To report the outcomes of surgical treatment of lower limb fractures in patients with chronic spinal cord injuries.
Material and methodA total of 37 lower limb fractures were treated from 2003 to 2010, of which 25 fractures were treated surgically and 12 orthopaedically.
ResultsPatients of the surgical group had better clinical results, range of motion, bone consolidation, and less pressure ulcers and radiological misalignment. No differences were detected between groups in terms of pain, hospital stay, and medical complications.
DiscussionThere is no currently consensus regarding the management of lower limb fractures in patients with chronic spinal cord injuries, but the trend has been conservative treatment due to the high rate of complications in surgical treatment.
ConclusionsChronic spinal cord injuries patients with lower limb fractures who are treated surgically achieved a more reliable consolidation, practically a free range of motion, low rate of cutaneous complications, and pain associated with the fracture. This allows a quick return to the previous standard of living, and should be considered as an alternative to orthopaedic treatment in these patients.
Conocer los resultados del tratamiento quirúrgico de las fracturas de extremidad inferior en los pacientes con lesiones medulares crónicas.
Material y métodoEntre el 2003-2012 se trataron 37 fracturas de extremidad inferior, divididas en 2 grupos según su tratamiento, 25 en el grupo quirúrgico y 12 en el grupo conservador.
ResultadosEl grupo quirúrgico presentó mejores resultados en cuanto a balance articular, consolidación ósea, alineación radiológica y menor número de úlceras por presión. No se detectaron diferencias entre grupos en cuanto a estancia hospitalaria, número de complicaciones médicas y control del dolor.
DiscusiónActualmente no hay consenso respecto al manejo de las fracturas de extremidad inferior en lesionados medulares crónicos, pero la tendencia ha sido el tratamiento conservador escudándose en la alta tasa de complicaciones del tratamiento quirúrgico.
ConclusionesEn fracturas de extremidad inferior en lesionados medulares crónicos, la estabilización quirúrgica presenta mejores resultados de consolidación ósea, un balance articular prácticamente libre, una baja tasa de complicaciones cutáneas y dolor asociado a la fractura. Todo ello permite un rápido retorno al nivel previo de la lesión, por lo que se debe tener en cuenta como alternativa al tratamiento conservador.
Bone density decreases in patients with chronic spinal cord injuries (cSCI) due to the absence of neurological and load stimuli.1–4 However, this observation is yet to be quantified in paraplegic and tetraplegic patients with associated fractures.5 There is currently no consensus on the best therapeutic strategy for these types of fractures.6–14 In lower limb fractures (LLF) occurring simultaneously with an acute spinal cord injury, internal fixation is preferred.12,15–20 By contrast, conservative treatment is preferred for cases of LLF in patients with chronic paraplegia or tetraplegia.7,8,11,17 However, this tendency has been a matter of debate in recent years.19–24
In our unit, a spinal cord injury reference centre in Spain, therapeutic decision making has been made difficult by a lack of scientific evidence, and is based on the experience of our surgical team. The aim of this article is to establish the outcomes of surgical treatment for lower limb fractures in cSCI. Our working hypothesis is that surgical treatment of LLI is better than nonsurgical treatment, and our null hypothesis is that both treatments achieve similar outcomes.
Material and methodA retrospective analysis between 2003 and 2012 that recorded 37 LLF in 25 patients with cSCI (6 tetraplegias and 19 paraplegias). The fractures included occurred at least two years after the spinal cord injury, based on the definition of cSCI by de Bruin et al.25 Acetabular, head-neck and tarsus fractures were excluded, rejecting fractures that were treated principally conservatively in our centre, or fractures that involved treatment by arthroscopy; in this way the groups to be analysed were homogenised. Minimum follow-up was 36 months.
The fractures were classified by injury mechanism according to McMaster and Staufer's17 system and by site, line and comminution according to the AO-ASIF system.26
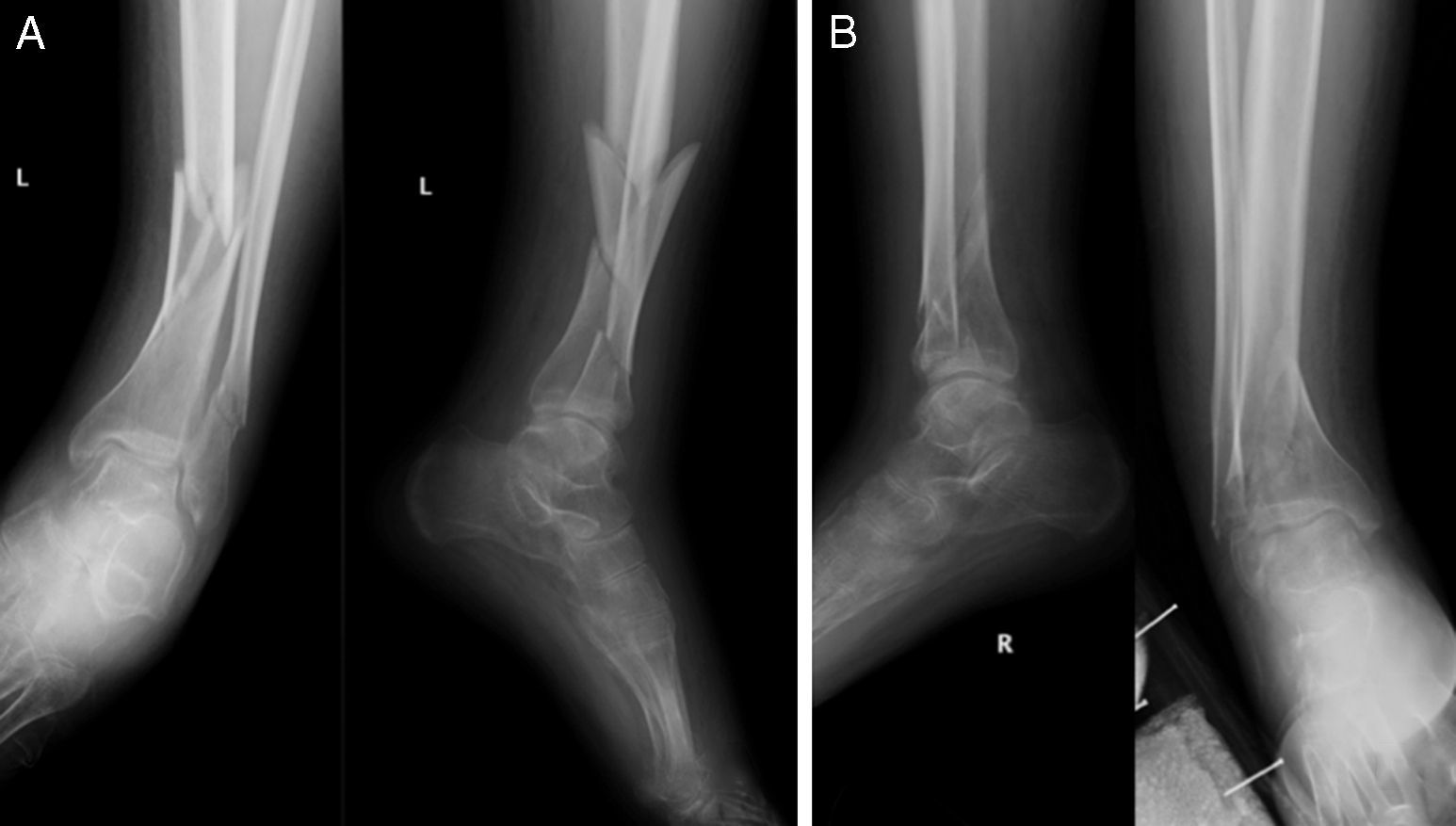
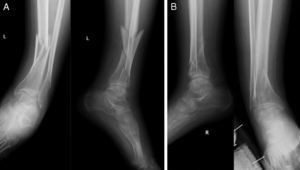
The fractures were divided into 2 groups, according to the therapeutic option for their treatment. The conservative group (C) comprised 12 fractures (4 femoral diaphyses, one femoral supracondylar, 2 proximal tibias, 2 tibial diaphyses and 3 tibial pylons) treated conservatively with plaster. The surgical group (Q) comprised 25 fractures treated surgically, because they presented displaced fractures (Figs. 1 and 2). The 25 fractures of group Q were 5 proximal femoral fractures, treated by intramedullary nail, 6 diaphyseal fractures stabilised by intramedullary nail (3 anterograde and 2 retrograde), 6 supracondylar fractures treated with retrograde intramedullary nail, 4 proximal tibial fractures treated with locking plates and screws, 3 diaphyseal tibial fractures synthesised by anterograde intramedullary nail (Fig. 3A), and one distal tibial stabilised by locking plates and screws (Fig. 3B).
The physiotherapy exercises prescribed for groups C and Q included daily exercises to preserve the functionality of the adjacent joints. Pressure ulcer prevention (PUP) and urinary and intestinal evacuation were ensured following our centre's cSCI protocols.
The criteria of Mize et al.27 were used to evaluate clinical outcomes. Measurements of articular balance and visual analogue scale (VAS) score for pain were undertaken at 3 and 6 months after the fracture. The degree of autonomy and level of satisfaction were also noted. The radiological analysis was based on conventional radiology (X-ray) and CAT, following the criteria developed by Schmeiser et al.20
The statistical analysis of the articular and radiological balance was performed by 2×2 contingency tables using Fisher's exact test, based on 4 outcomes (very good, good, satisfactory and poor) grouping the comparisons between groups Q and C into very good/good vs satisfactory/poor.
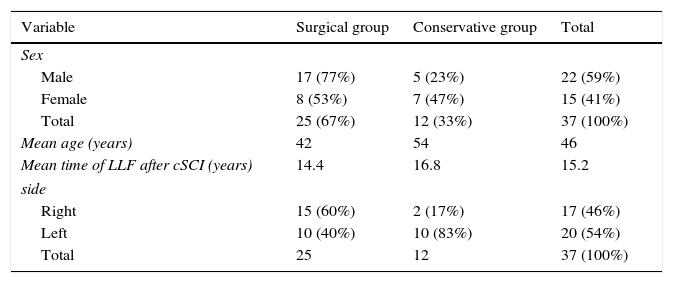
ResultsEpidemiology: the epidemiological data of both groups Q and C are described in Table 1.
Patient distribution.
| Variable | Surgical group | Conservative group | Total |
|---|---|---|---|
| Sex | |||
| Male | 17 (77%) | 5 (23%) | 22 (59%) |
| Female | 8 (53%) | 7 (47%) | 15 (41%) |
| Total | 25 (67%) | 12 (33%) | 37 (100%) |
| Mean age (years) | 42 | 54 | 46 |
| Mean time of LLF after cSCI (years) | 14.4 | 16.8 | 15.2 |
| side | |||
| Right | 15 (60%) | 2 (17%) | 17 (46%) |
| Left | 10 (40%) | 10 (83%) | 20 (54%) |
| Total | 25 | 12 | 37 (100%) |
LLF: lower limb fractures; cSCI: chronic spinal cord injury.
Twenty-one of the 25 patients had a full spinal cord injury. The majority presented muscular spasticity due to neuronal inhibition at spinal cord level. The initial spinal cord injury was caused by a road accident in 21 patients and an accident at work in 3 patients. The fractures were the result of minor trauma (during transfer manoeuvres) in 29 cases, wheelchair falls in 6 cases and road accidents in 2. Of the 37 fractures, 35 were classified as group II according to McMaster and Staufer's17 system and the remainder as group III. The patients were followed up for a mean 47 months (range 36–91). Most of the fractures occurred around the knee (Table 2).
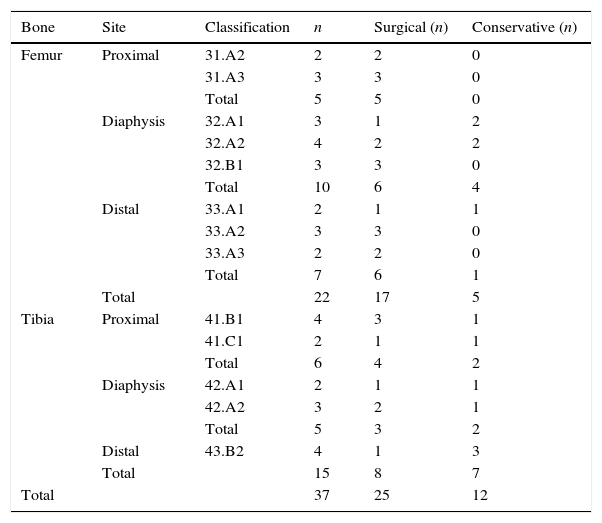
Classification of fractures (n=37).
| Bone | Site | Classification | n | Surgical (n) | Conservative (n) |
|---|---|---|---|---|---|
| Femur | Proximal | 31.A2 | 2 | 2 | 0 |
| 31.A3 | 3 | 3 | 0 | ||
| Total | 5 | 5 | 0 | ||
| Diaphysis | 32.A1 | 3 | 1 | 2 | |
| 32.A2 | 4 | 2 | 2 | ||
| 32.B1 | 3 | 3 | 0 | ||
| Total | 10 | 6 | 4 | ||
| Distal | 33.A1 | 2 | 1 | 1 | |
| 33.A2 | 3 | 3 | 0 | ||
| 33.A3 | 2 | 2 | 0 | ||
| Total | 7 | 6 | 1 | ||
| Total | 22 | 17 | 5 | ||
| Tibia | Proximal | 41.B1 | 4 | 3 | 1 |
| 41.C1 | 2 | 1 | 1 | ||
| Total | 6 | 4 | 2 | ||
| Diaphysis | 42.A1 | 2 | 1 | 1 | |
| 42.A2 | 3 | 2 | 1 | ||
| Total | 5 | 3 | 2 | ||
| Distal | 43.B2 | 4 | 1 | 3 | |
| Total | 15 | 8 | 7 | ||
| Total | 37 | 25 | 12 |
Hospital stay: this was a mean of 18 days (range 7–33) for group Q and 18 days (range 0–60) for group C. No significant differences were found between the groups (p>0.05).
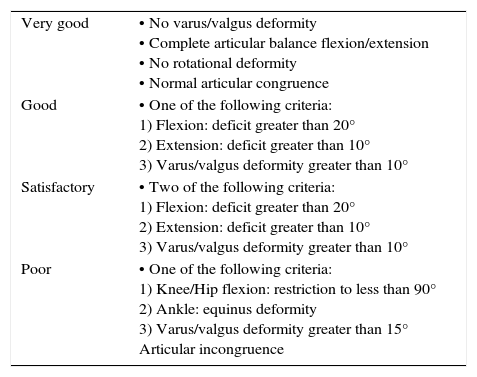
Clinical examination: the results were analysed using the criterion of Mize et al.27 (Table 3). No loss of functionality affecting daily activities was found in group Q. Neither did we find any shortening of the limb greater than 1cm, no varus/valgus deformity or recurvatum/antecurvatum that would hinder sitting or wheel chair use. In group C, the four patients with documented non union (33% of the patients), had reduced quality of life due to pain and autonomic dysreflexia (AD).
Clinical criteria for evaluating lower limb fracture healing in patients with chronic spinal cord injury.
| Very good | • No varus/valgus deformity • Complete articular balance flexion/extension • No rotational deformity • Normal articular congruence |
| Good | • One of the following criteria: 1) Flexion: deficit greater than 20° 2) Extension: deficit greater than 10° 3) Varus/valgus deformity greater than 10° |
| Satisfactory | • Two of the following criteria: 1) Flexion: deficit greater than 20° 2) Extension: deficit greater than 10° 3) Varus/valgus deformity greater than 10° |
| Poor | • One of the following criteria: 1) Knee/Hip flexion: restriction to less than 90° 2) Ankle: equinus deformity 3) Varus/valgus deformity greater than 15° Articular incongruence |
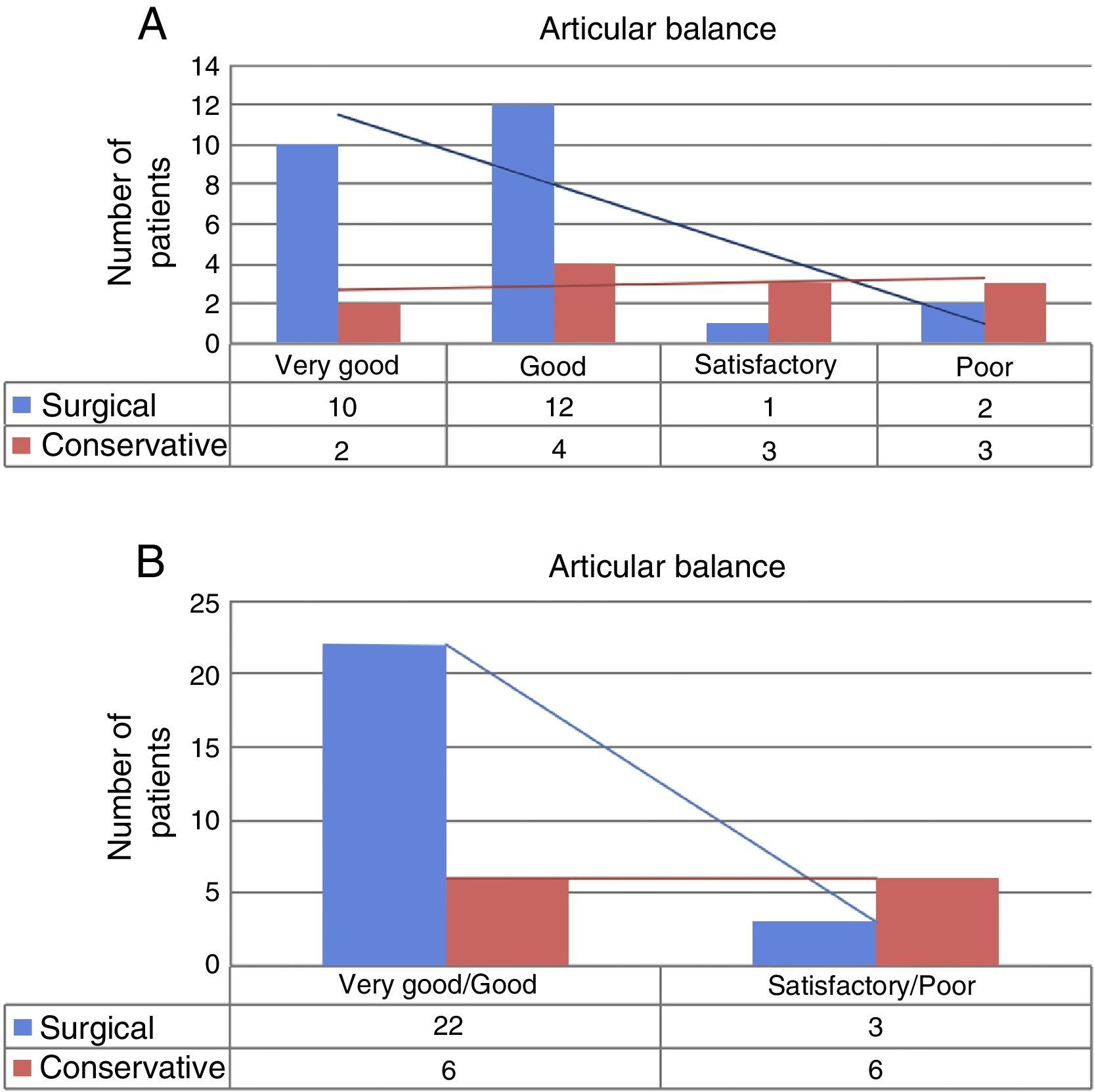
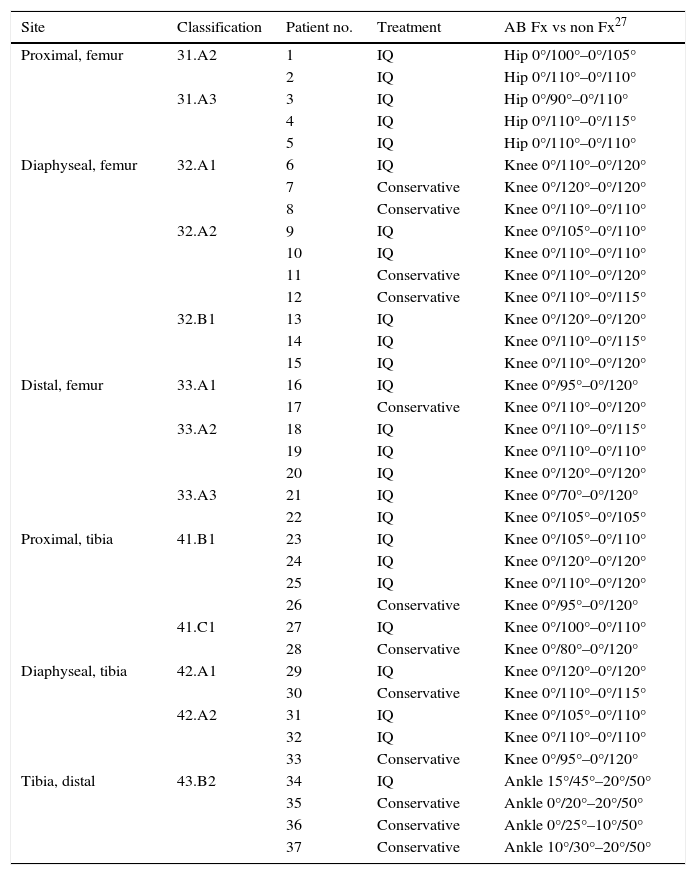
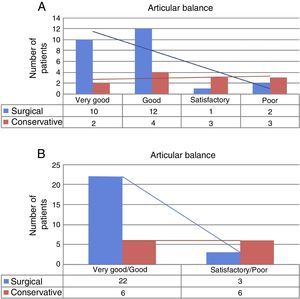
Range of motion: the range of motion data of both the surgical (Q) and the conservative (C) groups are shown in Table 4 and Fig. 4A and B. The statistical analysis found statistical differences in favour of group Q (p=0.035).
Articular balance on follow-up of fractured limb vs non-fractured limb (contralateral).
| Site | Classification | Patient no. | Treatment | AB Fx vs non Fx27 |
|---|---|---|---|---|
| Proximal, femur | 31.A2 | 1 | IQ | Hip 0°/100°–0°/105° |
| 2 | IQ | Hip 0°/110°–0°/110° | ||
| 31.A3 | 3 | IQ | Hip 0°/90°–0°/110° | |
| 4 | IQ | Hip 0°/110°–0°/115° | ||
| 5 | IQ | Hip 0°/110°–0°/110° | ||
| Diaphyseal, femur | 32.A1 | 6 | IQ | Knee 0°/110°–0°/120° |
| 7 | Conservative | Knee 0°/120°–0°/120° | ||
| 8 | Conservative | Knee 0°/110°–0°/110° | ||
| 32.A2 | 9 | IQ | Knee 0°/105°–0°/110° | |
| 10 | IQ | Knee 0°/110°–0°/110° | ||
| 11 | Conservative | Knee 0°/110°–0°/120° | ||
| 12 | Conservative | Knee 0°/110°–0°/115° | ||
| 32.B1 | 13 | IQ | Knee 0°/120°–0°/120° | |
| 14 | IQ | Knee 0°/110°–0°/115° | ||
| 15 | IQ | Knee 0°/110°–0°/120° | ||
| Distal, femur | 33.A1 | 16 | IQ | Knee 0°/95°–0°/120° |
| 17 | Conservative | Knee 0°/110°–0°/120° | ||
| 33.A2 | 18 | IQ | Knee 0°/110°–0°/115° | |
| 19 | IQ | Knee 0°/110°–0°/110° | ||
| 20 | IQ | Knee 0°/120°–0°/120° | ||
| 33.A3 | 21 | IQ | Knee 0°/70°–0°/120° | |
| 22 | IQ | Knee 0°/105°–0°/105° | ||
| Proximal, tibia | 41.B1 | 23 | IQ | Knee 0°/105°–0°/110° |
| 24 | IQ | Knee 0°/120°–0°/120° | ||
| 25 | IQ | Knee 0°/110°–0°/120° | ||
| 26 | Conservative | Knee 0°/95°–0°/120° | ||
| 41.C1 | 27 | IQ | Knee 0°/100°–0°/110° | |
| 28 | Conservative | Knee 0°/80°–0°/120° | ||
| Diaphyseal, tibia | 42.A1 | 29 | IQ | Knee 0°/120°–0°/120° |
| 30 | Conservative | Knee 0°/110°–0°/115° | ||
| 42.A2 | 31 | IQ | Knee 0°/105°–0°/110° | |
| 32 | IQ | Knee 0°/110°–0°/110° | ||
| 33 | Conservative | Knee 0°/95°–0°/120° | ||
| Tibia, distal | 43.B2 | 34 | IQ | Ankle 15°/45°–20°/50° |
| 35 | Conservative | Ankle 0°/20°–20°/50° | ||
| 36 | Conservative | Ankle 0°/25°–10°/50° | ||
| 37 | Conservative | Ankle 10°/30°–20°/50° |
AB: articular balance; Fx: fracture; IQ: surgical intervention.
Comparison of articular balance between the surgical group (Q) and the conservative group (C). In (A), comparison table classifying the balance into four grades: very good, good, satisfactory and poor. In (B), 2×2 table, grouping into two categories according to good or poor outcome.
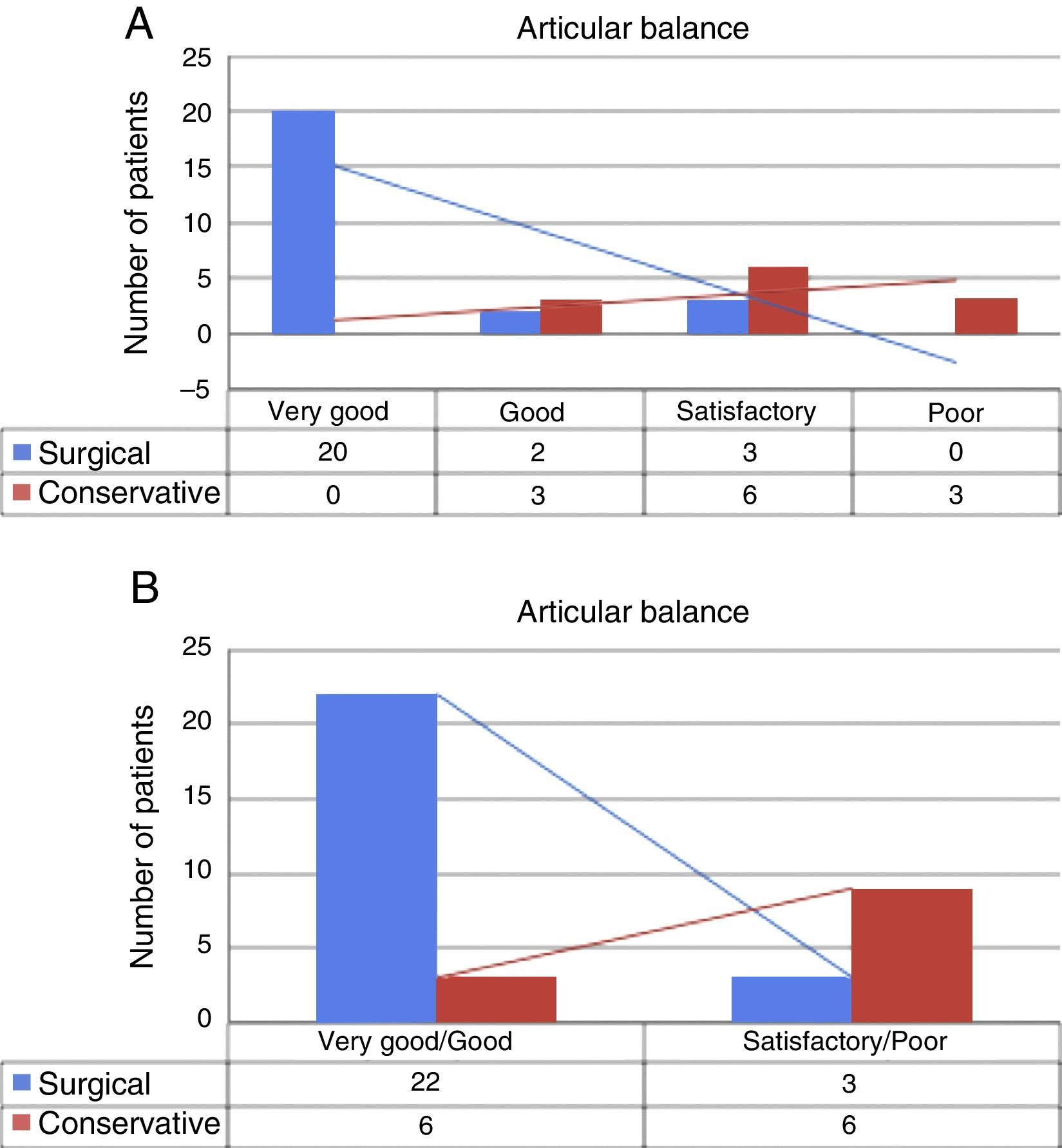
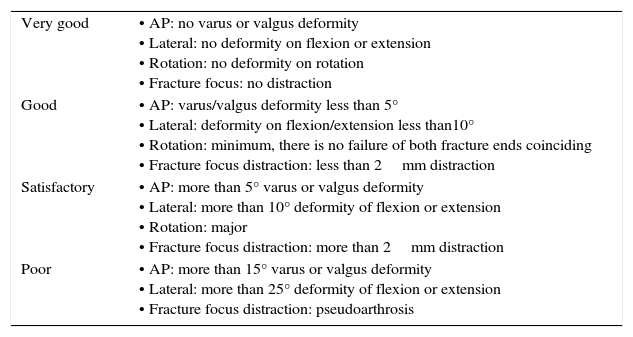
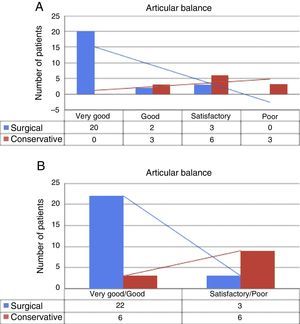
Radiological results: the results were analysed using the criteria developed by Schmeiser et al.20 (Table 5). The radiological alignment data of both groups Q and C are described in Table 6 and Fig. 5A and B. With regard to healing, at the last radiological follow-up at 48 months, solid union of all the fractures was found in group Q, with a mean union at 14.5 weeks. In group C, at the last radiological follow-up, undertaken on average at 34.9 months, 4 of the 12 patients (33.3%)had no union and 2 had delayed union (21 weeks). The remainder of the fractures had good union, achieved at a mean of 15.9 weeks. A CAT scan was required between 3 and 6 months postoperatively in 83% of the patients. The statistical analysis found significant differences in favour of group Q (p<0.05) in terms of radiological union and radiological alignment.
Radiological criteria for evaluating LLF in cSCI patients.
| Very good | • AP: no varus or valgus deformity • Lateral: no deformity on flexion or extension • Rotation: no deformity on rotation • Fracture focus: no distraction |
| Good | • AP: varus/valgus deformity less than 5° • Lateral: deformity on flexion/extension less than10° • Rotation: minimum, there is no failure of both fracture ends coinciding • Fracture focus distraction: less than 2mm distraction |
| Satisfactory | • AP: more than 5° varus or valgus deformity • Lateral: more than 10° deformity of flexion or extension • Rotation: major • Fracture focus distraction: more than 2mm distraction |
| Poor | • AP: more than 15° varus or valgus deformity • Lateral: more than 25° deformity of flexion or extension • Fracture focus distraction: pseudoarthrosis |
AP: antero-posterior; LLF: lower limb fracture; cSCI: chronic spinal cord injury.
Radiological results.
| Group | Fracture | Coronal axis | Sagittal axis | AP translation | Lateral translation | Distraction | Rotation |
|---|---|---|---|---|---|---|---|
| Surgical | 31.A2 | 10° valgus | 0° | 0mm | 0mm | 0mm | 0° |
| Surgical | 31.A2 | 0° | 0° | 0mm | 0mm | 0mm | 0° |
| Surgical | 31.A3 | 0° | 0° | 0mm | 2mm | 0mm | 0° |
| Surgical | 31.A3 | 5° valgus | 0° | 0mm | 0mm | 0mm | 0° |
| Surgical | 31.A3 | 0° | 0° | 0mm | 0mm | 0mm | 0° |
| Surgical | 32.A1 | 0° | 0° | 0mm | 0mm | 0mm | 0° |
| Surgical | 32.A2 | 0° | 0° | 0mm | 0mm | 0mm | 0° |
| Surgical | 32.A2 | 10° varus | 0° | 0mm | 2mm | 0mm | 0° |
| Surgical | 32.B1 | 0° | 0° | 2mm | 2mm | 0mm | 0° |
| Surgical | 32.B1 | 0° | 0° | 0mm | 0mm | 0mm | 0° |
| Surgical | 32.B1 | 0° | 0° | 0mm | 2mm | 0mm | 0° |
| Surgical | 33.A1 | 0° | 5° antecurvatum | 0mm | 0mm | 0mm | 0° |
| Surgical | 33.A2 | 0° | 0° | 0mm | 0mm | 0mm | 0° |
| Surgical | 33.A2 | 0° | 0° | 2mm | 0mm | 0mm | 0° |
| Surgical | 33.A2 | 0° | 0° | 0mm | 0mm | 0mm | 0° |
| Surgical | 33.A3 | 0° | 5° Recurvatum | 2mm | 2mm | 0mm | 0° |
| Surgical | 33.A3 | 0° | 0° | 0mm | 0mm | 0mm | 0° |
| Surgical | 41.B1 | 0° | 0° | 0mm | 0mm | 0mm | 0° |
| Surgical | 41.B1 | 5° valgus | 0° | 0mm | 0mm | 0mm | 0° |
| Surgical | 41.B1 | 0° | 0° | 0mm | 0mm | 0mm | 0° |
| Surgical | 41.C1 | 0° | 0° | 2mm | 0mm | 0mm | 0° |
| Surgical | 42.A1 | 0° | 0° | 0mm | 2mm | 0mm | 0° |
| Surgical | 42.A2 | 0° | 5° antecurvatum | 0mm | 0mm | 0mm | 0° |
| Surgical | 42.A2 | 0° | 0° | 0mm | 2mm | 0mm | 0° |
| Surgical | 43.B2 | 10° valgus | 0° | 0mm | 0mm | 0mm | 0° |
| Conservative | 32.A1 | 10° valgus | 10° Recurvatum | 0mm | 2mm | 4mm | 0° |
| Conservative | 32.A1 | 15° Valgus | 5° Recurvatum | 0mm | 2mm | 2mm | 0° |
| Conservative | 32.A2 | 0° | 5° antecurvatum | 2mm | 2mm | 3mm | 0° |
| Conservative | 32.A2 | 5° valgus | 5° recurvatum | 2mm | 2mm | 2mm | 0° |
| Conservative | 33.A1 | 0° | 5° recurvatum | 0mm | 0mm | 0mm | 0° |
| Conservative | 41.B1 | 10° valgus | 5° antecurvatum | 2mm | 4mm | 4mm | 0° |
| Conservative | 41.C1 | 5° valgus | 0° | 0mm | 0mm | 0mm | 0° |
| Conservative | 42.A1 | 10° varus | 5° recurvatum | 2mm | 2mm | 2mm | 0° |
| Conservative | 42.A2 | 15° valgus | 10° recurvatum | 2mm | 2mm | 2mm | 0° |
| Conservative | 43.B2 | 0° | 0° | 2mm | 0mm | 0mm | 0° |
| Conservative | 43.B2 | 5° valgus | 0° | 0mm | 2mm | 0mm | 0° |
| Conservative | 43.B2 | 10° varus | 10° antecurvatum | 4mm | 2mm | 4mm | 0° |
Comparison of the radiological results between the surgical group (Q) and the conservative group (C). In (A), comparison table classifying the radiological results into four grades: very good, good, satisfactory and poor. In (B), 2×2 table, grouping into two categories according to good or poor outcome.
AD: preoperatively, both groups had similar pain and AD. In group Q, 19 of the 25 patients (76%) presented postoperative symptoms of AD. Forty-eight percent of them already had symptoms preoperatively. In all cases, the symptoms disappeared within 17 days following the injury. In group C, 5 of the 12 patients (42%) had post fracture symptoms. And 50% had symptoms prior to the fracture. Subsequently, 4 patients of group C (33%) still had symptoms at 6 months and 3 of them presented non union demonstrated radiologically.
Pain: the average result at 3 months was: group Q VAS 2 (range 0–5) and group C VAS 4 (range 0–8). At 6 months: group Q VAS 1 (range 0–2) and group C VAS 3 (range 0–5). The statistical analysis found no significant differences between the groups (p>0.05).
Satisfaction with the treatment: in group Q, 92% of the patients said that they would undergo the operation again if they sustained a further fracture. In addition, all the patients that had been treated conservatively in the past for other fractures (6 out of 25) claimed they would prefer surgery.
Complications: prior to treatment, 4 patients of group Q were diagnosed with a urinary tract infection (UTI) (16%), a comparable proportion to group C (2 patients out of 12; 17%). None of the patients sustained a chest infection. All the infections were treated satisfactorily with no added morbidity. After treatment and during the hospital stay, seven UTIs were diagnosed in group C (28%) and two pneumonias (8%). In group Q, four UTIs (33%) and two pneumonias (17%). All the infections were treated satisfactorily with no added complications.
No case of thrombosis was detected in the patients of group Q. In group C, one patient with a tibial plateau fracture and contralateral tibial diaphysis fracture suffered an acute pulmonary thromboemolism, requiring admission to the intensive care unit for 12 days with satisfactory postoperative outcome.
The patients in group Q presented 4 pressure ulcers (16%), predominantly on the heel, type I (50%) and II (50%). These resolved in 18 days (range 14–29), without requiring surgery. In group C, despite the prophylactic measures, 10 patients (83%) developed a PU, type II (70%), III (20%) and IV (10%). The areas affected were: ankle (60%), ischium (30%) and knee (10%). These resolved in 29 days (range 14–75). Two (ankle type III and ischium type IV) required surgical treatment with pedicle flap. Statistical analysis found significant differences in favour of group Q (p<0.05) with regard to the number of PU.
DiscussionThere is currently no consensus with regard to the management of LLF in patients with cSCI. Traditionally, surgical treatment is avoided due to the high rate of surgical complications, lack of union, osteoporosis and lack of active mobility in these patients.28 Some studies propose conservative treatment, such as splints and well-padded casts,6,10–13 despite the risk of UP and thromboembolic events.27 Recently, in specific situations, surgical treatment has been recommended. Nottage10 recommends open reduction and internal fixation of hip fractures to improve sitting capacity. Baird et al.12 used external fixation to treat diaphyseal femur fractures, believing it to provide the patient greater autonomy and enable them to use a wheelchair sooner than when using splints. Frotzler et al.29 have also recently published good outcomes with external fixation for tibia and fibula, finding no differences compared to internal fixation. Levine et al.14 suggest that external fixators interfere with the position of the patient, and by contrast, internal fixation might simplify this problem. In any case, we believe that it might be a technique to be taken into consideration. McMaster and Stauffer17 consider that open reduction and internal fixation should be used whenever there are difficulties with circular casts and traction methods for controlling the fracture.
Hospital stay: in our series, we found no significant differences between the groups. The mean duration of treatment was 18 days, less than that described in previous studies.6,10–14,17,27,28
Range of motion: only Cochran et al.23 refer in detail to the range of movement of patients treated conservatively.23 In their study, 87% of the patients developed restricted knee flexion less than 90°. In our group Q, by contrast, we achieved a loss in range of motion to less than 10° compared to the contralateral limb. The range of motion was better in the surgical group than in the conservative group.
Radiological results: according to Schmeiser et al. there is little mention of radiological results in the literature and generally only shortening and poor alignment are considered.6,8,11 In our series, we had 13 cases (35%) of poor alignment. The radiological results in terms of alignment and union were better in the surgical group. Our results are comparable with the most recent published series.19,22,24
Pain and AD: in group Q, the pain or AD disappeared after 17 days on average in all patients and did not affect their level of autonomy. Thirty-three percent of the patients in group C still presented pain and AD 6 months after the fracture, of whom 75% presented radiological non-union of their fracture. These patients reported a significant reduction in their autonomy and required assistance in many of their daily activities, principally to do with hygiene. Therefore we can confirm that the radiological results, especially in terms of fracture union, correlate with the clinical results, and specifically with the patient's pain and independence.
Level of satisfaction: there are no studies that assess patient satisfaction with the outcomes achieved. In our series, it appears high in group Q since 92% of patients would choose the same form of treatment again.
Complications: we observed no significant differences in the rate of complications, before and after treatment in our two groups. Some authors had previously described skin complications, such as PU due to casts and splints.6,16,18,23 In our study, we observed a lower incidence of PU in group Q (16%) than group C (83%).
ConclusionsAlthough not free from complications, our outcomes demonstrate that surgical stabilising is a valid strategy in patients with cSCI presenting a lower limb fracture. In fact, as we describe, the patients in group Q had better union and alignment, practically free range of motion and a low rate of complications.
We believe that the most important factor in choosing treatment should be that it provides the patient with a better degree of Independence. Splints and casts make managing a wheelchair more laborious and delay patient recovery. By contrast, surgical treatment offers a rapid return to functionality. Despite our scant experience with external fixators, we prefer internal fixation for this population, because it facilitates management and care in hospital and at home.13,22,29,30
The study has limitations because it is retrospective with a limited number of patients, with a heterogeneous group in terms of fracture type and site and with different surgical options offered. Therefore, we believe that more studies are required to confirm, with methodological certainty, the advantages of surgical treatment, and the differences between the types of osteosynthesis.22 At any rate, given the current lack of scientific evidence, we believe that our outcomes are sufficiently important and suggest that surgical fixation should be considered as a valid option for the treatment of LLF in the context of cSCI.
Level of evidenceLevel of evidence III.
Ethical responsibilitiesProtection of people and animalsThe authors declare that the procedures followed conform to the ethical standards of the committee for responsible human experimentation and in accordance with the World Medical Association and the Helsinki Declaration.
Data confidentialityThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThe authors have received no funding of any type to undertake this study.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Barrera-Ochoa S, Haddad S, Rodríguez-Alabau S, Teixidor J, Tomás J, Molero V. ¿Se deben tratar quirúrgicamente las fracturas de extremidad inferior en pacientes con lesiones medulares crónicas? Experiencia en un centro de referencia. Rev Esp Cir Ortop Traumatol. 2017;61:19–27.