To evaluate the incidence of venous thromboembolism in spine surgery with no chemical and mechanical prophylaxis, and to determine the specific risk factors for this complication.
Materials and methodsA historical cohort was analysed. All patients subjected to major spinal surgery, between January 2010 and September 2014, were included. No chemical or mechanical prophylaxis was administered in any patient. Active mobilisation of lower limbs was indicated immediately after surgery, and early ambulation started in the first 24–48h after surgery. Clinically symptomatic cases were confirmed by Doppler ultrasound of the lower limbs or chest CT angiography.
ResultsA sample of 1092 cases was studied. Thromboembolic events were observed in 6 cases (.54%); 3 cases (.27%) with deep venous thrombosis and 3 cases (.27%) with pulmonary thromboembolism. A lethal case was identified (.09%). There were no cases of major bleeding or epidural haematoma. The following risk factors were identified: a multilevel fusion at more than 4 levels, surgeries longer than 130min, patients older than 70 years of age, hypertension, and degenerative scoliosis.
DiscussionThere is little scientific evidence on the prevention of thromboembolic events in spinal surgery. In addition to the disparity of prophylactic methods indicated by different specialists, it is important to weigh the risk-benefit of intra- and post-operative bleeding, and even the appearance of an epidural haematoma. Prophylaxis should be assessed in elderly patients over 70 years old, who are subjected to surgeries longer than 130min, when 4 or more levels are involved.
Evaluar la incidencia de enfermedad tromboembólica venosa sin profilaxis química o mecánica y valorar factores de riesgo específicos.
Material y métodosRealizamos un estudio de cohorte histórica en pacientes sometidos a cirugía espinal mayor, entre enero de 2010 y septiembre de 2014, con un total de 1.092 casos. En ningún paciente se administró tromboprofilaxis perioperatoria química o mecánica, indicando la movilización activa de los miembros inferiores y la deambulación precoz en torno a las primeras 24–48h. Los casos clínicamente sintomáticos se confirmaron con eco-doppler de miembros inferiores o angio-TC de tórax.
ResultadosSe identificaron 3 casos (0,27%) con TVP y 3 casos (0,27%) con TEP, con un caso letal (0,09%). En total, los eventos relacionados a ETV ascendieron a 0,54% (n=5). No hubo casos de complicaciones de sangrado mayor o hematoma epidural. Se identificaron los siguientes factores de riesgo: cirugías de 4 o más niveles, intervenciones más largas de 130min, más de 70 años de edad, el padecimiento de HTA y el diagnóstico de escoliosis degenerativa.
DiscusiónEn cirugía espinal, actualmente existe poca evidencia científica que determine la influencia de los distintos factores de riesgo tromboembólicos y la prevención de los mismos, sumado a la disparidad de los métodos profilácticos indicados por los distintos especialistas, teniendo que sopesar el riesgo de sangrado perioperatorio, incluso la aparición de hematoma epidural. La indicación de profilaxis farmacológica debe valorarse en pacientes mayores de 70 años con HTA, cirugía prolongada más de 130min o de 4 o más niveles.
Venous thromboembolism (VTE) is a known complication in major orthopaedic surgical procedures, and in particular in total arthroplasty of the hip and knee, and in hip fracture surgery. There is an estimated incidence of distal deep vein thrombosis (DVT) of between 40% and 60% and proximal DVT of between 10% and 30% in patients who undergo surgery without any thromboprophylaxis.1 The incidence of symptomatic VTE is 4.3% (2.8% for symptomatic DVT, 1.5% for symptomatic pulmonary thromboembolism [PTE]).2 This has affected surgical practice and thromboembolic prophylaxis is now already considered an obligatory indication in this type of surgery.
It has long been reported that spinal surgery patients are at recognised risk of developing VTE due to prolonged prone position, prolonged surgeries, lying down and limitation of movement.3–5 In orthopaedic surgery the majority of resources have gone into VTE research in knee and hip arthroplasty but the volume of publications relating to spinal surgery complications is substantially limited. Furthermore, the majority of studies reporting on epidemiological values of these events is highly varied with VTE figures being quoted as between 0.3% and 31%, due to the variability of simple sizes and diagnostic methods of detection (clinical evaluation, Doppler screening, phlebograms).3–8 Another aspect which may affect incidence is the variety of spinal injury procedures, the different forms of surgical approach, and the different specific risk factors affecting each individual patient.
The publication of medical guidelines for VTE prophylaxis in different areas of surgery has encouraged specialists in spinal injury to review the matter, with the aim of establishing relevant risk incidence and factors to determine how thromboembolic prophylaxis is to be applied in these patients. It is generally acknowledged that risk for patients undergoing elective spine surgery is low, somewhat higher in oncology surgery and high in trauma surgery with spinal cord injury.9,10 Notwithstanding, there is a lack of homogeneity in the application and election of the type of thromboprophylaxis, which is exacerbated by the individual preferences of the different spinal injury specialists.11,12
In addition to the already difficult task of finding an ideal method of prophylaxis for VTE in these patients is the added problem of haemorrhagic complications of the surgical wound and epidural haematoma (EH), both of which affect the surgeons’ decision when weighing up the risk-benefit balance of different methods of prophylaxis.
Bearing in mind that in our hospital, in practice, there is no thromboembolic prophylaxis other than active lower limb mobilisation for the great majority of patients a few hours after surgery and early ambulation, we developed this study to assess the incidence of VTE in patients with major spinal surgery, with no prophylaxis other than that mentioned above, and to assess the specific risk factors which may lead to this complication.
Materials and methodsAn historical cohort study was designed to include all patients who had undergone major spinal surgery in our hospital between January 2010 and September 2014. Major procedures were defined as those which required general anaesthesia, including anterior or posterior spinal fusion procedures, major reconstructive surgery, decompressions, and discectomies of the spinal, cervical and thoracic column.
The following patients were excluded from this study: those with multiple trauma; with fractures of the lower limbs or other conditions which impeded early ambulation; patients with acute spinal cord injuries classified on the A to D – ASIA impairment scale (AIS); patients with medical procedures requiring therapeutic anticoagulation, and patients with metastatic cancer. Bearing in mind that this study was conducted in the trauma and orthopaedic service for adults in our hospital, no cases of patients under 14 were included.
The demographic data of these patients was collected, including gender, age, diagnosis, type and level of surgery, duration of surgery, hospital stay, the difference between haemoglobin levels before and after surgery, transfusions, comorbidities and smoking habits. None of the patients had been administered chemical or mechanical thromboembolic prophylaxis before or after surgery, with the exception of non-resistant isometric or isotonic exercises immediately after surgery and early ambulation 24–48h after surgery.
They were monitored to detect symptomatology or clinical signs of VTE, using the predictive Wells13 model from admission to hospital discharge, and then later in follow-up consultancies. In accordance with this, a lower limb Doppler scan or computed tomography angiography (CTA) with intravenous contrast was performed on the patients identified as potential carriers of DVT or PTE, depending on the cases.
All patients were assessed daily during their hospital stay, with a mean stay of 7.03±5.7 days (range between 2 and 60 days). They were subsequently assessed in the outpatient spinal unit of our hospital, in all cases (n=1092) for a minimum of 10 weeks and at least 96% (n=1049) for 20 weeks.
The student's t-test was used for comparing continuous variable means and the chi square test for dichotomous variable comparison. The significance level was established for a value equal to P<0.05. Logistic regression analysis was performed for the association of demographic factors, comorbidities and aspects inherent from surgery resulting in VTE, calculating the RR and a 95% confidence interval.
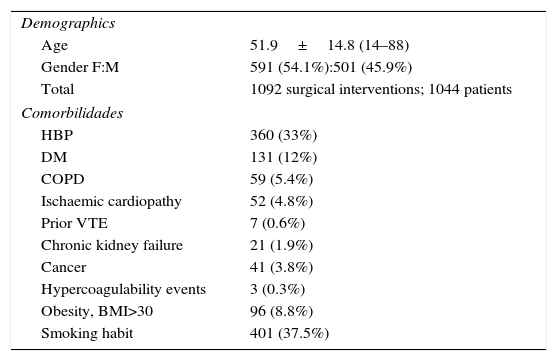
ResultsDuring the period mentioned 1227 major spinal surgeries were performed on 1179 patients. Once the exclusion criteria were applied, 1044 patients were included in the final study (1092 surgical interventions [Table 1]).
Demographics and comorbidities.
| Demographics | |
| Age | 51.9±14.8 (14–88) |
| Gender F:M | 591 (54.1%):501 (45.9%) |
| Total | 1092 surgical interventions; 1044 patients |
| Comorbilidades | |
| HBP | 360 (33%) |
| DM | 131 (12%) |
| COPD | 59 (5.4%) |
| Ischaemic cardiopathy | 52 (4.8%) |
| Prior VTE | 7 (0.6%) |
| Chronic kidney failure | 21 (1.9%) |
| Cancer | 41 (3.8%) |
| Hypercoagulability events | 3 (0.3%) |
| Obesity, BMI>30 | 96 (8.8%) |
| Smoking habit | 401 (37.5%) |
DM: diabetes mellitus; COPD: chronic obstructive pulmonary disaease; VTE: venous thromboembolism; HBP: high blood pressure; BMI: body mass index.
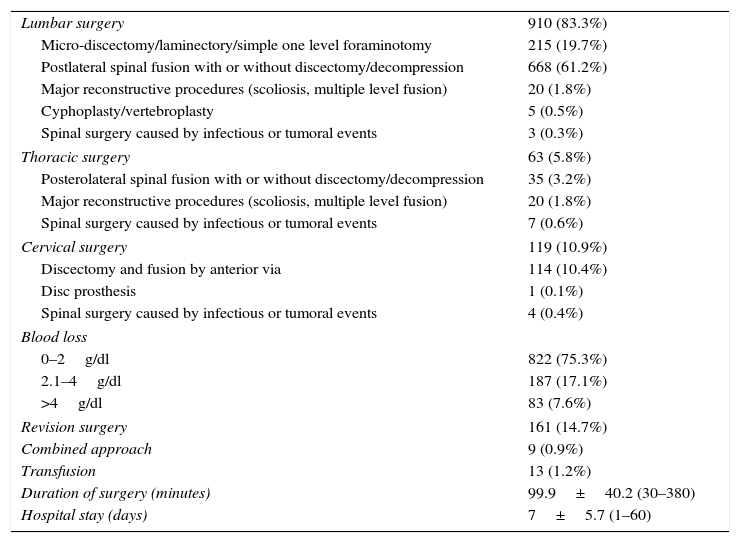
Lumbar spine operations totalled 910, caused by herniated discs (n=218), degenerative discopathy (n=368), canal stenosis (n=139), spondilolisthesis (n=121), fractures of the spine with no neurological compromise (n=36), infectious spondilitis (n=3), degenerative scoliosis (n=24) and idiopathic scoliosis (n=1). 63 thoracic spine interventions were made, caused by idiopathic scoliosis (n=31), spine fractures with no neurological compromise (n=20), infectious or tumoral lesions (n=6), degenerative discopathies (n=3), herniated discs (n=1), canal stenosis (n=1) and spondilolisthesis (n=1). Cervical spine interventions were performed on 119 patients as a consequence of herniated discs (n=27), cervical canal spondilosis with or without myelopathy (n=88) and infectious spondilitis (n=4). Data linked to surgery is shown in Table 2.
Variables relating to surgery.
| Lumbar surgery | 910 (83.3%) |
| Micro-discectomy/laminectory/simple one level foraminotomy | 215 (19.7%) |
| Postlateral spinal fusion with or without discectomy/decompression | 668 (61.2%) |
| Major reconstructive procedures (scoliosis, multiple level fusion) | 20 (1.8%) |
| Cyphoplasty/vertebroplasty | 5 (0.5%) |
| Spinal surgery caused by infectious or tumoral events | 3 (0.3%) |
| Thoracic surgery | 63 (5.8%) |
| Posterolateral spinal fusion with or without discectomy/decompression | 35 (3.2%) |
| Major reconstructive procedures (scoliosis, multiple level fusion) | 20 (1.8%) |
| Spinal surgery caused by infectious or tumoral events | 7 (0.6%) |
| Cervical surgery | 119 (10.9%) |
| Discectomy and fusion by anterior via | 114 (10.4%) |
| Disc prosthesis | 1 (0.1%) |
| Spinal surgery caused by infectious or tumoral events | 4 (0.4%) |
| Blood loss | |
| 0–2g/dl | 822 (75.3%) |
| 2.1–4g/dl | 187 (17.1%) |
| >4g/dl | 83 (7.6%) |
| Revision surgery | 161 (14.7%) |
| Combined approach | 9 (0.9%) |
| Transfusion | 13 (1.2%) |
| Duration of surgery (minutes) | 99.9±40.2 (30–380) |
| Hospital stay (days) | 7±5.7 (1–60) |
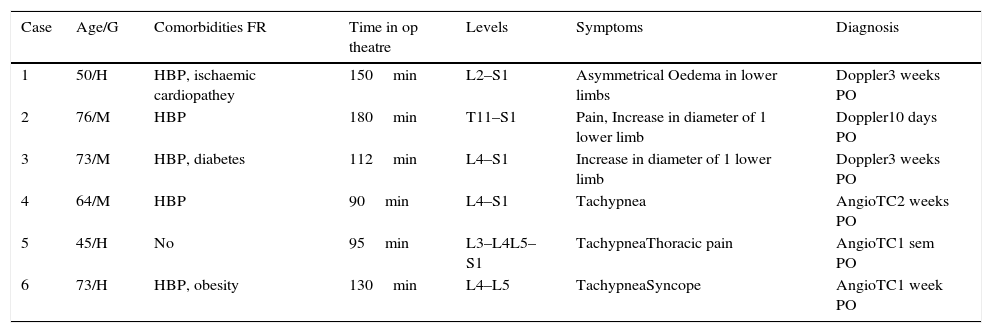
20 patients (1.8%) were identified with clinical signs of VTE, 19 patients underwent lumbar spine surgery and one patient thoracic spine surgery. Imaging scans revealed deep vein thrombosis in 3 of the patients, proximal in the 3 cases (0.27%). In our series there were 3 cases (0.27%) of PTE which was confirmed by angiography of the thorax. In total, events relating to VTE amounted to 0.54% (n=6), and there was a lethal event in one patient who suffered a PTE (0.09%). The other patients satisfactorily responded long-term to anti-coagulating treatment.
There were no cases in our study relating to complications with perioperative bleeding, nor local complications of bleeding to the surgical wound (haematomas, painful wounds), nor any appearance of complicated cases with epidural haematoma.
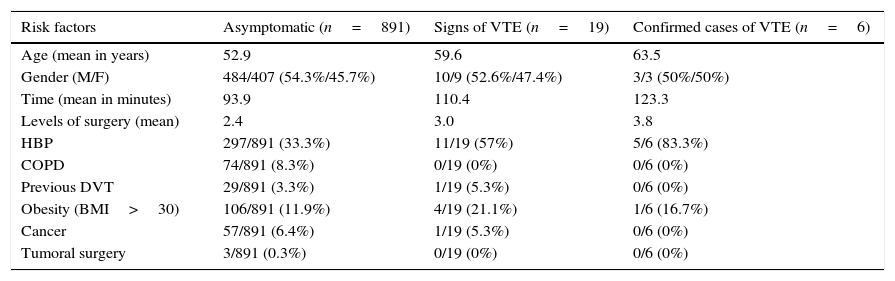
All events relating to VTE occurred in patients who had undergone lumbar surgery, and the specific incidence in this group was 0.65%, 0.32% for DVT and 0.32% for PTE. Table 3 shows the demographic relationship and the risk factors among aymptomatic, symptomatic and confirmed DVT patients. Of these patients 4 cases were surgeries which required instruments or decompression at 3 or more levels, 2 cases of degenerative scoliosis and 2 of canal stenosis. Another patient underwent a discectomy at 2 cervical levels due to 2 acute herniated discs in adjacent segments, with a progressive and disabling mobility outcome for ambulation. The remaining patient had canal stenosis surgery with decompression and instrumentation at 2 levels. Mean to diagnosis was 13 days (ranged between 7 and 20 days) (Table 4).
Comparison of demographic factors and patient risk for lumbar spine surgery.
| Risk factors | Asymptomatic (n=891) | Signs of VTE (n=19) | Confirmed cases of VTE (n=6) |
|---|---|---|---|
| Age (mean in years) | 52.9 | 59.6 | 63.5 |
| Gender (M/F) | 484/407 (54.3%/45.7%) | 10/9 (52.6%/47.4%) | 3/3 (50%/50%) |
| Time (mean in minutes) | 93.9 | 110.4 | 123.3 |
| Levels of surgery (mean) | 2.4 | 3.0 | 3.8 |
| HBP | 297/891 (33.3%) | 11/19 (57%) | 5/6 (83.3%) |
| COPD | 74/891 (8.3%) | 0/19 (0%) | 0/6 (0%) |
| Previous DVT | 29/891 (3.3%) | 1/19 (5.3%) | 0/6 (0%) |
| Obesity (BMI>30) | 106/891 (11.9%) | 4/19 (21.1%) | 1/6 (16.7%) |
| Cancer | 57/891 (6.4%) | 1/19 (5.3%) | 0/6 (0%) |
| Tumoral surgery | 3/891 (0.3%) | 0/19 (0%) | 0/6 (0%) |
COPD: chronic obstructive pulmonary disease; M: male; HBP: high blood pressure; BMI: body mass index; F:female; DVT: deep vein thrombosis.
Cases of lumbar surgery with VTE.
| Case | Age/G | Comorbidities FR | Time in op theatre | Levels | Symptoms | Diagnosis |
|---|---|---|---|---|---|---|
| 1 | 50/H | HBP, ischaemic cardiopathey | 150min | L2–S1 | Asymmetrical Oedema in lower limbs | Doppler3 weeks PO |
| 2 | 76/M | HBP | 180min | T11–S1 | Pain, Increase in diameter of 1 lower limb | Doppler10 days PO |
| 3 | 73/M | HBP, diabetes | 112min | L4–S1 | Increase in diameter of 1 lower limb | Doppler3 weeks PO |
| 4 | 64/M | HBP | 90min | L4–S1 | Tachypnea | AngioTC2 weeks PO |
| 5 | 45/H | No | 95min | L3–L4L5–S1 | TachypneaThoracic pain | AngioTC1 sem PO |
| 6 | 73/H | HBP, obesity | 130min | L4–L5 | TachypneaSyncope | AngioTC1 week PO |
RF: risk factors for VTE; M: male; HBP: high blood pressure; F: female; min: minutes; LL: lower limbs; week PO: post operative week.
Statistical analysis on overall patients was carried out and bearing in mind that the VTE cases were exclusively objectified in patients with lumbar surgery, it was later narrowed down to these patients.
With the inclusion of all patients, we found that the mean age, operating theatre time and number of cervical levels involved was higher in patients with thromboembolic episodes. However, these differences were not statistically significant, probably due to the varied nature of the patients involved, since surgery at all levels was included, and we only found thromboembolic events in lumbosacral surgery.
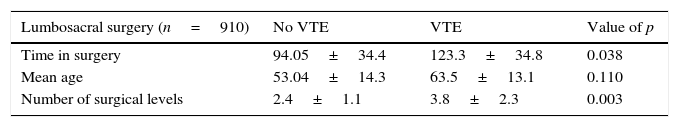
When we analysed only the patients who underwent lumbar surgery (n=910), we found that those who suffered from thromboembolic events were older than the other patients (63.5±13.1 vs 53.04±14.3), although this difference was not statistically significant (P=0.110). The mean duration of surgery was higher for VTE patients (123.3±34.8 vs 94.05±34.4) and this difference was statistically significant (P=0.038 [Table 5]).
Another analysed aspect relating to surgery were the levels established. VTA patients underwent surgery with more levels of instrumentation or decompression (3.8±2.3) than the other patient means (2.4±1.1), and this difference was significant. (P=0.003).
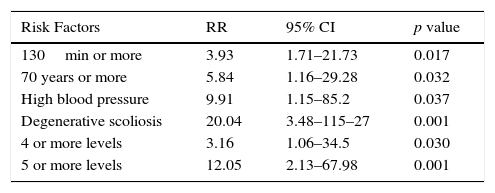
Logistic regression analysis was performed on this data to calculate the risk of patients suffering from VTE in accordance with operating theatre time, age group, number of surgery levels, comorbidities and diagnosis on admission. We found that patients who underwent surgery at 4 or more levels increased the risk, similarly to patients with surgery which lasted over 130min, those who were over 70, those who suffered from HBP or who had been diagnosed with degenerative scoliosis on admission (Table 6).
Regression logistic analysis of risk factors.
| Risk Factors | RR | 95% CI | p value |
|---|---|---|---|
| 130min or more | 3.93 | 1.71–21.73 | 0.017 |
| 70 years or more | 5.84 | 1.16–29.28 | 0.032 |
| High blood pressure | 9.91 | 1.15–85.2 | 0.037 |
| Degenerative scoliosis | 20.04 | 3.48–115–27 | 0.001 |
| 4 or more levels | 3.16 | 1.06–34.5 | 0.030 |
| 5 or more levels | 12.05 | 2.13–67.98 | 0.001 |
CI: confidence interval; min: minutes; RR: relative risk.
Suffering from diseases or conditions relating to the probability of developing VTE (such as obesity, prior VTE, cancer, hypercoaguability) were not relevant to this study.
DiscussionThromboembolic prophylaxis protocols currently exist in the different areas of orthopaedic surgery, although they are not as well defined in spinal surgery. Thromboembolic events, although less frequent than in other orthopaedic procedures, are not absent from spinal surgery. This has determined that prophylaxis guidelines exist in different medical guidelines, such as the American College of Chest Physicians, North American Spine Society and that of SECOT.1,2,9,10,12 Despite the attempt to review current scientific evidence and the intention to include this type of pathological process into the different guidelines, the latter are not very specific in determining which patients are candidates, what type of specific treatment is required or when it should commence and end. In general, the application of mechanical prophylaxis systems is recommended, with the addition of chemoprophylaxis, in high risk patients.
Lack of prophylaxis standardisation may be due to 2 relevant aspects. Firstly, the lack of scientific reports with high levels of proof to determine the real incidence of VTE in spinal surgery, patient type and specific risk factors which determine the population susceptible to prophylaxis and, also what type of prophylaxis to use (or not use?). This is probably due to the fact that VTE has a relatively low incidence in these patients when no method of prophylaxis has been used, compared with other orthopaedic surgery. Studies with a higher proportion of patients offer incidence rates of between 2.7% and 5.8% for DVT and around 0.2% for PTE.4,15 This incidence would also vary depending on the recording method, since it is obviously greater when phlebogram (12.3%) or Doppler scanning (3.7%) screening is performed than when it is clinically recorded (1%).14
Secondly, spine injury is very varied, as are the techniques and approaches to which a patient may be subjected. Furthermore, there are different specialists dedicated to treating it, which indicates prophylaxis more from personal experience than contemporary evidence, with risk of VTE often having to be weighed up against the risk of haemorrhagic events. The latter are infrequent but may have highly negative connotations for patient prognosis.11
To clarify the first aspect, reports with a large number of patients have been published in recent years, to obtain health system data bases. Fineberg et al. published a report based on the obtainment of data base records called the Nationwide Inpatient Sample, grouping together over 570,000 surgical interventions at lumbar level between 2002 and 2009, divided into 2 groups, lumbar decompression and lumbar fusion, with similarities regarding size. A VTE incidence was recorded in 4.9/1000 patients, with significant differences in older patients who were subject to fusion and with further comorbidities. They detected prolonged stay, university hospitals, anaemia, coagulopathies, electrolytic and fluid conditions, obesity and pulmonary circulatory conditions as risk factors.16
Similarly, Schoenfeld et al. published a study of data obtained from the National Surgical Quality Improvement Program of over 27,000 assisted patients in over 250 hospitals. They detected DVT incidence of 0.7% and PTE of 0.4%. They described BMI as >40, age over 80, operating theatre time as over 261min and ASA >3 as factors which increase the risk of suffering from VTE.17
Despite the impact these studies aimed at with large patient numbers recorded, we found there was a fundamental limitation, since neither the method of diagnosis nor the prophylaxis used (if any) was determined and this would have been a relevant factor when bearing in mind the huge disparity of protocols from the different centres and different professionals.
Following on from the search for risk factors, in a cohort study of over 1400 patients, where intermittent pneumatic compression was used, Schulte et al. report that hormone replacement therapy with oestrogens, major depression, and hospital discharge to a rehabilitation centre were separate risk factors involved in VTE.18
Patients at risk have been classified as those who: are at risk of acute spinal lesions, concomitant surgery or lesions of lower limbs, those with a background of VTE, obesity, cancer, hypercoagulability syndromes, or patients with anterior and posterior combined approaches, for whom some kind of prophylaxis was indicated, be it mechanical (graduated compression or intermittent pneumatic compression), chemical (low-molecular-weight heparin or unfractionated low dose heparins), or a combination of both when several risk factors were present. There is some consensus regarding the application of chemical or combined prophylaxis in patients with acute spinal lesions with sustained neurological deficit, where the highest rate of VTE occurred, and the greater benefit of prophylaxis, compensated for the risk of epidural haematomas since functional prognosis in these cases was not compromised.19,20 As an alternative to prophylactic anticoagulation in patients at high risk of bleeding and embolism vena cava filters were used which had favourable results in prevention of PTE. Notwithstanding, there is a percentage of complications which ranges from between 0% and 69%, and the appearance of DVT and post-thrombotic syndrome in lower limbs is not avoided. As a result, it should only be used in very selected cases.8,21
Regarding the disease and its treatment, it is known that in patients who undergo elective surgery there is less incidence of events relating to VTE, but it has not been determined which sub-populations are at the greatest risk in order to indicate a prophylaxis which would be beneficial despite the risk of bleeding, and also cost-effective. The different authors agree in general that the procedures of discectomy or laminectomy at a single level present low risk and that this risk increases when multiple levels are performed together with instrumentation. In one study in which the complications of over 108,000 cases of different spinal surgery were studied, the patients with implants had incidences of DVT, PTE and higher mortality than those who had no implants. In the same study it was also reported that the patients who had undergone primary surgery had a lower rate of DVT than those who had undergone repeated surgery.22
Bearing in mind the above, a classification has been made of the different risk factors derived from the patient and the surgical interventions to which they have been submitted. We are therefore able to decide whether or not to adopt a method of prophylaxis. It is maybe not very clear as to when these methods should be established, especially for anticoagulants, due to the risk of perioperative bleeding. The majority of surgeons prefer to commence prophylaxis 48h after surgery but decide this empirically.10 Neither is the length of duration clear, although the mean time of VTE appearing in these patients is at around 8 days.17
We would be inclined to think that screening all patients could help us in the diagnosis of asymptomatic processes as well as clarifying the real incidence of VTE. However, in major lower limb orthopaedic conditions, it has not been proven that screening has any benefit for asymptomatic patients and may even unnecessarily increase the risk of complications through bleeding due to over-prescribing of antigoagulants, and the American College of Chest Physicians therefore adopts a pose against the conducting of these methods on hospital discharge.2,15
Post-operative complications in the form of post-operative bleeding in patients who are referred for elective spinal surgery is not a minor issue. The appearance of EH in these patients notably affects prognosis negatively. Despite lower rates of VTE being reported, when low-molecular-weight heparins are used (0.01–0.6%),15 the risk of bleeding and the appearance of EH has to be weighed up against this. In this regard, Awad et al. published a study where risk factors for the development of epidural haematomas were analysed, in patients who had undergone spinal surgery, where it was concluded that a well-controlled post-operative anticoagulation did not increase the risk of haematomas, which would in themselves increase with an INR>2.23 Notwithstanding, in this study chemoprophylaxis was very varied, including low-molecular-weight heparins and unfractionated heparins, without determining the pattern of administration of the different guidelines. In systematic reviews the risk of a higher bleeding was stated as being between 0% and 4.3%, with the appearance of haematomas in 10 out of the 2507 patients according to Cheng.24 Sansone, in his meta-analysis, describes the appearance of 8 cases of epidural haematoma in 2071 patients with low-molecular-weight heparin prophylaxis, all of whom required surgical evacuation, and in 3 cases neurological deficit was sustained.14 Al-Dujaili, in a series of prospective cases, observed an incidence of 1.8% (3/158) of epidural haematomas in patients who had been administered with a combination of mechanical and chemoprophylaxis.25
We believe prophylaxis recommendations for patients undergoing spinal surgery should be perfected. There is a need for further studies with a higher level of evidence specifying types of prophylaxis by stratified group according to risk. In our centre it is general practice to emphasise mobilisation of lower limbs and early ambulation as the method of prophylaxis in patients wherever possible, with the exclusion of paraplegic patients, or those with acute spinal injuries, with multiple trauma, lower limb injuries or some type of previous ambulation disability. The low rate of VTE events in elective spinal surgery means that in a great many of cases patients could be referred for this, particularly when we take into account the comparison with the appearance of adverse effects relating to bleeding through prophylactic anticoagulation, where we have not found a single episode in 1092 cases of surgical intervention.
We believe that only prospective studies would access real figures regarding the prevalence of this problem in spinal surgery. Despite its limitations, with this study we are attempting to provide further details of the current evidence on the incidence of VTE in these patients and recognise specific risk factors which may help us to select the patients for whom a method of prophylaxis is to be administered, thus avoiding the “pendulum” effect of indicating an unnecessary method or omitting patients who should have been offered prophylaxis.
We acknowledge that clinical screening to detect VTE in our patients is one of the limitations of our study, with possible understating of the real rate of incidence. However, the realisation of other methods may lead to severe complications regarding the over-prescribing of anticoagulants. Incidence reflected in our study is in keeping with that described in studies with large data bases, and the risk factors mentioned.
With this in mind, we believe that our study is a good example of how to maintain simple, effective practices, since the majority of elective spinal surgery patients would not require more complex or costly prophylaxis than the mobilisation of lower limbs and early ambulation if possible. However, at times this is forgotten due to the faith bestowed on more costly, albeit not risk-free methods of prophylaxis. However, the appearance of thromoembolic events in our patients and the detection of risk factors, remind us of the existence of VTE in certain patient subgroups for major spinal surgery, and we must therefore assess prophylaxis methods in those patients who present with one or several of the risk factors mentioned in our study.
Level of evidenceLevel of evidence Level III.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments on humans or animals have been used in this research.
Confidentiality of dataThe authors declare that they are adhered to the protocols of their place of work regarding the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors have no conflicts of interest to declare relating to this article.
Please cite this article as: Rojas-Tomba F, Gormaz-Talavera I, Menéndez-Quintanilla IE, Moriel-Durán J, García de Quevedo-Puerta D, Villanueva-Pareja F. Incidencia y factores de riesgo de enfermedad tromboembólica venosa en cirugía mayor espinal, sin profilaxis química o mecánica. Rev Esp Cir Ortop Traumatol. 2016;60:133–140.