To assess if the Hawkins sign can predict whether or not astragalus fractures of the neck will develop avascular necrosis. It is also assessed whether the occurrence of this complication is related to the displacement of the fracture, soft tissue injury, or delay in the reduction or surgery. The results were compared with those found in the literature.
Material and methodsA retrospective study was conducted on 23 talar neck fractures recorded over a period of thirteen years. The following variables were analyzed: displacement of the fracture, soft tissue injury, delay and type of treatment, complications, observation of the Hawkins sign, and functional outcome.
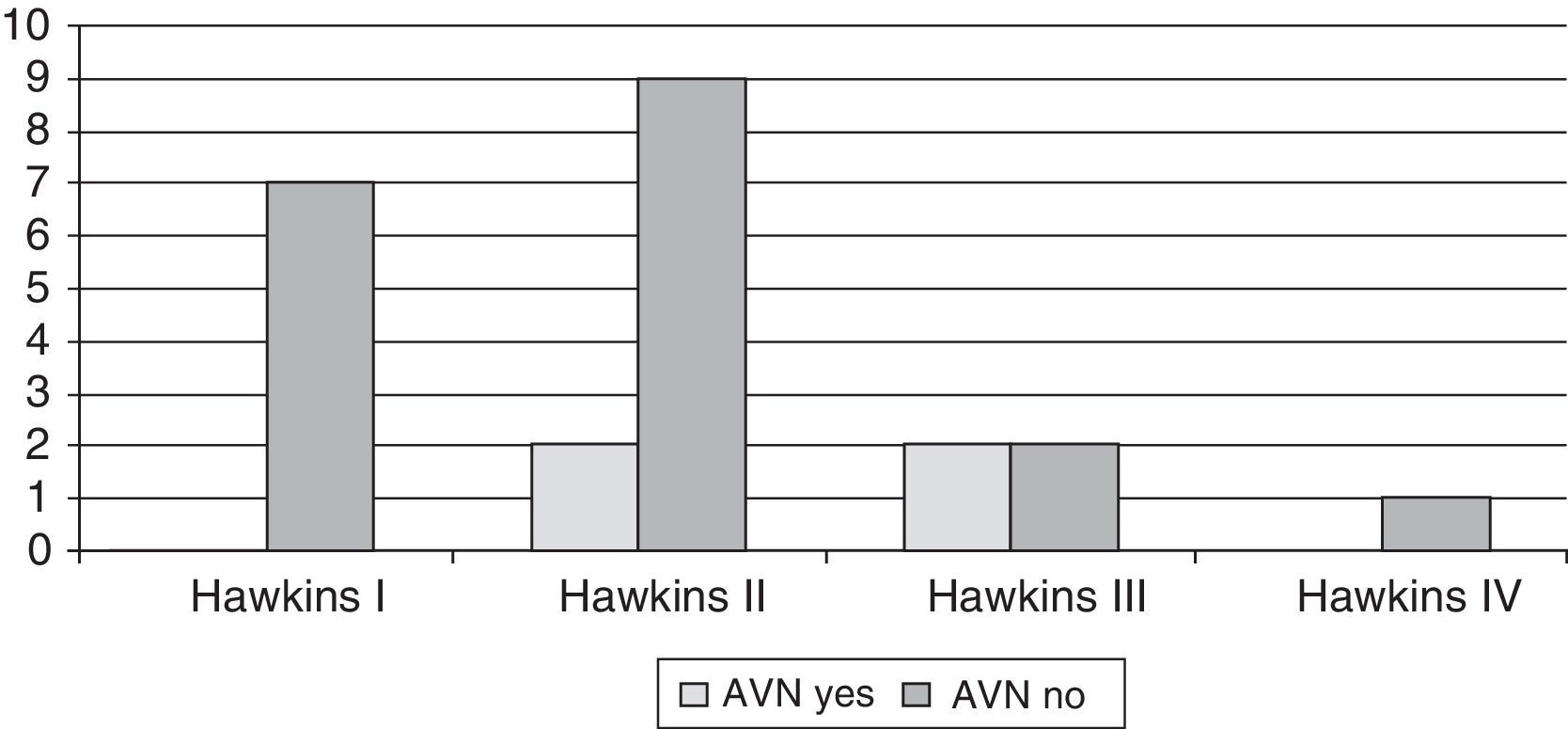
ResultsThere were 7 type I Hawkins fractures, 11 type II, and 4 type III and 1 type IV. Four cases developed avascular necrosis (2 Hawkins type II and 2 type III). Hawkins sign was observed in 12 cases, of which none developed necrosis. Four cases with negative Hawkins sign developed necrosis. No statistically significant differences were found when comparing the development of avascular necrosis with the displacement of the fracture, soft tissue injury, or delay in treatment. Differences were found when comparing the development of avascular necrosis with the Hawkins sign (P=.03).
ConclusionA positive Hawkins sign rules out that the fractured talus has developed avascular necrosis, but its absence does not confirm it.
Determinar si el signo de Hawkins predice que el astrágalo fracturado a nivel del cuello desarrollará o no una necrosis avascular (NAV), y determinar la relación con el desplazamiento de la fractura, la lesión de partes blandas, o la demora en la reducción o en la cirugía.
Material y métodosEstudio retrospectivo de 23 fracturas de cuello de astrágalo recogidas durante 13 años. Se recogen las siguientes variables: desplazamiento de la fractura, lesión de partes blandas, demora y tipo de tratamiento, complicaciones, observación del signo de Hawkins y resultado funcional.
ResultadosSe registraron 7 fracturas Hawkins tipo I, 11 tipo II, 4 tipo III y una tipo IV. Cuatro casos desarrollaron una NAV (2 Hawkins tipo II y 2 tipo III). Se observó el signo de Hawkins en 12 casos, de los cuales ninguno desarrolló necrosis. Cuatro casos con signo de Hawkins negativo desarrollaron necrosis. No se hallaron diferencias al comparar el desarrollo de NAV con el desplazamiento de la fractura, la lesión de partes blandas o la demora en el tratamiento. Sí se hallaron diferencias al comparar el desarrollo de NAV con la observación del signo de Hawkins (p=0,03).
ConclusiónEl signo de Hawkins positivo descarta que el astrágalo fracturado desarrolle una NAV, pero su ausencia no lo confirma.
Fractures of the astragalus (or talus) bone are highly uncommon lesions (0.1–0.85%).1 The peculiar anatomy of the talus, along with its distinctive vascular supply,2–5 make it a feared lesion due to the complications or sequelae that may result, especially avascular necrosis (AVN).
Hawkins6 developed a classification scale for talar neck fractures based on the existence or absence of talar body dislocation and the type of dislocation: type I for vertical fractures of the neck without displacement, type II for fractures with subluxation or dislocation of the subtalar joint and type III for fractures with subluxation or dislocation of both the subtalar and tibiotalar joints. Subsequently, Canale and Kelly7 described a fourth type for talar neck fractures associated not only to subtalar and tibiotalar dislocation, but also to talonavicular dislocation. This type of fracture also includes the only case described so far in the literature with neck fracture and dislocation, whilst maintaining the body of the astragalus in its anatomical position.8
The relevance of the classification system offered by Hawkins lies in proving that the greater the dislocation of the body of the astragalus, the greater the lesion of its vascularization and, therefore, the greater the vascular damage. Thus, in Hawkins type I fractures, the damaged vessels are only those originating from the anterolateral portion of the neck. Type II lesions also affect vessels entering through the tarsal canal and sinus. In type III, 3 blood supply sources are damaged, as in type IV, with the difference that AVN which will take place will not only affect the talar body, but also the head.6
Identifying the existence of bone necrosis is not always a simple task. Hawkins determined that between 6 and 8 weeks after the trauma it is detectable through the familiar Hawkins sign6: subchondral bone resorption in the talar dome, especially in ankle mortise and anteroposterior (AP) projections. The sign is said to be negative when it cannot be observed (Fig. 1) and positive when it can (Fig. 2). This sign indicates that the vascularization of the talus is preserved because it allows bone resorption caused by immobilization and disuse of the limb and, therefore, AVN is unlikely. However, its absence does not always imply necrosis.9
In order to reduce vascular damage, some authors advocate early reduction in talar neck fractures. However, no relationship has been found between the appearance of AVN and the time elapsed until fracture fixation. On the other hand, a relationship has been found with the level of comminution of the fracture, and with the fact of it being open or closed. This confirms that high-energy trauma lesions entail more complications and, therefore, a worse prognosis.9
Material and methodsDuring the elaboration of this work we retrospectively reviewed the medical records and complementary tests of patients with talar fractures treated at Dr. Josep Trueta University Hospital in Girona (tertiary center) over a period of 13 years, from January 1st, 1997 to December 31st, 2010. We found a total of 63 talar fractures. Of the total 31 talar neck fractures gathered, 23 were monitored (74%), representing a total of 21 patients (2 bilateral cases): 7 type I cases, 11 type II cases, 4 type III cases and the only type IV case. Follow-up had a mean duration of 23 months (range: 1 month to 11 years).
The variables collected in the study were age, gender, mechanism of injury (high- or low-energy trauma), fracture pattern (classified according to the anatomical region affected: head, neck and body of the astragalus, whilst the Hawkins6 classification was used for neck fractures, including the fourth type added by Canale and Kelly7), soft tissue involvement (closed or open fractures according to the classification by Gustilo and Anderson8), type of reduction, type of treatment, complications, observation of Hawkins sign during monitoring of talar neck fractures and functional clinical outcomes according to the Hawkins scoring system.6
We used the software packages Stata® and SPSS®. The statistical tests used were the Fischer test for 2×2 contingency tables and the Kruskal–Wallis test to compare continuous and ordinal variables. We considered as statistically significant results of P≤.05.
We evaluated the sensitivity and specificity of the Hawkins sign as a diagnostic test for the detection of AVN at 6–8 weeks of trauma.
ResultsWe collected 63 talar fractures, of which 31 affected the neck of the talus in 29 patients (2 bilateral cases).
Of these 29 patients, 90% were males (n=26). The mean age was 30 years, with a range varying from 5 to 56 years.
Except in 1 case, the mechanism of fracture was high-energy trauma: 23 traffic accidents and 6 falls.
We identified 12 Hawkins type I fractures, 13 type II, 5 type III and only 1 type IV fracture.
After analyzing 31 talar neck fractures we found 4 open fractures (12%): 2 Gustilo type II (on a non-displaced fracture of the neck and on another with subtalar dislocation) and 2 Gustilo type III fractures of the talar neck with subtalar and tibiotalar dislocation (1 IIIA case and 1 IIIB case).
After removing all type I fractures with no displacement and, therefore, not requiring reduction and 1 patient with type II talar neck fracture whose records did not indicate whether a reduction was performed or not, we obtained a total of 18 fractures which did undergo reduction. Of these, 14 were reduced in the first 48h after arrival at the emergency room, with a mean value of 2 days and a range between 0 and 17 days. In 6 cases (33.3%) reduction was closed: 4 with Hawkins type II, 1 with type III and 1 with the only type IV fracture in the series. In 12 cases (66.6%) the reduction was open, of which 2 cases underwent an unsuccessful initial attempt at closed reduction: 8 cases of Hawkins type II fracture and 4 of type III.
In reference to the treatment performed, 17 of the 31 talar neck fractures (55%) were treated surgically and the rest were treated conservatively.
When analyzing the type of treatment received, whether surgical or conservative, depending on the degree of displacement of the fracture according to the Hawkins classification, we found that 9 fractures (75%) without displacement received conservative treatment, 9 Hawkins type II fractures (69%) received surgical treatment, the 5 Hawkins type III talar neck fractures in the series all received surgical treatment, and the only case of Hawkins type IV fracture was treated conservatively.
Out of the fractures treated surgically, 11 (64%) underwent osteosynthesis with retrograde screws; in 4 (23%) cases with antegrade screws, in 1 case with Kirschner wires and in 1 case with external fixation.
All intervened Hawkins type I talar neck fractures were treated with screws (2 retrograde and 1 antegrade), as was also the case in type II (7 retrograde and 2 antegrade). In type III there was more treatment variability: osteosynthesis with retrograde screws in 2 fractures, antegrade in 1, with needles in 1 and osteotaxis in 1.
The anteromedial approach was the most commonly employed (47%), followed by the posterolateral and anterolateral (23%, respectively). Only in 1 Hawkins type II fracture did we use a combination of 2 surgical approaches, anterior and posterior.
In 3 cases, in addition to surgery we also associated malleolar osteotomy in order to achieve a correct reduction and fixation of the fracture: in 2 Hawkins type III talar neck fractures we performed osteotomy of the tibial malleolus and in 1 Hawkins type II fracture of the fibular malleolus. A further 3 cases already presented a fracture of the tibial malleolus and this facilitated the approach: 1 in a Hawkins type I fracture, 1 in a type II and 1 in a type III.
The definitive surgical intervention took place after a mean period of 3 days (range: 0–17 days).
Complications appeared in 78% of fractures. In order of highest to lowest frequency, these were: posttraumatic arthritis (11), intolerance to osteosynthesis material (7), AVN (4), problems of skin necrosis or alteration of the healing process (4), infection (2), algodystrophy (or reflex sympathetic dystrophy) (1), irritation in the fibular region (1) and neurovascular lesion (1).
Up to 48% of monitored talar neck fractures developed posttraumatic osteoarthritis: 5 cases of subtalar osteoarthritis (3 Hawkins type I fractures and 2 type II), 3 tibiotalar (1 case in a Hawkins type I fracture, 1 in a type II and 1 in a type III) and 3 with involvement of both joints (1 in a Hawkins type II fracture, 1 in a type III and 1 in the only case with type IV).
Only 1 case of subtalar osteoarthritis underwent arthrodesis. This corresponded to a type I talar neck fracture associated to a fracture of the lateral tuberosity.
Degenerative signs were not related to the displacement of the fracture (P=.667) or to the fractures being open or closed (P=.59).
We detected 4 cases (17%) of AVN: 2 in Hawkins type II fractures and 2 in type III fractures (Fig. 3). Only 1 of the 4 cases of AVN appeared in a type II open fracture.
AVN was not related to the displacement of the talar neck (P=.273) or to the fracture being open or closed (P=.562).
After eliminating the fractures without displacement, we recorded the type of reduction performed, when it was performed and whether or not AVN appeared. Out of these 16 patients, only 11 (69%) underwent open reduction, 3 of whom presented AVN, and 5 cases of closed reduction, with only 1 case of AVN. In 1 case of AVN, the reduction was performed within the first 24h after the lesion, in 2 cases within the first 48h and in 1 case the reduction was delayed for 7 days. We found no relationship between the occurrence of AVN and a delay in reduction (P=.569).
We opted for conservative treatment in 7 of the 23 cases, in which only 1 case of AVN appeared, whilst in 16 cases we applied surgical treatment, 3 of which suffered AVN. The delay in surgery was less than 24h in 1 case and less than 48h in the other 2 cases. Delay in surgery was also unrelated to the occurrence of AVN (P=0.35).
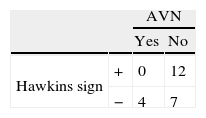
We assessed the presence or absence of Hawkins sign in the 23 patients with talar neck fracture. None of the 12 patients with positive Hawkins sign developed AVN (P=.037). The following 2×2 contingency table shows the corresponding data (Table 1).
If we assess the sensitivity and specificity of Hawkins sign as a diagnostic test for the detection of AVN following talar neck fracture, we obtain a sensitivity of 100%, a specificity of 37%, a positive predictive value of 100% and a negative predictive value of 63%.
We observed Hawkins sign in talar body fractures, but there were no cases of AVN. All cases of AVN were due to talar neck fractures.
In 1 case of type II talar neck fracture it is unknown whether the patient was maintained without load or for how long, whilst in another case the affected limb was kept without load for 8 months because the fracture was treated conservatively. In the other 2 cases of AVN in type III talar neck fractures, which were both treated surgically, the limb was maintained without load for 2 months after surgery. Full load was authorized after 3 months, once the consolidation of the fracture had been verified.
Patients were evaluated using the Hawkins Scoring System in order to assess their functional outcome. We found 9 patients with an excellent result (40%), 4 with a good result (17%), 7 with a moderate result (30%) and 3 with a poor outcome (13%).
We evaluated whether there was a relationship between the degree of displacement of the fracture and the score on the Hawkins functional scale, that is, with the functional outcome obtained by the patient at the end of the follow-up period. No statistically significant differences were found (P=.29).
DiscussionIn our review we included 63 fractured taluses (31 fractures of the neck) which occurred within a period of 13 years. After eliminating patients who were lost during nearly 2 years of follow-up, we were left with 39 taluses (23 fractures of the neck) to perform our analysis and discuss the results.
It is worth highlighting the predominance in the literature of males with a mean age in the fourth decade of life9–16 and high-energy trauma as mechanism of lesion,6,9,10,12,14–16 as was also the case in our study.
The classification system proposed by Hawkins for talar neck fractures not only allows description of fracture patterns, but also helps to guide their treatment and predict the results.6,17
Specifically analyzing the talar neck fractures included in our study, we found 12 Hawkins type I fractures, 13 type II, 5 type III and 1 type IV, which accounted for 39%, 42%, 16% and 3%, respectively.
A total of 12% presented open fractures and the 2 cases of type III Gustilo fractures occurred in Hawkins type III fractures, that is, with considerable displacement.
In 78% of cases, reduction of displaced fractures was performed within the first 48h from the initial emergency care, as recommended by various authors to alleviate soft tissue involvement and minimize the risk of further injury to talar vascularization.1,11,18,19 Two-thirds of cases required an open reduction.
Up to 55% of talar neck fractures were treated surgically, with this rate increasing alongside the degree of fracture displacement: 25% in non-displaced fractures, 69% in Hawkins type II and 100% in type III.
The anteromedial approach was also the most commonly used in our series (47%).11,12,14,16
Despite the recommendations of Trillat et al.,20 Swanson et al.21 and Ebraheim et al.,22 who maintain that osteosynthesis with antegrade screws through a posterolateral approach distributes the load better, the technical difficulty entailed by this type of treatment limits its use. Surgeons require a longer learning curve and, due to the limited number of cases available, this is not always feasible. The mean delay in surgery was approximately of 3 days (range: 0–17 days).10,23
When assessing the complications in the group of talar neck fractures, posttraumatic arthrosis was the most common complication (48%), 3 times more so than AVN, albeit with a somewhat lower incidence than that reported in the literature.7,10,19
When reviewing the literature, the reported incidence of AVN varies widely (0–67%).3,6,7,11,16,19 This is partly due to the reduced number of cases examined by numerous studies, as well as to differences in the treatment protocols of the various researchers, which have changed over the years. What is common to all studies is that the rate of AVN is related to the Hawkins classification: the greater the displacement, the greater the number of affected vessels, the more blood supply to the talus is reduced and the greater the possibility of osteonecrosis.6
We found 4 cases of AVN in 23 talar neck fractures (17%), a similar rate to that reported by other authors.12,14
Our results can be explained by considering the anastomotic network of vessels that make up the blood supply to the talus. There were no cases of AVN in type I talar neck fractures because only 1 point of the blood supply corresponding to the anterolateral side of the talus was injured. The incidence of AVN was higher (18%) in Hawkins type II fractures because 2 blood supply paths to the talus were interrupted. It is natural to find that the incidence of AVN in Hawkins type III fractures was 50%, since the 3 blood supply paths were affected. We found no cases of AVN in Hawkins type IV fractures, although we only examined 1 patient.2,4,5 We found no significant differences regarding the onset of AVN and the degree of displacement of the talar neck and being open fractures.
Although the recommendation for displaced talar neck fractures is to urgently reduce them in order to minimize the risk of necrosis, there are no studies demonstrating that urgent surgery reduces this possibility.1,9–11,17,18 We found no relationship between the delay in reduction or fixation of the fracture and the onset of osteonecrosis.
Regarding the ability of Hawkins sign to predict the onset of AVN, we did find significant differences (P=.03), with a sensitivity of 100% (0 of 4) and a specificity of 37% (7 of 19).
When comparing our results with those reported in the literature we found that we obtained a sensitivity equal to Tezval et al.,14 but lower specificity than any other author.15,23,24
The observation of Hawkins sign during patient follow-up will allow us to predict that the astragalus will not suffer necrosis. Conversely, if Hawkins sign is not observed we cannot assure that necrosis will appear, so other complementary tests, such as MRI, should be performed to confirm it.
The functional results obtained by our patients were satisfactory, since 59% of them presented a good or excellent functional outcome. These figures were similar to those reported by other studies which also used the Hawkins Scoring System for assessment.7,12,15
Schulze et al. observed that the greater the severity of the injury, the lower the score obtained, although in our study we have not observed differences between the degree of displacement and the score obtained in the functional assessment scale.12
Based on the knowledge of the precarious blood supply of the astragalus, early reduction, either by closed or open methods, should continue to be applied for displaced talar neck fractures.
Surgical treatment becomes more relevant with increasing displacement of the fracture according to the Hawkins classification, with osteosynthesis using retrograde screws by an anteromedial approach being the most common.
Positive Hawkins sign enables us to predict that a fractured talus will not develop AVN. The absence of Hawkins sign is not predictive of the onset of necrosis.
The development of AVN (prevalence of 17%) is not related to the initial displacement of the fracture, being an open or closed fracture, or to a delay in reduction or surgery.
The functional result is not related to the displacement of the fracture.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestThe authors have no conflict of interest to declare.
I wish to express my gratitude to the coauthors of this work for guiding me during these months of hard work and granting me some of their precious time.
Please cite this article as: Rodríguez-Paz S, Muñoz-Vives JM, Froufe-Siota MA. ¿Es el signo de Hawkins capaz de predecir la necrosis en las fracturas del cuello astragalino? Rev Esp Cir Ortop Traumatol. 2013;57:403–408.