We estimated the health resource utilisation (HRU) and associated costs during the 12months after a first osteoporotic hip fracture in Spain per Autonomous Regions (OHF) in six Spanish Regions.
MethodsObservational, prospective study including patients ≥65years-old hospitalised due to a first OHF in: Andalusia, Catalonia, Valencian Community, Galicia, Madrid and the Basque Country. HRU related to OHF, quality of life and patient autonomy were collected, and HRU-associated costs were estimated.
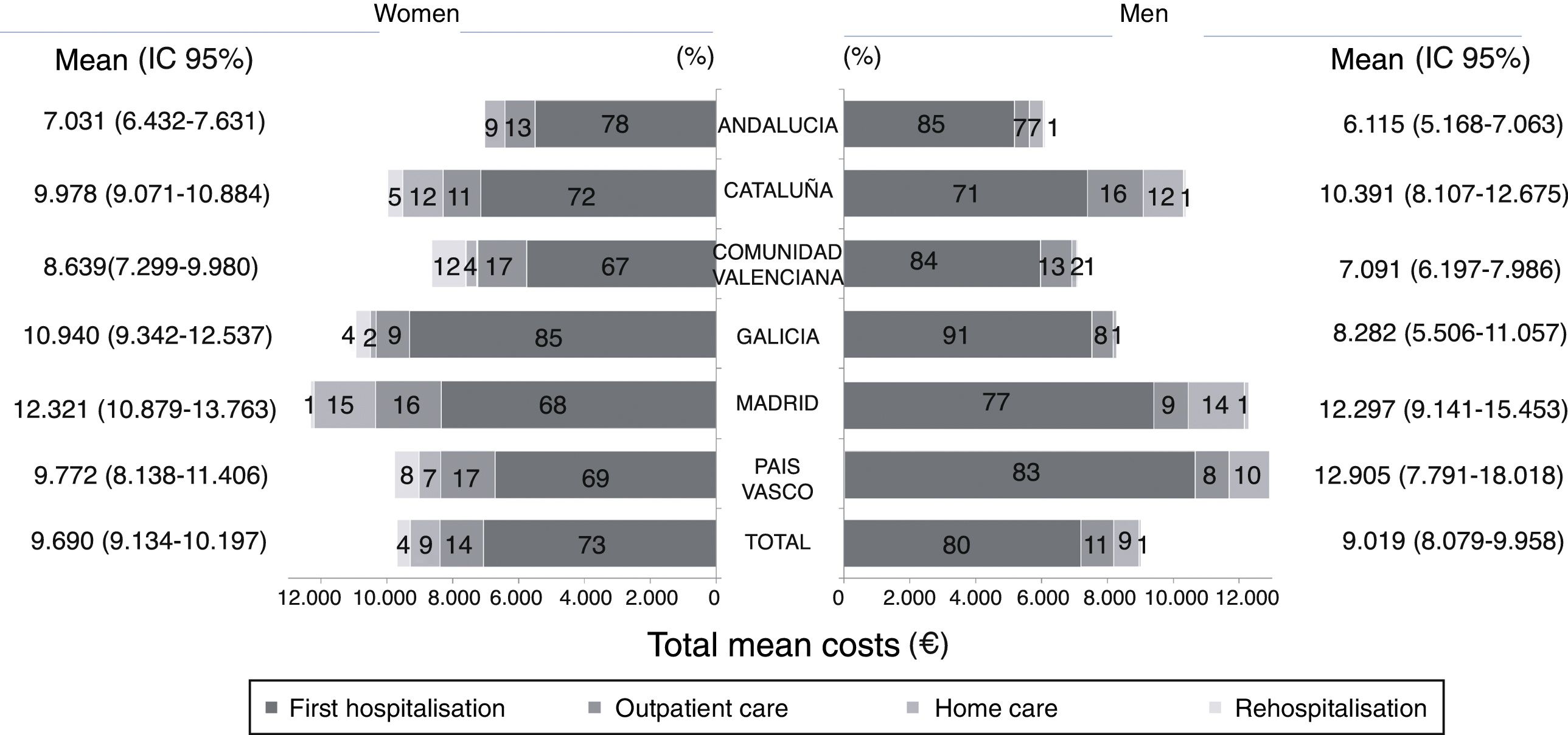
ResultsFour hundred and eighty-seven patients (mean age: 83.1years, 77% women) were included, with demographic characteristics that were similar across the Regions. Mean hospital stay was longest in Madrid and Galicia (women/men: 15.0/18.6 and 16.9/12.6days, respectively) and shortest in Andalusia and the Valencian Community (8.2/7.2 and 8.4/9.4days). There were more rehabilitation sessions and formal home care days in Catalonia and Madrid (women/men: 16/21 and 17/29 sessions; 19/20 and 30/27days) and fewer in Andalusia and Galicia (4/1 and 3/0 sessions; 3/1 and 1/0days). Mean HRU costs were higher in Madrid and lower in Andalusia (women/men: 12.321€/12,297€ and 7031€/6115€, respectively).
ConclusionsOHF place a large burden on Spanish Regional Health Systems, including high economic costs. We found notable differences in mean costs across the Regions, mainly caused by the differential length of the first hospital stay and the outpatient care in subsequent months. These differences may be associated with differences in surgical delay. A national consensus on the management of OHF is desirable; moreover, agreeing common guidelines could have major socio-economic and healthcare benefits.
Se estimó la utilización de recursos sanitarios (URS) y costes asociados durante los 12meses posteriores a una primera fractura de cadera osteoporótica (FCO) por comunidad autónoma (CC.AA.).
MétodosEstudio observacional, prospectivo, que incluyó pacientes ≥65años hospitalizados por una primera FCO en Andalucía, Cataluña, Comunidad Valenciana, Galicia, Madrid y País Vasco. Se registró la URS relacionada con la FCO, la calidad de vida y la autonomía del paciente, y se estimaron los costes asociados.
ResultadosParticiparon 487 pacientes (edad media: 83,1años, 77% mujeres), con características demográficas similares entre CC.AA. La duración media del ingreso fue más prolongada en Madrid y en Galicia (mujeres/hombres: 15,0/18,6 y 16,9/12,6 días) y menor en Andalucía y en la Comunidad Valenciana (8,2/7,2 y 8,4/9,4días). Las sesiones de rehabilitación y días de asistencia domiciliaria formal fueron más numerosos en Cataluña y en Madrid (mujeres/hombres: 16/21 y 17/29 sesiones; 19/20 y 30/27días) comparado con Andalucía y Galicia (4/1 y 3/0 sesiones; 3/1 y 1/0días). Los costes medios fueron más altos en Madrid y menores en Andalucía (mujeres/hombres: 12.321/12.297€ y 7.031/6.115€, respectivamente).
ConclusionesLas FCO implican un coste elevado para los sistemas sanitarios autonómicos, observándose diferencias notables entre CC.AA., derivadas principalmente de la duración diferencial de la primera estancia hospitalaria, así como al cuidado ambulatorio durante los meses posteriores. Estas diferencias podrían estar relacionadas con diferencias en la demora quirúrgica. Es deseable un abordaje y consenso a nivel nacional de este problema sanitario, con pautas de actuación comunes, ya que podría suponer grandes beneficios socioeconómicos y sanitarios globales.
Osteoporosis is a chronic skeletal disorder that causes increased bone fragility and fracture risk.1,2 As the population ages an increasingly higher proportion is vulnerable to low-impact trauma fractures, with significant consequences on their health, health-related quality of life (HRQoL), and the social burden.2,3 However, this burden is systematically undervalued, since it is usually considered simply to be the time that a patient is hospitalised.
Approximately 36,000 hip fractures occur in Spain each year in patients aged ≥65 years (90.5% of all hip fractures).4 Few studies have been undertaken to date on the cost and social and economic burden of hip fractures in European countries.5–8
The observational, prospective PROA (PRospective Observational study on burden of hip frActures in Spain) has recently been published, with national data on the costs of a first osteoporotic hip fracture in Spain per Autonomous Regions in subjects aged ≥65 years.9 In light of the differential administration of the health system by the regional health services of each of Spain's autonomous regions, and the need for a reliable and up-to-date estimate of the costs of osteoporotic fractures regionally for healthcare decision-making, we present the results of the PROA study in each of the six participating autonomous regions (Andalusia, Catalonia, Valencian Community, Galicia, Madrid and the Basque Country).
The study objectives were to estimate health resource utilisation (HRU) and direct costs during the 12 months after a first osteoporotic hip fracture in Spain per Autonomous Regions, and to describe the patients’ demographic and clinical features.
Material and methodThe PROA was a prospective, observational, multi-centre and national study over 12 months. The methodology used is described in depth in the published paper by Caeiro et al.9
Twenty-eight hospitals of six of Spain's autonomous regions participated in the study (Andalusia, Catalonia, Galicia, Madrid, Valencia and the Basque Country) between March 2011 and June 2012. The autonomous regions were selected based on their population size, geographic dispersion and likelihood of requesting and/or using these data for decision-making. In each autonomous region, the sample size was proportional to their population aged ≥65 years. To reflect the different regional health structures, the number of patients included for each hospital size (small: <200 beds, medium: 200–500 beds, large: >500 beds) was representative of the real distribution of fractures in each autonomous region's clinical practice.
Patients (≥65 years of age) admitted to hospital with a first osteoporotic hip fracture in Spain per Autonomous Regions(low-impact trauma fracture or fall from a height equal to or less than their height or any mild or moderate trauma not caused by a fall) were included.10 Patients with a secondary hip fracture in Spain per Autonomous Regions due to severe trauma (fall from a height above that of a stool, chair or first step of a staircase, or due to severe trauma not caused by a fall), with an acute concurrent fracture not of the hip, a neoplasm or primary bone disease, or having participated in any clinical trial over the past 6 months were excluded from the study.
The protocol was approved by an independent ethical committee, and all the patients signed their informed consent before inclusion in the study.
The patients were followed-up over the 12 months after their fracture. The baseline data were recorded (first hospital admission), on discharge from hospital, and at 4 and 12 months after the fracture. The demographic data, fracture risk factors and comorbidities (according to the Charlson Comorbidity Index11) were gathered at baseline. Fracture-related HRU was recorded at each visit: hospital care, re-hospitalisation, care, home visits and/or telephone support, rehabilitation, walking aids, number of visits to the emergency department, formal and/or informal home care, HRQoL (Euroqol five-dimension questionnaire [EQ-5D]),12 and patient autonomy (modified Barthel index13 and the Harris hip score).14 HRU data was not collected at the time of death.
Statistical analysisThe perspective of the Spanish health system was used to estimate the HRU (except for informal home care resources). The unit costs were obtained from the eSalud database (http://www.oblikue.com/bddcostes) and adjusted to 2012 values. The mean annual costs and the 95% confidence intervals (CI) (by 1000 bootstrap replications) were calculated. The hip fracture in Spain per Autonomous Regions-related cost was calculated as the difference between the care required before and after the fracture.15
All the analyses were descriptive and no statistical comparisons were made between groups of patients. The results of the HRQoL scales and autonomy on discharge, and at 12 months were compared to the baseline in each autonomous region. The statistical analyses were performed using SAS software (SAS Institute, Inc, Cary, NC, USA).
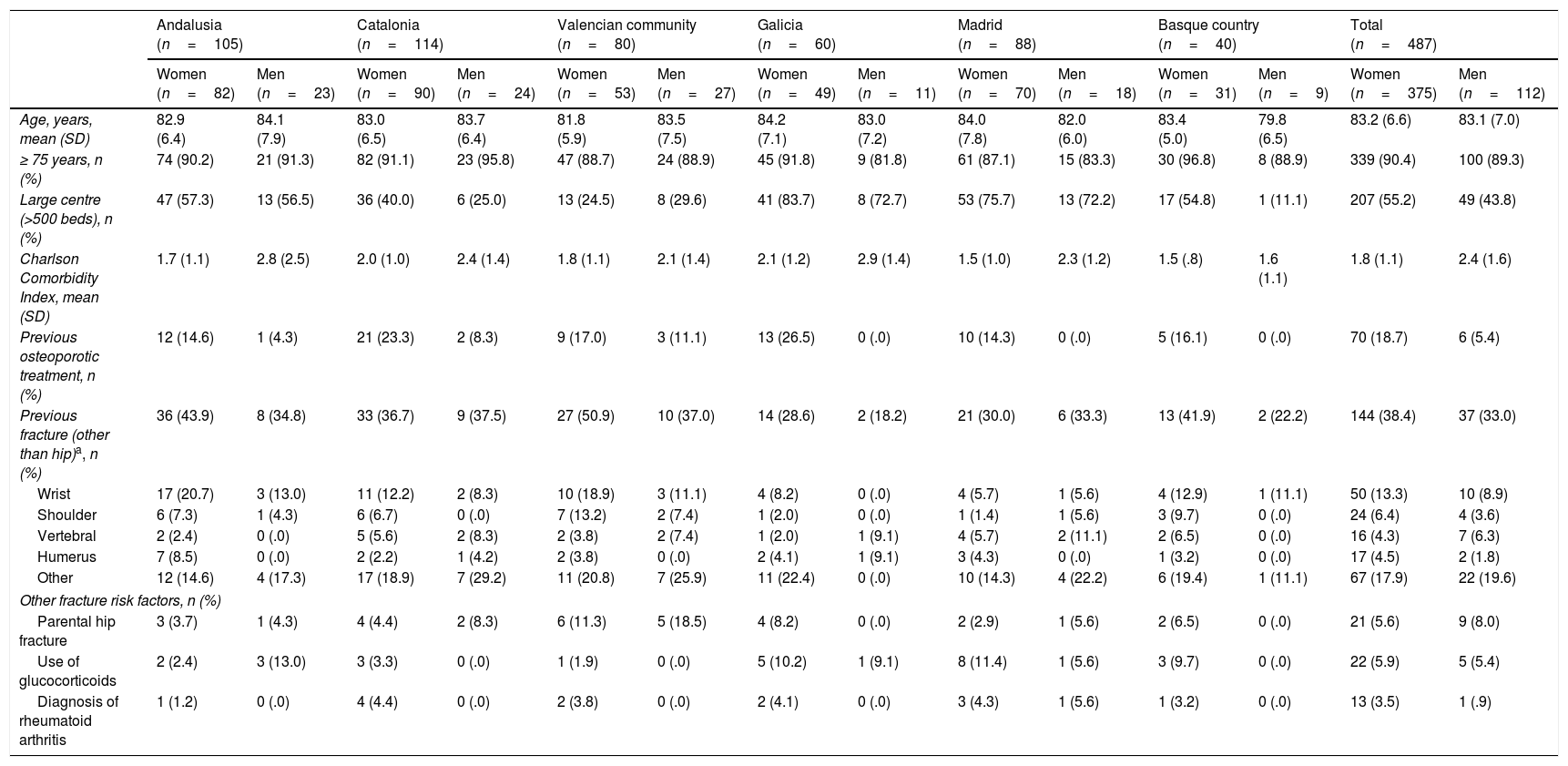
ResultsBaseline demographic and clinical featuresThe demographic and clinical features of the population per autonomous region and sex are described in Table 1. A total of 487 patients were included. Of them, 73% (n=357) were followed up over one year. The majority of early withdrawals were due to the death of the patient (77/130, 59%). Most of the patients included in the study were female (77%), with a mean age (standard deviation, SD) of between 79.8 (6.5) and 84.2 (7.1) years among the subgroups per region and sex (Table 1).
Main baseline features of the population per autonomous community and sex.
| Andalusia (n=105) | Catalonia (n=114) | Valencian community (n=80) | Galicia (n=60) | Madrid (n=88) | Basque country (n=40) | Total (n=487) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Women (n=82) | Men (n=23) | Women (n=90) | Men (n=24) | Women (n=53) | Men (n=27) | Women (n=49) | Men (n=11) | Women (n=70) | Men (n=18) | Women (n=31) | Men (n=9) | Women (n=375) | Men (n=112) | |
| Age, years, mean (SD) | 82.9 (6.4) | 84.1 (7.9) | 83.0 (6.5) | 83.7 (6.4) | 81.8 (5.9) | 83.5 (7.5) | 84.2 (7.1) | 83.0 (7.2) | 84.0 (7.8) | 82.0 (6.0) | 83.4 (5.0) | 79.8 (6.5) | 83.2 (6.6) | 83.1 (7.0) |
| ≥ 75 years, n (%) | 74 (90.2) | 21 (91.3) | 82 (91.1) | 23 (95.8) | 47 (88.7) | 24 (88.9) | 45 (91.8) | 9 (81.8) | 61 (87.1) | 15 (83.3) | 30 (96.8) | 8 (88.9) | 339 (90.4) | 100 (89.3) |
| Large centre (>500 beds), n (%) | 47 (57.3) | 13 (56.5) | 36 (40.0) | 6 (25.0) | 13 (24.5) | 8 (29.6) | 41 (83.7) | 8 (72.7) | 53 (75.7) | 13 (72.2) | 17 (54.8) | 1 (11.1) | 207 (55.2) | 49 (43.8) |
| Charlson Comorbidity Index, mean (SD) | 1.7 (1.1) | 2.8 (2.5) | 2.0 (1.0) | 2.4 (1.4) | 1.8 (1.1) | 2.1 (1.4) | 2.1 (1.2) | 2.9 (1.4) | 1.5 (1.0) | 2.3 (1.2) | 1.5 (.8) | 1.6 (1.1) | 1.8 (1.1) | 2.4 (1.6) |
| Previous osteoporotic treatment, n (%) | 12 (14.6) | 1 (4.3) | 21 (23.3) | 2 (8.3) | 9 (17.0) | 3 (11.1) | 13 (26.5) | 0 (.0) | 10 (14.3) | 0 (.0) | 5 (16.1) | 0 (.0) | 70 (18.7) | 6 (5.4) |
| Previous fracture (other than hip)a, n (%) | 36 (43.9) | 8 (34.8) | 33 (36.7) | 9 (37.5) | 27 (50.9) | 10 (37.0) | 14 (28.6) | 2 (18.2) | 21 (30.0) | 6 (33.3) | 13 (41.9) | 2 (22.2) | 144 (38.4) | 37 (33.0) |
| Wrist | 17 (20.7) | 3 (13.0) | 11 (12.2) | 2 (8.3) | 10 (18.9) | 3 (11.1) | 4 (8.2) | 0 (.0) | 4 (5.7) | 1 (5.6) | 4 (12.9) | 1 (11.1) | 50 (13.3) | 10 (8.9) |
| Shoulder | 6 (7.3) | 1 (4.3) | 6 (6.7) | 0 (.0) | 7 (13.2) | 2 (7.4) | 1 (2.0) | 0 (.0) | 1 (1.4) | 1 (5.6) | 3 (9.7) | 0 (.0) | 24 (6.4) | 4 (3.6) |
| Vertebral | 2 (2.4) | 0 (.0) | 5 (5.6) | 2 (8.3) | 2 (3.8) | 2 (7.4) | 1 (2.0) | 1 (9.1) | 4 (5.7) | 2 (11.1) | 2 (6.5) | 0 (.0) | 16 (4.3) | 7 (6.3) |
| Humerus | 7 (8.5) | 0 (.0) | 2 (2.2) | 1 (4.2) | 2 (3.8) | 0 (.0) | 2 (4.1) | 1 (9.1) | 3 (4.3) | 0 (.0) | 1 (3.2) | 0 (.0) | 17 (4.5) | 2 (1.8) |
| Other | 12 (14.6) | 4 (17.3) | 17 (18.9) | 7 (29.2) | 11 (20.8) | 7 (25.9) | 11 (22.4) | 0 (.0) | 10 (14.3) | 4 (22.2) | 6 (19.4) | 1 (11.1) | 67 (17.9) | 22 (19.6) |
| Other fracture risk factors, n (%) | ||||||||||||||
| Parental hip fracture | 3 (3.7) | 1 (4.3) | 4 (4.4) | 2 (8.3) | 6 (11.3) | 5 (18.5) | 4 (8.2) | 0 (.0) | 2 (2.9) | 1 (5.6) | 2 (6.5) | 0 (.0) | 21 (5.6) | 9 (8.0) |
| Use of glucocorticoids | 2 (2.4) | 3 (13.0) | 3 (3.3) | 0 (.0) | 1 (1.9) | 0 (.0) | 5 (10.2) | 1 (9.1) | 8 (11.4) | 1 (5.6) | 3 (9.7) | 0 (.0) | 22 (5.9) | 5 (5.4) |
| Diagnosis of rheumatoid arthritis | 1 (1.2) | 0 (.0) | 4 (4.4) | 0 (.0) | 2 (3.8) | 0 (.0) | 2 (4.1) | 0 (.0) | 3 (4.3) | 1 (5.6) | 1 (3.2) | 0 (.0) | 13 (3.5) | 1 (.9) |
SD: standard deviation.
The amount of patients included in large centres was higher in Galicia and Madrid (women/males: 72.7%/83.7% and 75.7%/72.2%, respectively) compared to the Valencian Community and Catalonia (24.5%/29.6% and 40.0%/25.0%).
Approximately a third of the patients had sustained a previous fracture other than a hip fracture in Spain per Autonomous Regions, chiefly the wrist, and generally more women than men (except in Catalonia and Madrid, where it was similar between both sexes). At baseline, only 18.7% of the women and 5.4% of the men had received previous osteoporotic treatment, with fewer in the Community of Madrid (women/males: 14.3%/0%) compared to Galicia (26.5%/0.0%) and Catalonia (23.3%/8.3%).
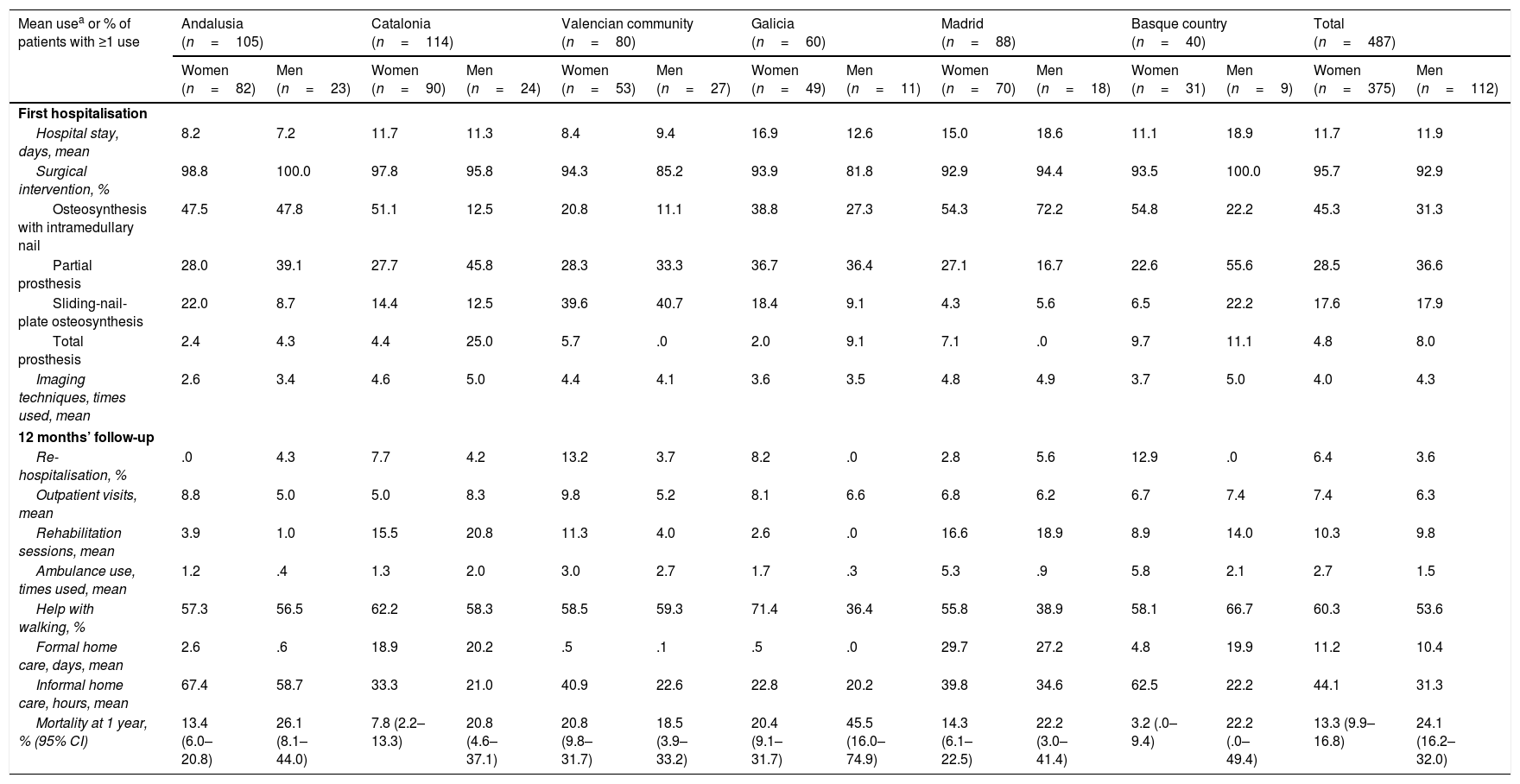
Health resources utilisationHRU was high, both during the first hospitalisation period and during the 12 months of follow-up, with similar results between the sexes in all the autonomous regions, except for the re-hospitalisations, which were generally more frequent for women than men, especially in the Valencian Community (males/women: 13.2%/3.7%), the Basque Country (12.9%/0%) and Galicia (8.2%/.0%). Rehabilitation sessions were more frequent in the Valencian Community for women (11.3/4.0 sessions); help with walking was more frequent in Galicia and Madrid (women/males: 71.4%/36.4% and 55.8%/38.9%, respectively), and informal home care in the Basque Country (women/males: 62.5%/22.2%) (Table 2).
Health resource utilisation (first hospitalisation and at 12 months) per autonomous region.
| Mean usea or % of patients with ≥1 use | Andalusia (n=105) | Catalonia (n=114) | Valencian community (n=80) | Galicia (n=60) | Madrid (n=88) | Basque country (n=40) | Total (n=487) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Women (n=82) | Men (n=23) | Women (n=90) | Men (n=24) | Women (n=53) | Men (n=27) | Women (n=49) | Men (n=11) | Women (n=70) | Men (n=18) | Women (n=31) | Men (n=9) | Women (n=375) | Men (n=112) | |
| First hospitalisation | ||||||||||||||
| Hospital stay, days, mean | 8.2 | 7.2 | 11.7 | 11.3 | 8.4 | 9.4 | 16.9 | 12.6 | 15.0 | 18.6 | 11.1 | 18.9 | 11.7 | 11.9 |
| Surgical intervention, % | 98.8 | 100.0 | 97.8 | 95.8 | 94.3 | 85.2 | 93.9 | 81.8 | 92.9 | 94.4 | 93.5 | 100.0 | 95.7 | 92.9 |
| Osteosynthesis with intramedullary nail | 47.5 | 47.8 | 51.1 | 12.5 | 20.8 | 11.1 | 38.8 | 27.3 | 54.3 | 72.2 | 54.8 | 22.2 | 45.3 | 31.3 |
| Partial prosthesis | 28.0 | 39.1 | 27.7 | 45.8 | 28.3 | 33.3 | 36.7 | 36.4 | 27.1 | 16.7 | 22.6 | 55.6 | 28.5 | 36.6 |
| Sliding-nail-plate osteosynthesis | 22.0 | 8.7 | 14.4 | 12.5 | 39.6 | 40.7 | 18.4 | 9.1 | 4.3 | 5.6 | 6.5 | 22.2 | 17.6 | 17.9 |
| Total prosthesis | 2.4 | 4.3 | 4.4 | 25.0 | 5.7 | .0 | 2.0 | 9.1 | 7.1 | .0 | 9.7 | 11.1 | 4.8 | 8.0 |
| Imaging techniques, times used, mean | 2.6 | 3.4 | 4.6 | 5.0 | 4.4 | 4.1 | 3.6 | 3.5 | 4.8 | 4.9 | 3.7 | 5.0 | 4.0 | 4.3 |
| 12 months’ follow-up | ||||||||||||||
| Re-hospitalisation, % | .0 | 4.3 | 7.7 | 4.2 | 13.2 | 3.7 | 8.2 | .0 | 2.8 | 5.6 | 12.9 | .0 | 6.4 | 3.6 |
| Outpatient visits, mean | 8.8 | 5.0 | 5.0 | 8.3 | 9.8 | 5.2 | 8.1 | 6.6 | 6.8 | 6.2 | 6.7 | 7.4 | 7.4 | 6.3 |
| Rehabilitation sessions, mean | 3.9 | 1.0 | 15.5 | 20.8 | 11.3 | 4.0 | 2.6 | .0 | 16.6 | 18.9 | 8.9 | 14.0 | 10.3 | 9.8 |
| Ambulance use, times used, mean | 1.2 | .4 | 1.3 | 2.0 | 3.0 | 2.7 | 1.7 | .3 | 5.3 | .9 | 5.8 | 2.1 | 2.7 | 1.5 |
| Help with walking, % | 57.3 | 56.5 | 62.2 | 58.3 | 58.5 | 59.3 | 71.4 | 36.4 | 55.8 | 38.9 | 58.1 | 66.7 | 60.3 | 53.6 |
| Formal home care, days, mean | 2.6 | .6 | 18.9 | 20.2 | .5 | .1 | .5 | .0 | 29.7 | 27.2 | 4.8 | 19.9 | 11.2 | 10.4 |
| Informal home care, hours, mean | 67.4 | 58.7 | 33.3 | 21.0 | 40.9 | 22.6 | 22.8 | 20.2 | 39.8 | 34.6 | 62.5 | 22.2 | 44.1 | 31.3 |
| Mortality at 1 year, % (95% CI) | 13.4 (6.0–20.8) | 26.1 (8.1–44.0) | 7.8 (2.2–13.3) | 20.8 (4.6–37.1) | 20.8 (9.8–31.7) | 18.5 (3.9–33.2) | 20.4 (9.1–31.7) | 45.5 (16.0–74.9) | 14.3 (6.1–22.5) | 22.2 (3.0–41.4) | 3.2 (.0–9.4) | 22.2 (.0–49.4) | 13.3 (9.9–16.8) | 24.1 (16.2–32.0) |
Hospital stays were longer in Madrid (mean of 15.0 and 18.6 days for women and men, respectively) and Galicia (16.9 and 12.6 days, respectively), and were shorter in Andalusia and the Valencian Community (8.2 and 7.2 days for women and 8.4 and 9.4 days for men).
Most of the patients underwent surgical intervention, most commonly osteosynthesis with intramedullary nail (45% of the men and 31% of the women).
Formal home care was more common in the regions of Madrid (mean of 30/27 days for women/men) and Catalonia (19/20 days), and less frequent in the Valencian Community (1/0 days), Galicia (1/0 days) and Andalusia (3/1 days).
There were more rehabilitation sessions in Catalonia and Madrid (mean sessions for women/men: 16/21 and 17/19 sessions, respectively), and fewer in Andalusia and Galicia (means of 4/1 and 3/0 sessions for women/men, respectively).
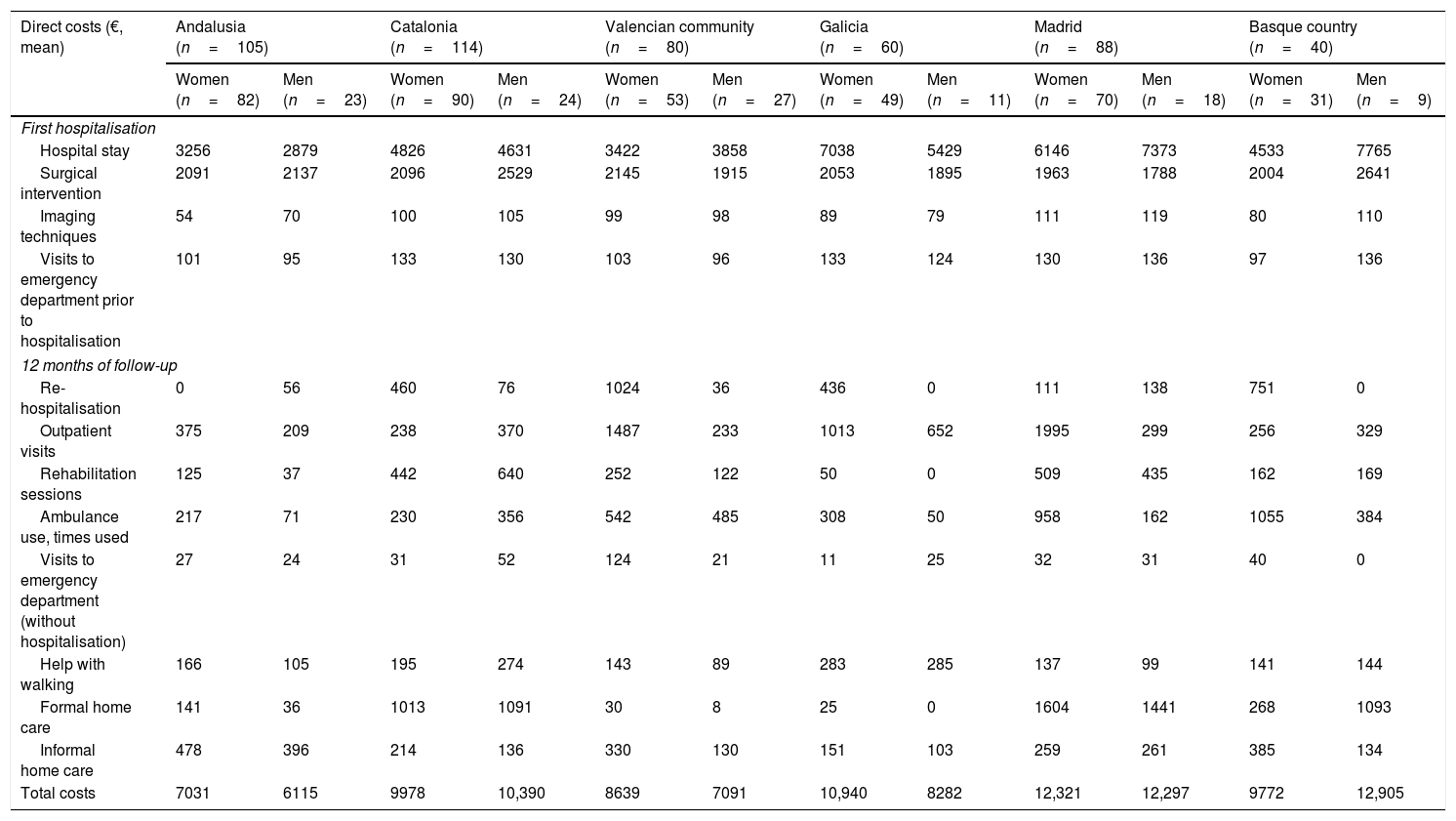
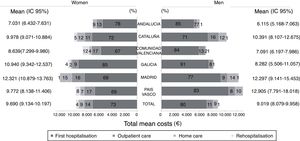
Direct costsThe direct costs over the first year associated with a first osteoporotic hip fracture in Spain per Autonomous Regions are shown in Fig. 1 and Table 3. Madrid was the autonomous region with the highest mean costs (12,321€ for women and 12,297€ for men), whereas Andalusia was the autonomous region with the lowest costs (7031€ for women and 6115€ for men). The main determining factor of cost was the first hospitalisation, which contributed between 67% and 91% to costs, followed by outpatient visits (7%-17%) and home care (1%-15%). Madrid and Galicia were the regions with the highest costs associated with hospital stay (women/men: 6146€/7373€ and 7038€/5429€, respectively) and together with the Valencian Community, were those with the highest costs for outpatient visits (1995€/299€, 1013€/652€ and 1487€/233€, respectively). The costs for rehabilitation sessions and formal home care were high in the autonomous regions of Madrid and Catalonia. Finally, the costs associated with the use of ambulances were also higher in Madrid and the Basque Country especially for women (Table 3).
Direct costs during the first year associated with the different resources used due to hip fracture in Spain per Autonomous Regions per autonomous region.
| Direct costs (€, mean) | Andalusia (n=105) | Catalonia (n=114) | Valencian community (n=80) | Galicia (n=60) | Madrid (n=88) | Basque country (n=40) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Women (n=82) | Men (n=23) | Women (n=90) | Men (n=24) | Women (n=53) | Men (n=27) | Women (n=49) | Men (n=11) | Women (n=70) | Men (n=18) | Women (n=31) | Men (n=9) | |
| First hospitalisation | ||||||||||||
| Hospital stay | 3256 | 2879 | 4826 | 4631 | 3422 | 3858 | 7038 | 5429 | 6146 | 7373 | 4533 | 7765 |
| Surgical intervention | 2091 | 2137 | 2096 | 2529 | 2145 | 1915 | 2053 | 1895 | 1963 | 1788 | 2004 | 2641 |
| Imaging techniques | 54 | 70 | 100 | 105 | 99 | 98 | 89 | 79 | 111 | 119 | 80 | 110 |
| Visits to emergency department prior to hospitalisation | 101 | 95 | 133 | 130 | 103 | 96 | 133 | 124 | 130 | 136 | 97 | 136 |
| 12 months of follow-up | ||||||||||||
| Re-hospitalisation | 0 | 56 | 460 | 76 | 1024 | 36 | 436 | 0 | 111 | 138 | 751 | 0 |
| Outpatient visits | 375 | 209 | 238 | 370 | 1487 | 233 | 1013 | 652 | 1995 | 299 | 256 | 329 |
| Rehabilitation sessions | 125 | 37 | 442 | 640 | 252 | 122 | 50 | 0 | 509 | 435 | 162 | 169 |
| Ambulance use, times used | 217 | 71 | 230 | 356 | 542 | 485 | 308 | 50 | 958 | 162 | 1055 | 384 |
| Visits to emergency department (without hospitalisation) | 27 | 24 | 31 | 52 | 124 | 21 | 11 | 25 | 32 | 31 | 40 | 0 |
| Help with walking | 166 | 105 | 195 | 274 | 143 | 89 | 283 | 285 | 137 | 99 | 141 | 144 |
| Formal home care | 141 | 36 | 1013 | 1091 | 30 | 8 | 25 | 0 | 1604 | 1441 | 268 | 1093 |
| Informal home care | 478 | 396 | 214 | 136 | 330 | 130 | 151 | 103 | 259 | 261 | 385 | 134 |
| Total costs | 7031 | 6115 | 9978 | 10,390 | 8639 | 7091 | 10,940 | 8282 | 12,321 | 12,297 | 9772 | 12,905 |
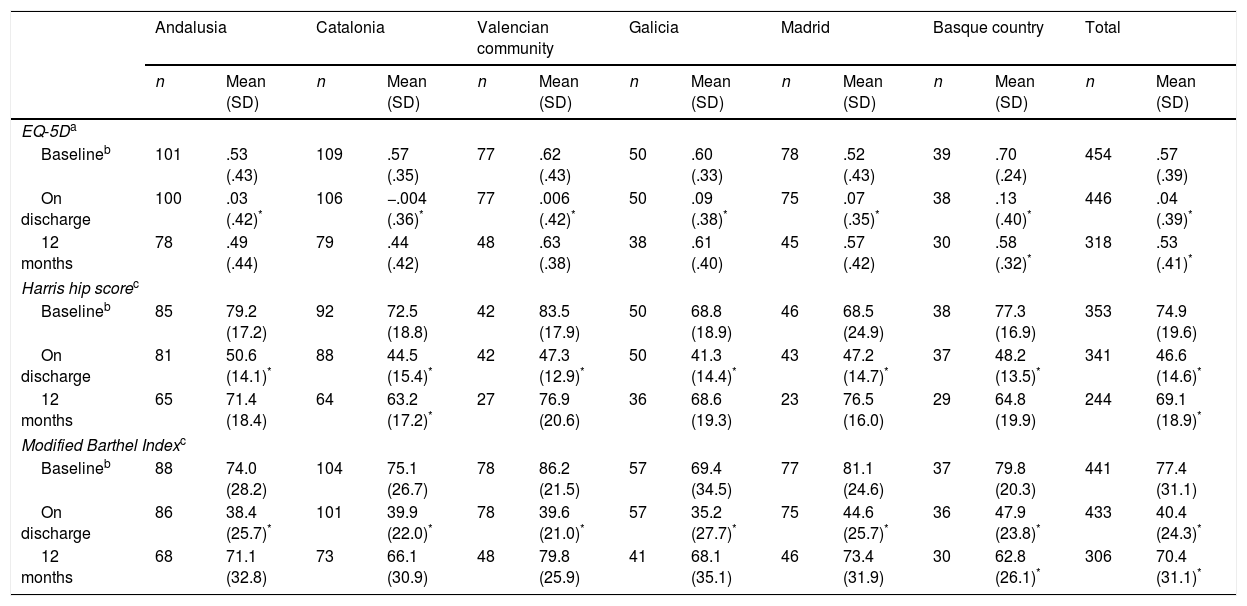
During hospitalisation, there was significant reduction in HRQoL and autonomy; this was of the same magnitude in all the autonomous regions. After discharge the values recovered, although at 12 months the scores were still slightly lower than those prior to the fracture, except in Madrid, Galicia and the Valencian Community, where the final EQ-5D scores (and the Harris hip score in Madrid) were slightly higher than those prior to the fracture. The loss at 12 months remained significant in patients in the Basque Country (according to the EQ-5D and the modified Barthel index), and those of Catalonia (according to the Harris hip score) (Table 4).
Patient quality of life and autonomy per autonomous community.
| Andalusia | Catalonia | Valencian community | Galicia | Madrid | Basque country | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| EQ-5Da | ||||||||||||||
| Baselineb | 101 | .53 (.43) | 109 | .57 (.35) | 77 | .62 (.43) | 50 | .60 (.33) | 78 | .52 (.43) | 39 | .70 (.24) | 454 | .57 (.39) |
| On discharge | 100 | .03 (.42)* | 106 | −.004 (.36)* | 77 | .006 (.42)* | 50 | .09 (.38)* | 75 | .07 (.35)* | 38 | .13 (.40)* | 446 | .04 (.39)* |
| 12 months | 78 | .49 (.44) | 79 | .44 (.42) | 48 | .63 (.38) | 38 | .61 (.40) | 45 | .57 (.42) | 30 | .58 (.32)* | 318 | .53 (.41)* |
| Harris hip scorec | ||||||||||||||
| Baselineb | 85 | 79.2 (17.2) | 92 | 72.5 (18.8) | 42 | 83.5 (17.9) | 50 | 68.8 (18.9) | 46 | 68.5 (24.9) | 38 | 77.3 (16.9) | 353 | 74.9 (19.6) |
| On discharge | 81 | 50.6 (14.1)* | 88 | 44.5 (15.4)* | 42 | 47.3 (12.9)* | 50 | 41.3 (14.4)* | 43 | 47.2 (14.7)* | 37 | 48.2 (13.5)* | 341 | 46.6 (14.6)* |
| 12 months | 65 | 71.4 (18.4) | 64 | 63.2 (17.2)* | 27 | 76.9 (20.6) | 36 | 68.6 (19.3) | 23 | 76.5 (16.0) | 29 | 64.8 (19.9) | 244 | 69.1 (18.9)* |
| Modified Barthel Indexc | ||||||||||||||
| Baselineb | 88 | 74.0 (28.2) | 104 | 75.1 (26.7) | 78 | 86.2 (21.5) | 57 | 69.4 (34.5) | 77 | 81.1 (24.6) | 37 | 79.8 (20.3) | 441 | 77.4 (31.1) |
| On discharge | 86 | 38.4 (25.7)* | 101 | 39.9 (22.0)* | 78 | 39.6 (21.0)* | 57 | 35.2 (27.7)* | 75 | 44.6 (25.7)* | 36 | 47.9 (23.8)* | 433 | 40.4 (24.3)* |
| 12 months | 68 | 71.1 (32.8) | 73 | 66.1 (30.9) | 48 | 79.8 (25.9) | 41 | 68.1 (35.1) | 46 | 73.4 (31.9) | 30 | 62.8 (26.1)* | 306 | 70.4 (31.1)* |
SD: standard deviation.
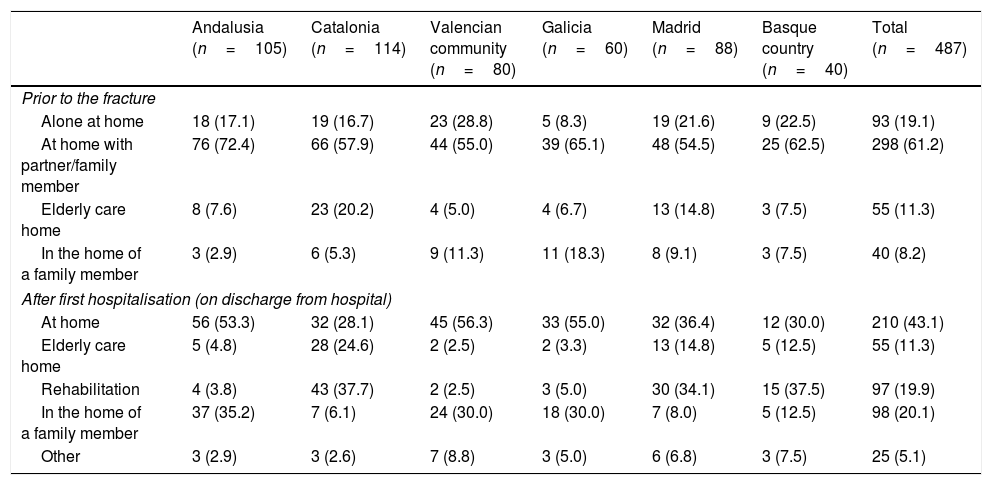
Differences were observed in the amount of patients institutionalised prior to the fracture. These were highest in Catalonia (20.2%) and Madrid (14.8%) than in the other autonomous regions (5.0%-7.6%). After discharge from hospital, Catalonia and Madrid continued to maintain amounts similar to and higher than those of the remaining autonomous regions of patients in care homes for the elderly, whereas in the Basque Country there was a slight increase in institutionalised patients. Similarly, there were quantitatively important differences in the amounts of patients in rehabilitation units, clearly higher in Catalonia, the Basque Country and Madrid (37.7%, 37.5% and 34.1%, respectively) than in the other regions (between 3.8% and 5.0%) (Table 5).
Patients’ place of residence before the hip fracture in Spain per Autonomous Regions and after discharge from hospital.
| Andalusia (n=105) | Catalonia (n=114) | Valencian community (n=80) | Galicia (n=60) | Madrid (n=88) | Basque country (n=40) | Total (n=487) | |
|---|---|---|---|---|---|---|---|
| Prior to the fracture | |||||||
| Alone at home | 18 (17.1) | 19 (16.7) | 23 (28.8) | 5 (8.3) | 19 (21.6) | 9 (22.5) | 93 (19.1) |
| At home with partner/family member | 76 (72.4) | 66 (57.9) | 44 (55.0) | 39 (65.1) | 48 (54.5) | 25 (62.5) | 298 (61.2) |
| Elderly care home | 8 (7.6) | 23 (20.2) | 4 (5.0) | 4 (6.7) | 13 (14.8) | 3 (7.5) | 55 (11.3) |
| In the home of a family member | 3 (2.9) | 6 (5.3) | 9 (11.3) | 11 (18.3) | 8 (9.1) | 3 (7.5) | 40 (8.2) |
| After first hospitalisation (on discharge from hospital) | |||||||
| At home | 56 (53.3) | 32 (28.1) | 45 (56.3) | 33 (55.0) | 32 (36.4) | 12 (30.0) | 210 (43.1) |
| Elderly care home | 5 (4.8) | 28 (24.6) | 2 (2.5) | 2 (3.3) | 13 (14.8) | 5 (12.5) | 55 (11.3) |
| Rehabilitation | 4 (3.8) | 43 (37.7) | 2 (2.5) | 3 (5.0) | 30 (34.1) | 15 (37.5) | 97 (19.9) |
| In the home of a family member | 37 (35.2) | 7 (6.1) | 24 (30.0) | 18 (30.0) | 7 (8.0) | 5 (12.5) | 98 (20.1) |
| Other | 3 (2.9) | 3 (2.6) | 7 (8.8) | 3 (5.0) | 6 (6.8) | 3 (7.5) | 25 (5.1) |
The percentages were calculated for the total population of each autonomous region, Lost data: n=1 in Galicia, prior to the fracture and after the first hospitalisation, and n=1 in Catalonia, after the first hospitalisation.
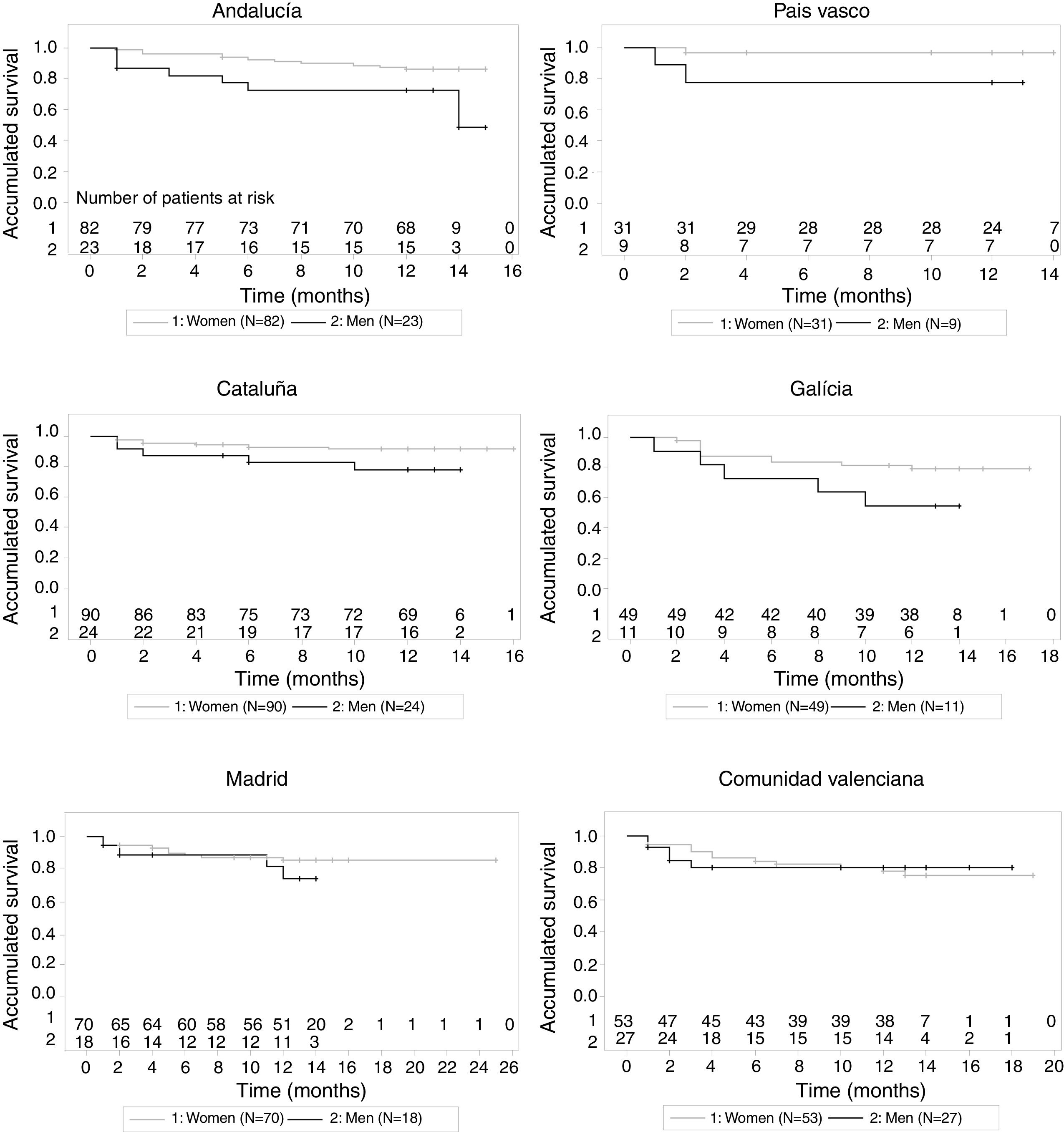
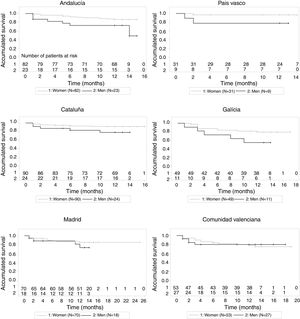
During the 12 months of follow-up, Galicia saw the highest mortality (women/men: 20.4%/45.5%) and in the Valencian Community (20.8%/18.5%), and Catalonia (7.8%/20.8%), and the Basque Country (3.2%/22.2%) the lowest. Mortality was numerically higher for men than women in all the autonomous regions (Fig. 2 and Table 2).
DiscussionTo our knowledge, this is the first study to estimate HRU and the direct costs associated with a first osteoporotic hip fracture in Spain per Autonomous Regions separately in six of our country's autonomous regions.
The sociodemographic characteristics of the population analysed were similar to those obtained in the 2010 Health Statistics in Spain's National Health System (SNS) hospitals,16 with a higher percentage of women, and a mean age of approximately 83 years.
Previous fractures (other than hip) were generally more common in women throughout the autonomous regions. However, we observed a small percentage of patients treated for osteoporosis prior to their fracture, similar to that observed in a Spanish study on women aged 50 and above, which showed considerable underuse of osteoporotic treatments (7%-41% of women not treated despite meeting osteoporosis guideline criteria), particularly in older women, at high risk or with previous osteoporotic fractures.17
The results of our study show high HRU during hospitalisation, similar to that observed in previous studies,18,19 principally due to prolonged hospital stay and more than 90% of patients requiring surgery. Hospital stays were longer in Madrid and Galicia, due perhaps to the greater amount of patients from the large centres of these communities, and the impossibility of these centres to refer patients to medium-stay hospitals. In addition, these differences might relate to surgical delay. A recently published study shows hospital stay to be prolonged by 1.8 days for each day that hip surgery is delayed.20 The cost per day of hospital stay has been estimated at 1000€,6 therefore a delay of only one day in hip surgery involves an extra cost of approximately 1800€. These data are comparable with those published in 2008 on SNS hospitals,16 where the mean duration of hospitalisation in Madrid and Galicia was 18 and 16 days respectively, whereas it was 12 and 11 days in Andalusia and the Valencian Community, respectively, with the consequent differences In associated costs.
The results also highlight relevant differences in the use of other types of health resources, principally those associated with patient care outside the hospital. Madrid and Catalonia, followed by the Basque Country, were the autonomous regions with the highest number of rehabilitation sessions and days of formal home care, at figures between 3 and 12 times higher than those observed in Andalusia and the Valencian Community. It is worth noting, however, that the lower health resource utilisation in these two regions was not associated with poorer recovery of these patients’ HRQoL or autonomy at 12 months, which seems to suggest that care outside the hospital in these two communities is carried out effectively by families or other types of informal carers.
In our study, the costs associated with first hospitalisation contributed to the total costs, and were similar to those applied in the Associated Diagnostic Groups applicable to hip fracture in Spain per Autonomous Regions in Spain.16 Per autonomous region, Madrid was one of the regions with highest costs associated with hospital stay and outpatient visits. Together with Catalonia, Madrid had higher costs for rehabilitation sessions and formal home care, and more patients admitted to care homes. By contrast, Andalusia, the Valencian Community and Galicia had lower costs and more patients in their own home or that of family members before and after hospitalisation. A plausible explanation for the differences in costs after first hospitalisation might be the lower requirement for health resources because there is greater social support in these communities, which are also characterised by more rural populations, with associated differences in terms of accessibility and provision of these services, compared to the situation in Catalonia and Madrid.
With regard to intangible costs, various studies have shown the impact of fracture-related disability on patients’ HRQoL.21,22 In our study, patients’ HRQoL and autonomy majorly reduced during hospitalisation in all the autonomous regions. Although they recovered their HRQoL at 12 months, it remained slightly reduced compared to before the fracture (except in Madrid and Galicia). This coincides with a study on patients aged 50 and over, which showed a considerable reduction in HRQoL in the first month after the fracture, and recovery was still not complete at 36 months.23
Our study has some limitations. One of which is the possible selection bias of the sample, since, despite being a multi-centre study, non-probability sampling does not ensure the representativeness of the population under study. Furthermore, some of the subgroups analysed had a limited sample size (fewer than 30 individuals), which makes it difficult to draw reliable conclusions. Due to the observational design of the study, the total cost might have been underestimated due to a lack of information on the resources used at time of death. The low percentage of rehospitalisations obtained, compared to that of the previous available evidence,24,25 suggests possible bias in collecting this variable. Therefore there might have been a slight underestimation of HRU and costs. In addition, although the total hospital stay was included as a variable, the surgical delay in the first hospitalisation was not gathered, which was an aspect that might partially explain the differences observed in the costs between the autonomous regions. Finally, the associated pharmaceutical costs were not taken into account. We consider that further comparative studies should be undertaken.
In conclusion, osteoporotic hip fracture in Spain per Autonomous Regions involves high costs for regional health systems, principally due to high health resource utilisation during first hospitalisation, and outpatient care during the months following it. Notable differences were observed in HRU and costs between the different autonomous regions which might be due to differences in health policies and the intrinsic features of the autonomous regions, and the variability in the management of the process between the different hospitals. Hip fracture in Spain per Autonomous Regions is associated with a marked reduction in quality of life and autonomy and with high mortality in the first year. Although approximately one in 3 patients had suffered a previous fracture other than of the hip, only in 6 had received osteoporotic treatment, which suggests inadequate prevention of this costly complication. A national approach to this health problem and consensus on common action guidelines is desirable, and could offer great social and economic benefits.
Level of evidenceLevel of evidence IV.
FinancingThe study was financed by Amgen, S.A.
AuthorshipA. Bartra, J.R. Caeiro, M. Mesa-Ramos, I. Etxebarría-Foronda, J. Montejo and P. Carpintero participated in the data collection and analysis, and in interpreting the results.
F. Sorio-Vilela, S. Gatell and L. Canals designed the study and supervised the field work. J.R. Caeiro contributed to the conception and design of the study.
All the signatories participated in drafting the manuscript and its critical review, and accepted its final version.
Conflict of interestsJ.R. Caeiro has received research grants from Lilly and Amgen, and has been a speaker at scientific events of Lilly, Merck, Pfizer and Servier. M. Mesa-Ramos is chairman of the SATO Foundation (Andalusian Society of Traumatology and Orthopaedics). P. Carpintero is a lecturer at the University of Cordoba, has received research grants from Amgen, MSD, Lilly and Nycomed, has been a speaker at scientific events of Amgen, MSD, Lilly, Nycomed, Servier, GlaxoSmithKline and AbbVie, and has been a consultant to MSD, Lilly and Bayer. A. Bartra, I. Etxebarría-Foronda and J. Montejo have no conflicts of interests to declare. S. Gatell and L. Canals are employees of Amgen S.A., F. Sorio-Vilela is an employee of Amgen GmbH., F. Sorio-Vilela, S. Gatell and L. Canals are shareholders in Amgen.
We would like to acknowledge the collaboration of Drs Neus Valveny, Juan Martín and Montserrat Sabaté from TFS Develop in writing this manuscript. The authors would like to thank Dr Jorge Arellano (Amgen Inc.) for his contribution to the study design, Andrea Farré (Amgen S.A.) for her contribution to the experimental work, and all the PROA study researchers (in alphabetical order by hospital name):
Complejo Hospitalario Ourense: Dr Antonio Fernández-Cebrián; Complejo Hospitalario Pontevedra – Hospital Montecelo: Dr Eduardo Vaquero-Cervino; Complejo Hospitalario Santiago – Hospital Médico Quirúrgico de Conxo: Dr José Ramón Caeiro; Fundación Jiménez Díaz: Dr Emilio Calvo; Hospital Alto Deba: Dr Íñigo Etxebarría-Foronda; Hospital Comarcal Sant Bernabé de Berga, Dr Pere Mir-Batlle; Hospital da Costa: Dr Luís-Ángel Montero-Furelos; Hospital de El Escorial: Dr Guillermo Sánchez-Inchausti; Hospital General Universitario de Alicante: Dr Isabel Serralta-Davia; Hospital General de Vic: Dr Joaquín Rodríguez-Miralles; Hospital Lluís Alcanyís: Dr Vicente Climent-Peris; Hospital Municipal de Badalona: Dr Núria Galofré-Álvaro, Dr Ana Serrado-Iglesias, Dr Josefa Torres-Martínez; Hospital Regional Universitario Carlos Haya: Dr Manuel Bravo-Bardají; Hospital San Agustín de Linares: Dr Alberto Delgado-Martínez; Hospital Txagorritxu: Dr Rubén Goñi-Robledo, Dr Naiara Gorostiaga-Perez; Hospital Universitari Germans Trias i Pujol: Dr Xavier Granero-Xiberta; Hospital Universitari Mútua de Terrassa: Dr Agustí Bartra-Ylla; Hospital Universitari Vall d’Hebron: Dr Vicente Molero-García; Hospital Universitario Donostia: Dr Gaspar de la Herran-Núñez; Hospital Universitario Fundación Alcorcón: Dr Jorge Montejo-Sancho; Hospital Universitario de Getafe: Dr Leocadio Rodríguez-Mañas, Dr Cristina Alonso-Bouzón, Dr Olga Laosa-Zafra; Hospital Universitario Infanta Leonor: Dr Fátima Brañas-Baztán; Hospital Universitario Ramón y Cajal: Dr Susana Alonso-Güemes; Hospital Universitario Reina Sofía: Dr Pedro Carpintero-Benítez; Hospital Universitario de la Ribera: Dr Francisco José Tarazona-Santabalbina; Hospital Valle de los Pedroches: Dr Manuel Mesa-Ramos; Hospital de Vinarós: Dr Miguel-Angel Valero-Queralt; Hospital Virgen de la Macarena: Dr Luís-Javier Roca-Ruíz.
Please cite this article as: Bartra A, Caeiro J-R, Mesa-Ramos M, Etxebarría-Foronda I, Montejo J, Carpintero P, et al. Coste de la fractura de cadera osteoporótica en España por comunidad autónoma. Rev Esp Cir Ortop Traumatol. 2019;63:56–68.