Although they are frequently described in the literature, lumbar synovial cysts are a relative uncommon cause of low back and radicular leg pain.
ObjectiveTo evaluate the treatment and surgical outcomes of the lumbar synovial cysts operated on in our hospital during a 5 year period.
Material and methodsA retrospective study was conducted on patients surgically treated in our department from August 2009 to September 2014, using a visual analogue scale for the clinical follow-up in the first year after surgery.
ResultsAfter the surgical treatment (surgical removal of the synovial cyst with or without instrumented arthrodesis with transpedicular screws) of 10 patients (5 female and 5 male) with a mean age of 70.2 years (range 50–80), the clinical outcome was satisfactory in 80% of the patients, with the resolving of their symptoms.
ConclusionsLumbar synovial cysts have to be considered in the differential diagnosis in patients with low back and radicular leg pain. The majority of the patients are in their sixties and have lumbar degenerative spondylopathy. Nowadays, surgical resection of the lumbar synovial cysts and spinal fusion are the recommended treatment, because it is thought that the increased movement of the spine is one to the causes of the cyst formation. More studies are still needed, hence the relevance of this article.
Los quistes sinoviales lumbares son una causa infrecuente de dolor lumbar y radicular, aunque cada vez se describen con más frecuencia en la literatura.
ObjetivoAnalizar el tratamiento y resultados quirúrgicos de los quistes sinoviales lumbares intervenidos en nuestro centro en un período de 5 años.
Material y métodosSe realizó un estudio retrospectivo de pacientes tratados quirúrgicamente en nuestro servicio entre agosto de 2009 y septiembre de 2014, empleando la escala visual analógica para seguimiento clínico durante el año posterior a la cirugía.
ResultadosTras el tratamiento quirúrgico (exéresis del quiste con o sin artrodesis instrumentada con tornillos transpediculares), de 10 pacientes (5 mujeres y 5 varones) de edades comprendidas entre los 50 y 80 años (edad media 70,2 años), la evolución clínica fue satisfactoria en el 80% de ellos con resolución de su sintomatología.
ConclusionesLos quistes sinoviales lumbares deben ser considerados en el diagnóstico diferencial de pacientes con dolor lumbar y radicular. La mayoría de estos pacientes están en la 6.a década de la vida y presentan generalmente una espondilopatía degenerativa lumbar. En la actualidad, se recomienda la exéresis de los quistes sinoviales con artrodesis instrumentadas con tornillos transpediculares, ya que se considera que el aumento de movilidad podría ser una de las causas de su aparición; aunque todavía se necesitan más estudios al respecto, de ahí el interés de este trabajo.
Lumbar synovial cysts (LSC) appear in the zygapophyseal joint capsule of the lumbar spine. Von Gruker was the first to describe these lesions in 1880. In 1974 Kao et al.1 were the first authors to report symptomatic nerve compression secondary to a lumbar synovial cyst and called these juxtafacet cysts. Their aetiology is unknown but it is believed that the extrusion of synovial fluid by the facet joint and the progressive growth of residual myxoid degeneration could be one of the causes. Increased mobility and repetitive micro traumas may possibly be influential to their formation.1,2
The majority of LSC patients are in their sixties and generally present with lumbar degenerative spondylosis. This is less frequent in younger patients where trauma is considered to principally be a possible trigger for formation.2
The prevalence of LSC is unknown and it is probable that no uniform distribution exists in all populations (0.65–10%). They are most frequently found in the lumbar region (85–95% of cases) and in females and usually mimic the symptoms of a lumbar herniated disc, leading to lower back pain and radicular pain.3 Neurological deficit is extremely rare. In young adults and children they are rare but cases have been reported in the literature.2
Material and methodsA retrospective descriptive study was conducted on a series of 10 patients surgically treated in our LSC department, with a histologically confirmed diagnosis, between August 2009 and September 2014, both inclusive. This study was carried out in compliance with the ethical regulations of the hospital research committee. The cysts were identified by lumbar sacral spine magnetic resonance imaging (MRI).
The patients underwent surgery following the initial failure of conservative treatment, consisting of a lack of response to analgesic and rehabilitation treatment. No infiltration techniques were used on these patients due to the possible risk of bleeding. All the patients gave their informed written consent and received the same preoperative antibiotic prophylaxis in accordance with the Preventative Medicine Service protocol at the hospital. Surgical treatment comprised isolated excision of the synovial cyst with or without associated spinal instrumentation. Progressive follow-up after hospital discharge was for a minimum of a year with patients attending a consultation 3, 6, 9 and 12 months after surgery. A visual analogue scale (VAS) and control X-rays were used for all clinical follow-up.
Following identification of the cases, analysis was made of the epidemiology, clinical characteristics, imaging findings, therapeutic approach, patient evolution and any complications.
Results10 patients surgically treated for LSC at our hospital during the period mentioned above were identified. There were 5 women and 5 men with ages ranging between 50 and 80 (mean age 70.2 years).
Clinical presentation consisted of: radicular pain in 4 patients (40%), claudication in 2 (20%), Lower back pain and radicular pain in 2 (20%) and radicular pain with claudication in the other 2 (20%).
Diagnostic radiology was performed only with MRI and computerised tomography was not performed in any cases.
In 60% of cases lesion location was facet joint at L4–L5 level (4 on the right side and 2 on the left side) and in 40% of cases it was facet joint at L3–L4 level (2 on the right side and 2 on the left side).
Seven patients who presented with canal stenosis and grade I spondylolisthesis in addition to synovial cysts underwent laminectomy, synovial cyst excision and spinal fixation surgery with transpedicular screws. One of the patients underwent this secondary surgery following failure of initial surgery with isolated excision of the cyst by hemilaminectomy and facetectomy (case 5). Two patients underwent hemilaminectomy and excision of the synovial cyst, respecting the facets and one patient, the oldest in our series (case 4), who in addition to the cyst also presented with canal stenosis underwent laminectomy at this level with cyst excision but without instrumented arthrodesis in this case.
In the 7 patients who required arthrodesis with transpedicular screws, the screws were guided by nauronavigation and intraoperative computerised tomography. Of the 40 implanted screws, one of them was intraoperatively reinserted owing to an initial malposition (case 8), which led to an error percentage of 2.5%. There were no intraoperative complications in the other patients. Three patients underwent spine fusion instrumentation at level one; two patients at level two and the other two patients at level three.
Intraoperatively yellowish-brownish well defined extradural masses were distinguished which were the continuation of the facet joint along its medial surface and filled with a clear or xanthochromic liquid (except in case 8 which contained haematic matter).
In all patients the diagnosis of synovial cyst was confirmed by pathological anatomy which revealed the presence of conjunctive tissue lesions with calcium deposits, areas of haemorrhaging and fibrosis with granulation tissue lined by a thick wall of a specialised synovial epithelium.
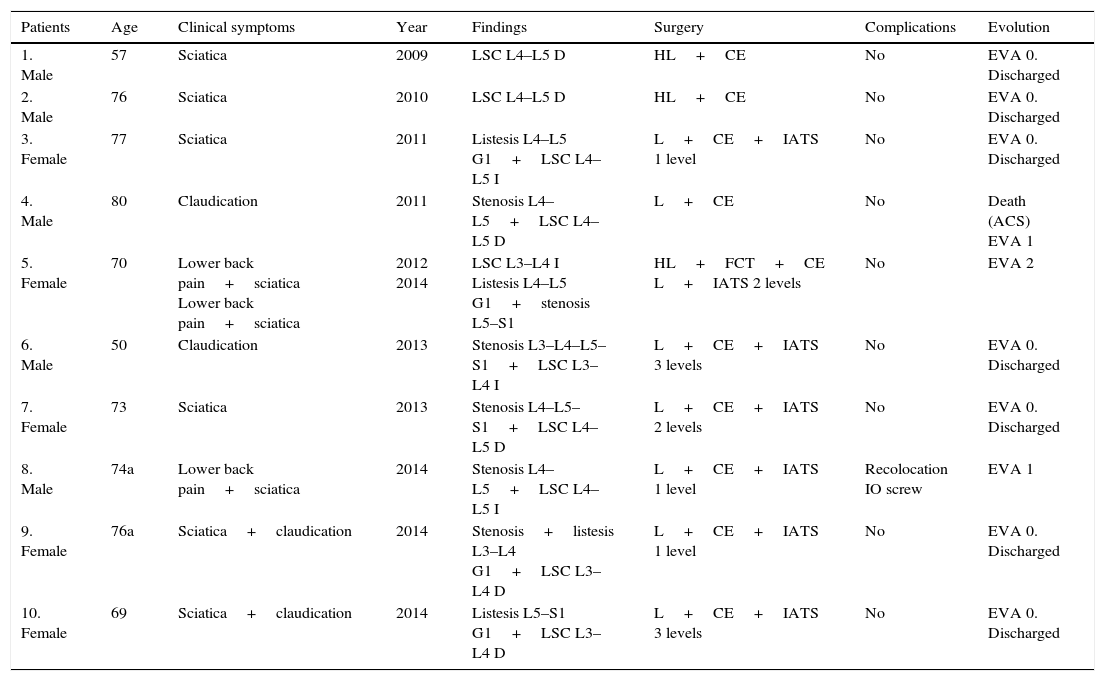
The minimum follow-up of all patients was one year. 80% of patients experienced relief of previous symptoms and a lowering of at least 6 points in the VAS. Seven patients are currently discharged from hospital, and one patient died a year and a half after surgery from an acute coronary syndrome which was not associated with surgical intervention (case 4). Another two patients continue to present with mild mechanical lower back pain (VAS 1–2) which is relieved with analgesics (case 5 and 8). None of the 3 patients who did not undergo spinal instrumentation have showed any signs of clinical instability in follow-up to date or recurrence of synovial cysts (Table 1).
Our series of 10 cases.
| Patients | Age | Clinical symptoms | Year | Findings | Surgery | Complications | Evolution |
|---|---|---|---|---|---|---|---|
| 1. Male | 57 | Sciatica | 2009 | LSC L4–L5 D | HL+CE | No | EVA 0. Discharged |
| 2. Male | 76 | Sciatica | 2010 | LSC L4–L5 D | HL+CE | No | EVA 0. Discharged |
| 3. Female | 77 | Sciatica | 2011 | Listesis L4–L5 G1+LSC L4–L5 I | L+CE+IATS 1 level | No | EVA 0. Discharged |
| 4. Male | 80 | Claudication | 2011 | Stenosis L4–L5+LSC L4–L5 D | L+CE | No | Death (ACS) EVA 1 |
| 5. Female | 70 | Lower back pain+sciatica Lower back pain+sciatica | 2012 2014 | LSC L3–L4 I Listesis L4–L5 G1+stenosis L5–S1 | HL+FCT+CE L+IATS 2 levels | No | EVA 2 |
| 6. Male | 50 | Claudication | 2013 | Stenosis L3–L4–L5–S1+LSC L3–L4 I | L+CE+IATS 3 levels | No | EVA 0. Discharged |
| 7. Female | 73 | Sciatica | 2013 | Stenosis L4–L5–S1+LSC L4–L5 D | L+CE+IATS 2 levels | No | EVA 0. Discharged |
| 8. Male | 74a | Lower back pain+sciatica | 2014 | Stenosis L4–L5+LSC L4–L5 I | L+CE+IATS 1 level | Recolocation IO screw | EVA 1 |
| 9. Female | 76a | Sciatica+claudication | 2014 | Stenosis+listesis L3–L4 G1+LSC L3–L4 D | L+CE+IATS 1 level | No | EVA 0. Discharged |
| 10. Female | 69 | Sciatica+claudication | 2014 | Listesis L5–S1 G1+LSC L3–L4 D | L+CE+IATS 3 levels | No | EVA 0. Discharged |
IATS: instrumented arthrodesis with transpedicular screws; R: right; CE: cyst excision; FCT: facetectomy; G1: grade 1; HL: hemilaminectomy; L: left; IO: intraoperative; L: laminectomy; LSC: lumbar synovial cysts; ACS: acute coronary syndrome.
LSCs are an uncommon cause of lumbar and radicular pain, although they are described in the literature with increasing frequency. Synovial cysts may appear at vertebral level but most frequently occur in the joints of the extremities. In the spine they are located at extradural level in the continuation of the degenerated facet joint along its medial surface, generally in the L4–L5 space (as in 60% of our cases), this being the most mobile section of the spine and the one most associated with spondylolisthesis and osteoarthritis, leading to instability and facet arthrosis which plays an essential role in the formation of the above-mentioned cysts.2–4 L4–L5 level is the most affected space, followed by L5–S1, L3–L4, and L2–L3 (unlike our series in which the second level most affected was L3–L4).
Their pathogenesis is widely debated although it is generally accepted that they forms part of the degenerative spinal process, where spinal instability and trauma are significant.3–6 The definitive association of these cysts with osteoarthritis (40.5%), spondylolisthesis (43.4%), and disc degeneration (13.2%) highlights their degenerative nature.3–5
LSC are in fact local instability markers of the functional spinal unit, and therefore their expansion or regression is closely linked to local physiological factors such as vascularisation of the synovial fluid of the joint, the possibility of intracystic haemorrhages and the degree of local inflammation of the facet. The disruption of a facet increases instability of the functional spinal unit and increases the biomechanical stress of the contralateral facet joint which accelerates its degeneration.4–6
Microscopically synovial cysts contain xanthochromic or clear fluid, are enclosed by the spinal epithelium which is pseudostratified around a fibrous grainy tissue with myxoid changes and presents a demonstrable communication with the joint capsule.6–10
The most frequent symptom is lower back or radicular pain (55–97%), as occurred in our cases, although neurogenic claudication and cauda equine syndrome may also present. This is usually a case of a progressive lower back pain or long term claudication with or without associated radiculopathy, which may, on occasions present in a more acute or sub acute manner if associated with intracystic haemorrhaging of the lesion (as in case 8).
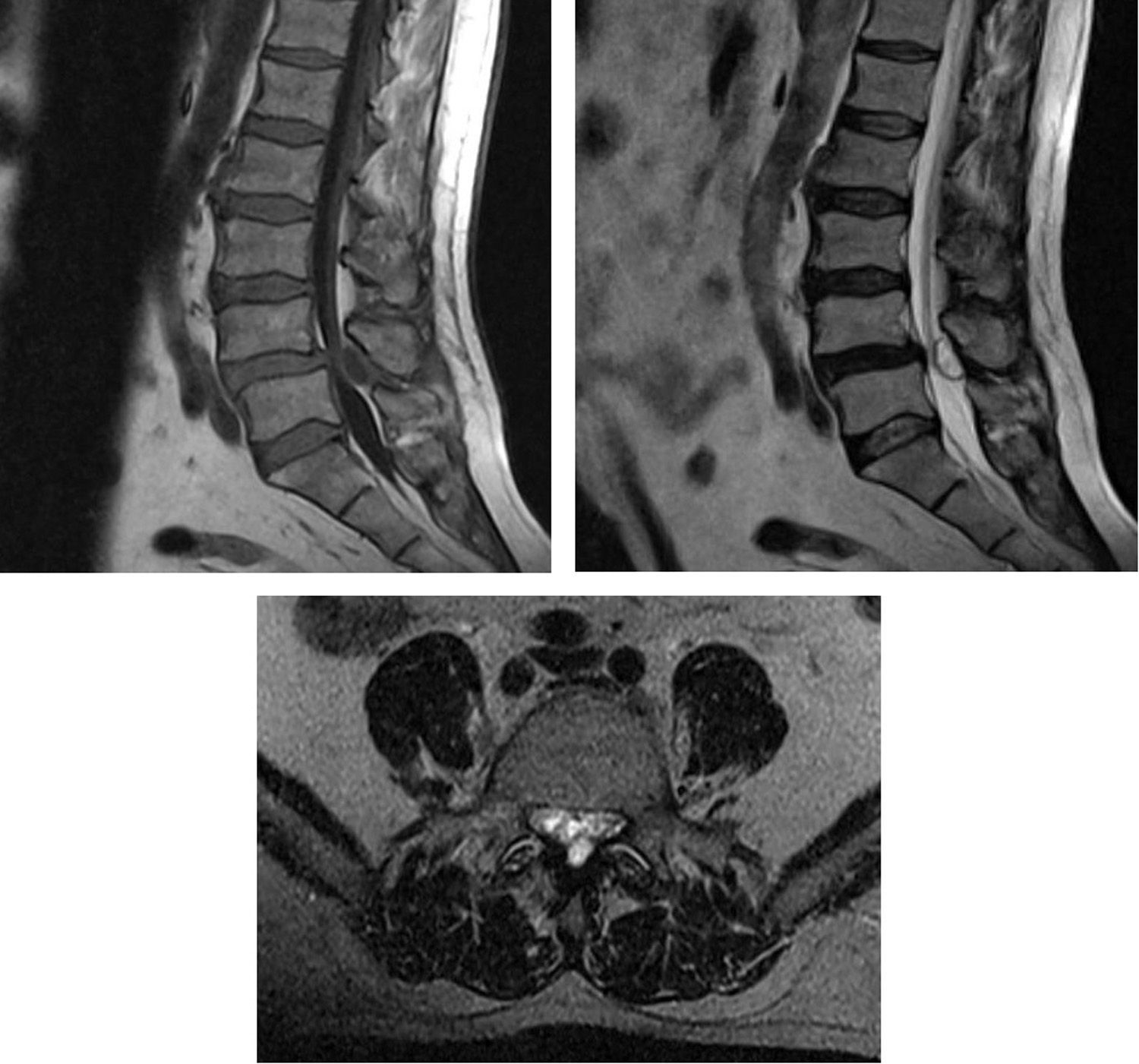
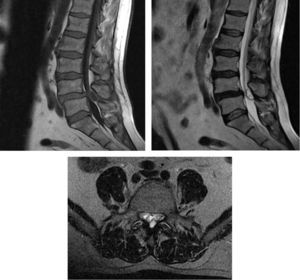
MRI is the technique of choice for diagnosis, since it reveals the cystic nature of the lesion. Intermediate signal intensity of extradural masses extending along the medial side of the facet joint which compress the dural sac are observed.3,6,11–14 These are well defined epidural masses, which are normally T1 isointense and T2 hyperintense or isointense, although intensity may vary depending on the protein content, previous haemorrhage and/or calcification. Fig. 1 – T2 sagittal (isointense) and T1 axial (isointense) of right LSC L4–L5 (case 7) – and Fig. 2 – T1 sagittal (isointense), and T2 sagittal and axial sagittal (hypertense, haematic material) of left LSC L4-L5 (case 8). Anticoagulant treatment, trauma, herniated disc, vascular anomalies, and neogangiogenesis in the synovial coating of the cyst are risk factors for intracystic haemorrhaging.15The presence of gas on the inside of the cyst may be a pathognomonic event.6
Differential diagnosis with other juxtafacet cysts (ganglion cysts, yellow ligament cysts and posterior longitudinal ligament cysts) is important because it conditions the type of surgery and approach used.6–9,12,16 Non synovial cysts are not in direct contact with the zygoapophysary joint and there is an absence of a specialised epithelial coating resulting in no major degenerative changes being provoked in the biomechanics of the so-called functional spinal unit. A contra-lateral approach may therefore be used without the need for surgical resection of the adjacent facet.8,9 On the contrary, true synovial cysts are the last phase of joint degeneration and there is therefore a much higher risk of instability and a tendency for a more aggressive approach in fusion, particularly data regarding associated degenerative changes (disc collapse, listesis) and lumbar pain (not only radicular) are present. In addition to the differential diagnosis with other juxtafacet cysts, infections and tumours such as neurofibroma, schwannoma or metastasis6,8,9 must be ruled out with the use of erythrocyte sedimentation rate and reactive protein C studies.
When these cysts do not respond to conservative treatment, there is great controversy regarding the best surgical approach. A surgical approach may range from simple excision of the synovial cyst with hemi or laminectomy, to minimally invasive techniques or even synovial cyst removal with associated instrumentation.
The advantage of open surgery is that it provides extensive and appropriate exposure of the cysts and areas of attachment, leading to macroscopic confirmation for excision (Fig. 3) – intraoperative image of synovial cyst right L3–L4 (case 9). Its disadvantage is that it presents the need to carry out medial facetectomy which when combined with an already degenerated spine, increases the risk of instability, with the dilemma of whether to use transpedicular screws for attachment or not.
Minimally invasive spine surgery with tubular retractors for access was described by Foley et al.17 in 1997. The paramedian ipsilateral lumbar spine approach has minimised incision, reduced blood loss, and decreased postoperative pain, but there is still the need for surgical resection of the medial facet and thus potentially accelerating the risk of degeneration and possibility of recurrence of the synovial cyst or segmental instability.8,9,12,15 In the light of this, the minimally invasive contralateral approach has been described, using a contralateral hemilaminectomy with preservation of the degenerated facet, to prevent possible future instability of the joint complex and recurrence of the cyst (1.3%-10.8%) and the need for spine fusion. The problem with this technique is that it is more demanding from a surgical point of view, with a higher risk of incidental durotomy, epidural haematoy and cerebrospinal fluid leakage.8,9,11–13,15,16
Laminectomy with instrumented fusion demands a more aggressive approach, associated with greater blood loss, higher neurological risk and long term risk of disease of the adjacent disc presenting. However, in a retrospective study of 39 cases, Khan et al. concluded that the patients who undergo spinal instrumentation with laminectomy would tend to have better results in scales of clinical improvement if they were compared with those who had simply undergone spinal decompression surgery.10 Notwithstanding, in our case 4, despite having carried out a excision of synovial cyst and a laminectomy, we did not carry out instrumented arthrodesis, due to greater aggressiveness and longer time in surgery, which would have increased the surgical risk of a patient aged 80.
The recurrence of synovial cysts after surgery varied between 1.3% and 10.8%. The risk of post surgical instability after isolated decompression is low but may support the adjuvant arthrodesis approach, generally when facetectomy is carried out or when there is proof of preoperative instability.3,6,8,12,15,18–20
This review has several limitations: firstly there were only 10 cases in the series and secondly a long term follow-up was required to reach relevant conclusions. However, we believe that in young patients where it is presupposed that trauma is the trigger of the cyst and there are no instability data we should firstly implement a more conservative approach with simple excision of the cyst and close monitoring with dynamic radiographs to detect instability data if they appear. In older patients where instability of the degenerated spine is the actual cause of the LSC and where their physical condition allows it, we consider that an excision of the cyst would be better indicated, together with an associated spinal instrumentation.
ConclusionsLSCs are a rare pathology, but responsible for lower back and radicular pain, especially in patients of advanced age, although they may exceptionally present in young people (<40). They are degenerative lesions of juxtafacet location. MRI is the diagnostic technique of choice.
Surgical resection should be considered a treatment option in patients who do not respond to conservative treatment. Unfortunately, the surgical approach to be followed continues presently to be under debate. We believe that the possibility of using spinal instrumentation should be considered to prevent spinal instability and recurrence of the cyst, personalising each case (size of cyst, age and patient circumstances, compromise of neighbouring structures, lumbar and/or radicular pain, degree of preoperative listesis and degeneration of facet joint). After excision of a synovial cyst where partial facetectomy is required there is the possibility in the future of requiring a spinal fusion and for this reason these patients must be closely monitor for any possible appearance of clinical instability.
Level of evidenceLevel of evidence II.
Ethical disclosuresProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors declare no patient data appears in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Lista-Martínez O, Moreno-Barrueco VM, Castro-Castro J, Varela-Rois P, Pastor-Zapata A. Quistes sinoviales lumbares: presentación de una serie de 10 casos y revisión de la literatura. Rev Esp Cir Ortop Traumatol. 2017;61:28–34.