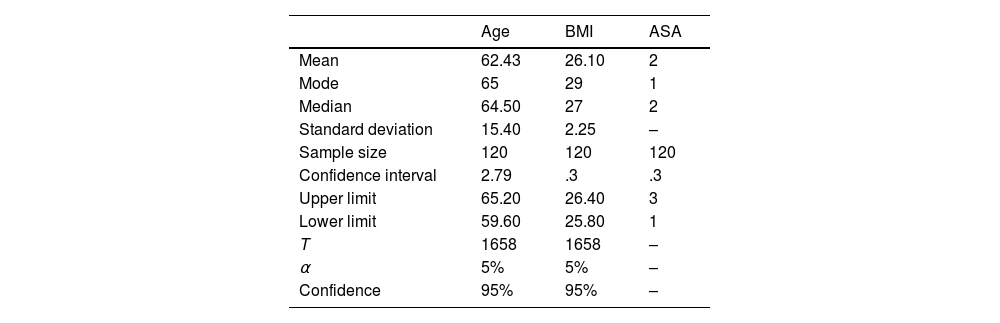
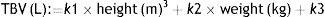
Material and methodsA retrospective observational case series study was conducted with patients diagnosed with primary coxarthrosis Tönnis9 type 3 treated by total hip arthroplasty with second-generation DM system. We included 114 patients representing a sample of 120 cases from January 2015 to January 2023 in Quito, Ecuador, where 45% of the patients were male and 55% female, with a mean sample age of 62.43 years (σ=15.4, CI 59.64; 65.2). The patients had a body mass index of 26.10 (σ=2.25 CI 25.80; 26.40). When comparing variables, we found that with a probability of 95%, the older the patient, the higher their body mass index tends to be. This data is also related to the patient's anaesthesia risk which was measured based on the ASA (American Society of Anaesthesiologists) scale, where the average was ASA 2, which correlates with the age of the patients and their body mass index (BMI), the total sample was found to range between ASA 1 and ASA 3. The follow-up was eight years with an average of 4.5 years (Table 1).
Summary of descriptive statistics for data acquisition.
| Age | BMI | ASA | |
|---|---|---|---|
| Mean | 62.43 | 26.10 | 2 |
| Mode | 65 | 29 | 1 |
| Median | 64.50 | 27 | 2 |
| Standard deviation | 15.40 | 2.25 | – |
| Sample size | 120 | 120 | 120 |
| Confidence interval | 2.79 | .3 | .3 |
| Upper limit | 65.20 | 26.40 | 3 |
| Lower limit | 59.60 | 25.80 | 1 |
| T | 1658 | 1658 | – |
| α | 5% | 5% | – |
| Confidence | 95% | 95% | – |
Exclusion factors were patients with a diagnosis of secondary coxarthrosis, patients with coxarthrosis Tönnis grade<3, patients younger than 18 years, patients with a follow-up of less than six months, and patients without sequential clinical or radiological controls.
Preoperative anteroposterior pelvis and axial hip radiographs were ordered for all patients. All procedures were performed with the same surgical technique, using the Hardinge lateral hip approach.10
The Dualis™ system (Gruppo Bioimpianti SRL, Milan, Italy) was used in 88% of the patients and the Quattro™ system (Groupe Lépine, Genay, France) in 12%. At the femoral level, the Korus™ stem (Gruppo Bioimpianti SRL, Milan, Italy) was used in 92% of the patients (95% cementless) and the cementless Taperloc® (Zimmer-Biomet, Warsaw, Indiana, USA) in the remaining 8%.
Two types of second-generation DM prostheses are currently available in our setting. The first is the Quattro™ system, where the acetabular cup has hydroxyapatite coating and spikes in its dome in order to provide better grip and immediate fixation in the host bone.
The second is the Dualis™ system which has a plasma spray coating and a 1mm peripheral flange to improve grip and fixation to the host bone.
The acetabular cup of the Dualis™ has a has a groove, designed to be placed distal and anterior to the acetabulum, in order to increase the range of hip adduction and decrease compression with the psoas iliacus anteriorly.
Both systems allow 28mm head placement. However, there are differences in the polyethylene (PE) of the two systems. The PE of the Quattro™ prosthesis has greater coverage of the femoral head compared to that of the Dualis™ implant (Fig. 2).
The Dualis™ system, due to the characteristic mentioned above, allows a greater range of motion and lower probability of contact with the femoral neck in both adduction and abduction (Fig. 3).
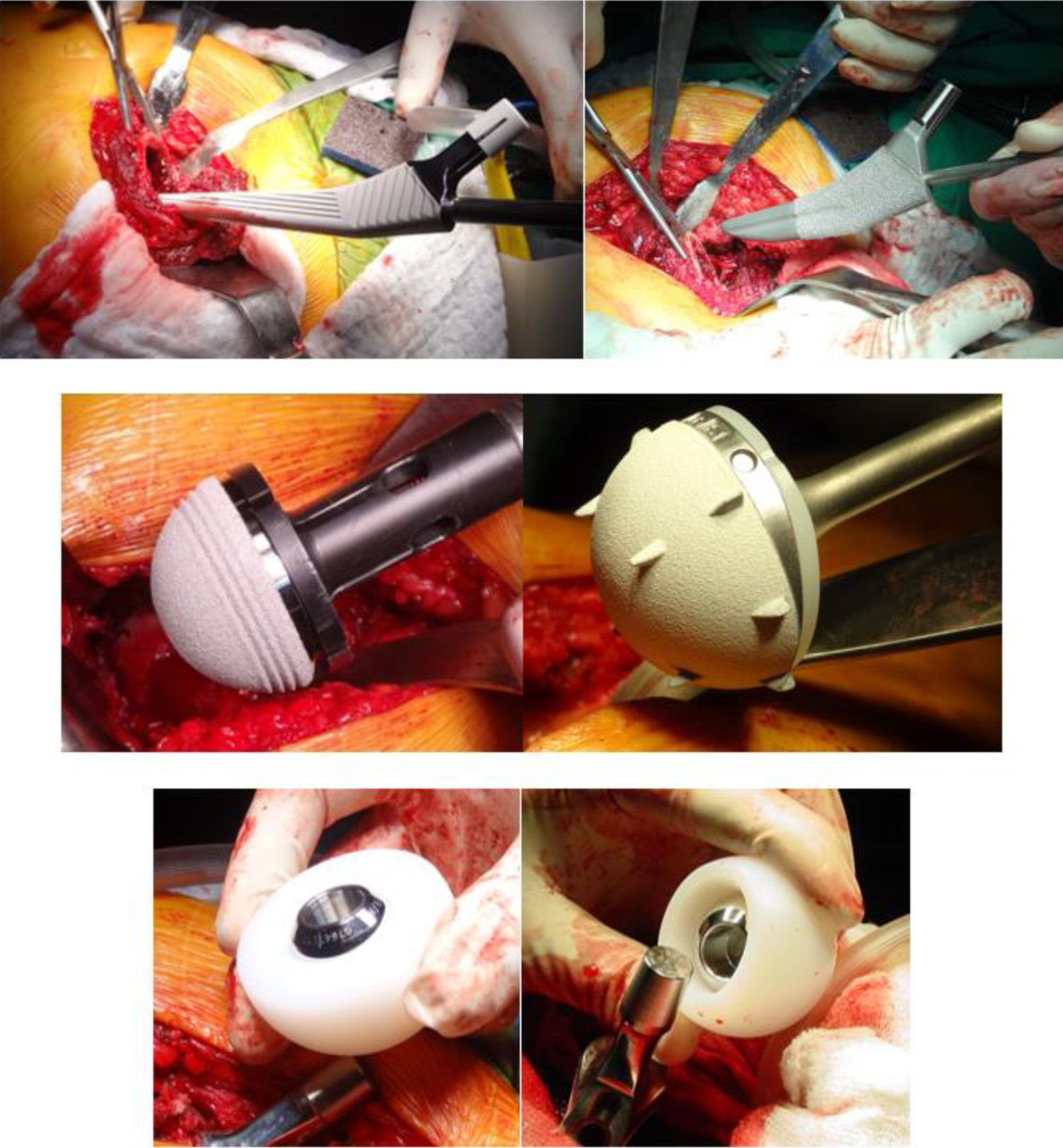
The patient is positioned in lateral decubitus on hip positioners, with asepsis and antisepsis using 2% chlorhexidine soap and iodised alcohol. The lateral Hardinge10 approach was deployed. Controlled hip dislocation, cervical osteotomy depending on the type of stem to be inserted. The femur and acetabulum are prepared with the corresponding rasps. The definitive components are then placed, and the prosthetic components are reduced (Fig. 4).
Finally, adequate stability of the prosthetic components and length of the limbs are checked, and the wound is closed in layers. Hospital stay was a minimum of two days and a maximum of five days. Early walking with full weight-bearing and a four-point walker was started five hours after surgery and three times a day during the hospital stay. All patients received thromboprophylaxis for 30 days and antibiotic therapy with first generation cephalosporins for three doses.11,12
Postoperative follow-up was at two weeks to remove stitches or staples. Clinical and radiographic controls were performed at one month, three months, six months, 12 months, and then every year.
The study was conducted in accordance with the ethical standards recognised by the declaration of Helsinki and resolution 008430 of 1993, and was approved by the institution's ethics committee, and the patients who participated in the study gave their informed consent.
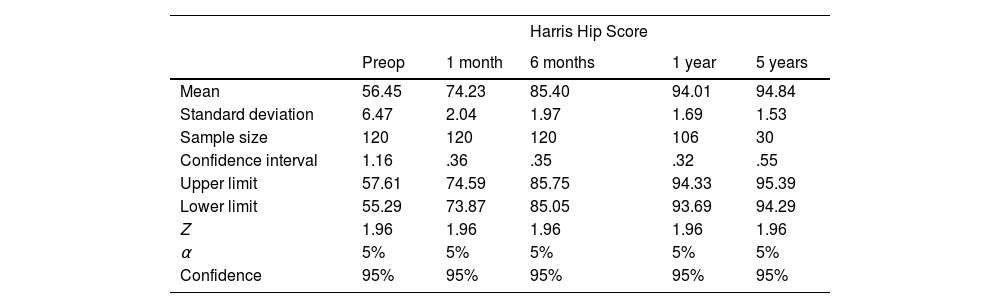
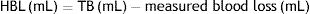
ResultsThe Harris Hip Score (HSS) (pain, limp, support, walking distance, sitting comfortably, using public transport, managing stairs, putting on shoes and socks, deformity, and range of motion) was used for functional assessment.13 The mean preoperative HHS was 56.45 points (σ=6.47, CI 55.29; 57.61), at one month postoperatively it was a mean of 74.23 (σ=2.04, CI 73.87; 74.59); 85.40 at six months (σ=1.97.47, CI 85.05; 85.75); 94.01 at one year (σ=1.69, CI 93.69; 94.33), and 94.84 at five years (σ=1.53, CI 94.29; 95.39). It is important to emphasise the time variability in follow-up, as not all individuals in the sample underwent surgery on the same timeline (Table 2).
Summary of descriptive statistics for data collection.
| Harris Hip Score | |||||
|---|---|---|---|---|---|
| Preop | 1 month | 6 months | 1 year | 5 years | |
| Mean | 56.45 | 74.23 | 85.40 | 94.01 | 94.84 |
| Standard deviation | 6.47 | 2.04 | 1.97 | 1.69 | 1.53 |
| Sample size | 120 | 120 | 120 | 106 | 30 |
| Confidence interval | 1.16 | .36 | .35 | .32 | .55 |
| Upper limit | 57.61 | 74.59 | 85.75 | 94.33 | 95.39 |
| Lower limit | 55.29 | 73.87 | 85.05 | 93.69 | 94.29 |
| Z | 1.96 | 1.96 | 1.96 | 1.96 | 1.96 |
| α | 5% | 5% | 5% | 5% | 5% |
| Confidence | 95% | 95% | 95% | 95% | 95% |
The imaging assessment was based on radiographs in two projections: anteroposterior of the pelvis and axial of the operated hip. Posterosuperior dislocation of the prosthesis was evident in .83% of the images, in the rest of the sample there was no evidence of acetabular loosening in the De Lee and Charnley areas, nor stem loosening in the Gruen areas, nor loss of congruence of the prosthetic components.
For the statistical analysis, the database was sorted, and descriptive statistics were initially performed to obtain measures of central tendency and central dispersion, which were compared with other studies of similar characteristics. Similarly, variables were crossed with parametric tests, which allowed Pearson's coefficients to be obtained to validate data correlation. Finally, to predict survival of the arthroscopy, a linear regression with elimination of statistical noise was performed, obtaining the result in years of implant survival, which in turn was compared with other studies with similar characteristics to validate the results.
Complications were reported in four cases out of the total sample, representing 3.32%. One case of intraprosthetic dislocation (.83%) occurred at four weeks postoperatively, resolved with revision of mobile components, one case of loosening of the acetabular component (.83%) at two weeks postoperatively due to poor bone quality, resolved with acetabular cup cementation. The other two cases reported were associated with causes unrelated to the prosthetic components; one case of crural nerve injury managed with neuromodulatory medication with complete recovery at five months, and another case of superficial infection of the surgical site managed with antibiotic therapy and dressings until it resolved completely.
The results obtained can be used to cross-reference different variables using simple linear regression models and two-sample t-test analysis under the assumption of different variances, which were obtained from studies of similar characteristics, to test or reject the hypothesis.
Data analysis was performed with linear regression, to contrast the data with studies of similar characteristics and then perform the appropriate extrapolation of data.
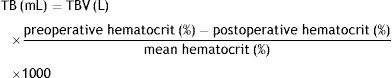
The linear equation below was obtained through a linear regression analysis with exponential smoothing between age and pre-operative HHS functional assessment:
where the independent variable Y is age and the dependent variable X is the loss or gain of mobility, prior to surgery it can be seen that there is an established relationship between the two, i.e., older adult patients who debut with difficulty of mobility and pain and have not undergone surgery, will worsen over time in an increasing ratio.Having undergone surgical resolution, with the technique described in this article, an improvement in the HHS can be inferred during the first postoperative year.
A very marked recovery of the patients can be observed at five years, and therefore an improvement in their quality of life according to the HHS.
On cross-referencing variables between the type of prosthesis used and recovery, a Pearson correlation coefficient of −.03 was found, which means that we can infer that the type of instruments used will reduce the patient's recovery time, allowing them to return to their daily life in less time.
On running a multivariate regression taking into account age, body mass index, comorbidities, the type of prosthesis used, and recovery over five years, with previous cross-checking of variables with T-sample analysis, we found that:
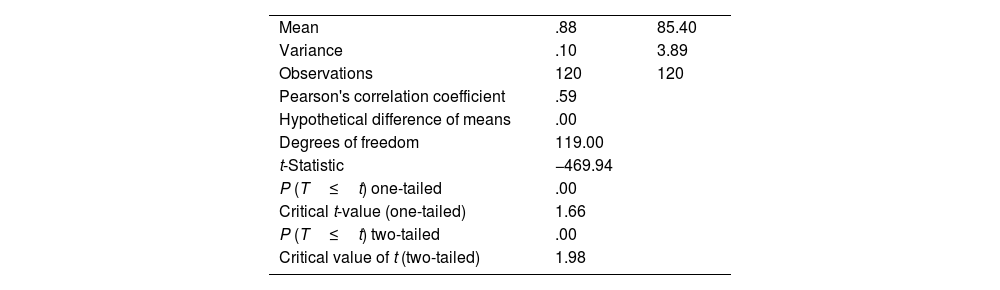
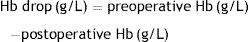
where it can be inferred that middle-aged patients with a body mass index within acceptable values, ASA between I and III, and the type of prosthesis used in this study, show better recovery over five years, reaching normality in 95% of the patients.With regard to the type of prosthesis used over five years the patients’ quality of life had improved, by combining the type of prosthesis used and recovery on the HHS, a Pearson correlation coefficient of .59 can be observed, which means we can infer that the type of prosthesis used contributes to patient recovery and is linked to having deployed an appropriate technique within the study sample. It would be advisable to compare with other techniques and extrapolate the data to statistical significance (Table 3).
Summary of paired two-variable t-test, prosthesis type versus functional scale.
| Mean | .88 | 85.40 |
| Variance | .10 | 3.89 |
| Observations | 120 | 120 |
| Pearson's correlation coefficient | .59 | |
| Hypothetical difference of means | .00 | |
| Degrees of freedom | 119.00 | |
| t-Statistic | −469.94 | |
| P (T≤t) one-tailed | .00 | |
| Critical t-value (one-tailed) | 1.66 | |
| P (T≤t) two-tailed | .00 | |
| Critical value of t (two-tailed) | 1.98 |
The total hip replacement procedure has been deployed very considerably over time, with younger and more active patients undergoing this type of procedure, making it a real challenge for the orthopaedic surgeon, for whom there can be complications such as early loosening, dislocations, periprosthetic fractures, or instability.
Puch et al.,14 in their 2016 study conducted in 119 patients under 55 years of age and 444 patients over 55 years of age, who underwent total hip arthroplasty using the DM system, with an average follow-up of 11 years (eight to 15 years), where no difference was found with respect to the rate of loosening or implant failure. No dislocation events were described in their study, and the implant survival rate was 99% at 14.2 years, thus demonstrating that total arthroplasty with the DM cup in young patients, is a relevant surgical option.
Assi et al.,15 in their 2017 study, describe a total of 84 hips operated on in 74 patients (10 bilateral), with a Harris score of 97.1±7, without finding a significant difference between primary interventions or revisions, and highlighting that religious patients (65% of patients in the study, Muslim) were able to return to the prayer position in an average of three months.
Gaillard et al.,16 in their 2019 study, in a cohort of 310 patients, presented very encouraging results, with an implant survival of 98% at 10 years, no signs of loosening or osteolysis, no prosthetic dislocation or intraprosthetic dislocation, and no infections, the only complication was periprosthetic fracture of the stem in three cases in total.
A study conducted in 2019 by Sappey et al., which included 126 patients, 53 with standard cup and 73 with DM, reported that dislocation was 12 times more frequent in the former group, while periprosthetic fractures were the reverse, concluding that DM components increase stability and the risk of periprosthetic fractures.17
The combination of second-generation materials such as high molecular weight, highly cross-linked polyethylene with DM cups has a good satisfaction rate. This is described by Epinette et al.18 in their study of 321 patients undergoing total arthroplasty with DM cup with high molecular weight, highly cross-linked polyethylene components, where no events of prosthetic dislocation or intra-prosthetic dislocation were reported. One of the patients in the study died of causes unrelated to the prosthetic replacement. The patients were assessed with a Harris score of 93.60±8.48, all acetabular components remained firm on X-ray studies, except for two cases that had to be revised due to malpositioning.
A systematic review published in 2023, which included 39 case series (10,494 patients) and 14 national registry series (23,020 patients), reports a survival of 99.7% at five years, 95.7% at 10 years, 96.1% at 15 years, and 77% at 20 years in the case series, while national registries show a survival of 97.8% at five years and 96.3% at 10 years, with dislocation rates of 1.1%, instability .8%, infection .4%, and fracture .3%, concluding that this type of prosthesis has an acceptable survival with low complication rates.19
A systematic review conducted in 2023 on 738 young patients (average age 46.9 years) reports dislocation in 15 hips representing 2.5%, concluding that using the DM system suggests favourable results with respect to stability.20
Total hip arthroplasty with the DM system in primary surgery has been shown to be a technique with good functional results in the short and medium term with dislocation rates of less than 1%.
The results obtained in this study are similar to those reported in the literature. We recommend limiting the use of the second-generation DM system in dysplastic acetabula or those with bony defects, because fixation in the native bone may be compromised as acetabular screw placement is not possible. We suggest that the system be considered in patients with high mobility demands to reap the benefits of its design and reduce complications.
Limitations of the studyThe main limitation of the study was the sample size, due to the number of patients coming from a single specialist physician. This influences the external validity of the study, which can be inferred by the mathematical projection processes and parametric models used that present statistical noise, which were run with exponential smoothing. Another limitation is the possibility of Hawthorne effect in some patients, only one functional scale was used for functional assessment, and finally, there is the possibility of recall bias in other patients.
ConclusionsTotal hip arthroplasty with the DM system is a procedure that shows an average functional improvement in HHS of 38.39 points at five years post-surgery. Complications were reported in 3.32%, .86% of the complications were prosthetic component dependent.
With the results demonstrated in the world literature and in this study, the use of DM systems in primary joint replacement is justified and should not be limited to revision cases or patients at increased risk of instability.
Level of evidenceLevel of evidence iv.
FundingThe authors received no funding or grant to undertake this study.
Conflict of interestsThe authors have no conflict of interests to declare.