There is currently great controversy about the ideal treatment of intraarticular calcaneal fractures. The objective of this study is to determine the usefulness of postoperative computed tomography (CT).
Material and MethodsWe conducted a retrospective descriptive study of patients operated on in the period 2007–2015 in our center. Epidemiological variables, specific fracture data, surgical intervention as well as results and complications were collected. The radiological evaluation was performed using simple radiology (Böhler angle) and coronal CT (congruence of posterior subtalar joint). For the functional results we use the AOFAS hindfoot scale and the EVA scale for the level of pain.
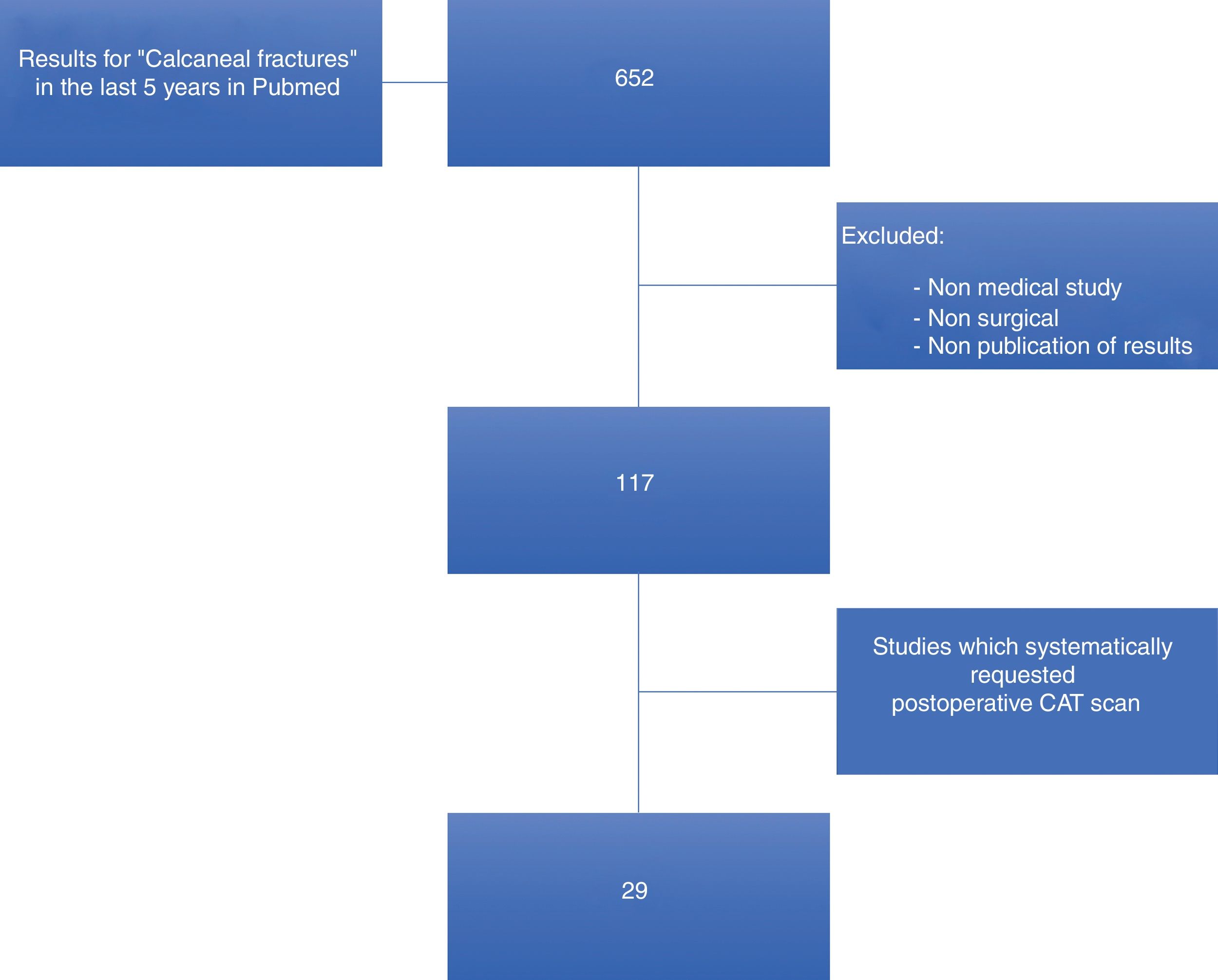
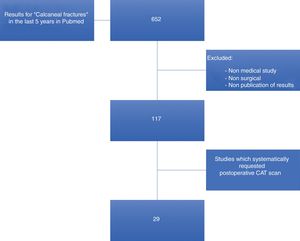
ResultsWe included 46 fractures in 43 patients (3 bilateral). 35 were male and 8 female, with an average age of 42 years (18−79) and an average follow-up of 57.39 months (33–129). Preoperative CT was performed in all cases, of which 11 were Sanders II, 23 type III and 12 type IV. Postoperative CT was only performed in 17 cases. The subsequent subtalar reduction measured by CT was satisfactory (articular step <2 mm) in 12 cases. The average presurgical Böhler angle was 6.45 ± 10.21 (-22−25) and the post-surgical angle of 20.46 ± 7.09 (4−38). Subtalar osteoarthritis developed in 19 cases (symptomatic in 12) and calcaneo-cuboid osteoarthritis in 6 cases (only 1 symptomatic). The AOFAS was 74.28 ± 18.98 (27−100) and the EVA was 4.14 ± 2.98 (2–9). A CT scan with a step of less than 2 mm was statistically significant, with a higher result on the AOFAS scale (77.17 average points) as well as lower EVA on average (2.83) (p = 0.002). Regarding the Böhler, it was statistically significant the relationship of an angle> 20° post-surgical with higher AOFAS (80.82) and lower VAS (3.18) (p = 0.001). The literature search obtained a total of 117 articles that met the search criteria, of which only 29 requested postoperative CT.
ConclusionsThe indication of postoperative CT in patients operated by intraarticular calcaneal fracture is the best technique to corroborate the correct reduction of the subtalar joint surface, although it is not universally accepted, according to the literature.
Actualmente existe gran controversia sobre el tratamiento ideal de las fracturas articulares de calcáneo. El objetivo de este estudio es determinar la utilidad de la tomografía computarizada (TC) postoperatoria.
Material y MétodosEstudio retrospectivo descriptivo de pacientes intervenidos en el período 2007 a 2015 en nuestro centro. Se recogieron variables epidemiológicas, datos específicos de la fractura, intervención quirúrgica así como resultados y complicaciones. La evaluación radiológica se realizó mediante radiología simple (ángulo de Böhler) y TC coronal (congruencia de subastragalina posterior). Para los resultados funcionales utilizamos la Escala AOFAS de retro pie y la escala EVA para el nivel de dolor.
ResultadosIncluimos 46 fracturas en 43 pacientes (3 bilaterales). 35 eran varones y 8 mujeres, con una edad promedio de 42 años (18-79) y un seguimiento medio de 57,39 meses (33-129). LA TC preoperatoria se realizó en todos los casos, de los que 11 fueron Sanders II, 23 tipo III y 12 tipo IV. El TAC postoperatorio solo se realizó en 17 casos. La reducción de la subastragalina posterior medida por TAC fue satisfactoria (escalón articular < a 2 mm) en 12 casos. El ángulo de Böhler prequirúrgico promedio fue de 6,45 ± 10,21 (-22 – 25) y el postquirúrgico de 20,46 ± 7,09 (4 – 38). La artrosis subastragalina se desarrolló en 19 casos (sintomática en 12) y la artrosis calcaneo-cuboidea en 6 casos (sólo 1 sintomático). El AOFAS fue de 74,28 ± 18,98 (27 – 100) y el EVA de 4,14 ± 2,98 (2-9). Resultó estadísticamente significativo un TAC con escalón inferior a 2 mm con mayor resultado en la escala AOFAS (77,17 puntos de promedio) así como menor EVA de promedio (2,83) (p = 0,002). Respecto al Böhler, resultó significativa la relación de un ángulo >20º postquirúrgico con mayor AOFAS (80,82) y menor EVA (3,18) (p = 0,001). La búsqueda bibliográfica obtuvo un total de 117 artículos que cumplieran los criterios de búsqueda, de los cuales sólo 29 solicitaron TC postoperatorio.
ConclusionesLa TC postoperatoria es la mejor técnica para corroborar la correcta reducción de la superficie articular subastragalina, sin embargo, su indicación no está universalmente aceptada.
Calcaneal fractures are the most common fractures of the tarsus and up to 75% have joint extension. The great majority occur in young males in the workplace environment, with subsequent socio-economic impact. Regardless of the method of treatment used, intraarticular calcaneal fractures are highly incapacitating injuries.1,2
Few subjects in orthopaedic surgery have raised as much controversy as the ideal treatment for displaced intraarticular calcaneal fractures. Historically treated conservatively, over the last few years advances gained in preoperative assessment, imaging methods and surgical techniques have changed the paradigm, with most authors advocating surgical treatment. Evidence supporting conservative treatment of these fractures is scarce and the level of recommendation is poor.3–6 The literature shows that the poorest outcomes are to be found in displaced and comminuted fractures, imprecise surgical reductions of the subtalar joint, males over 50 years of age and patients who do heavy manual labour or patients involved in employment litigation.4 Hence the most favourable outcomes are obtained in young, female patients who do not perform heavy manual labour and with simple fracture lines.7 Even so, evidence supporting surgical treatment remains moderate (level of recommendation B according to evidence-based medicine).
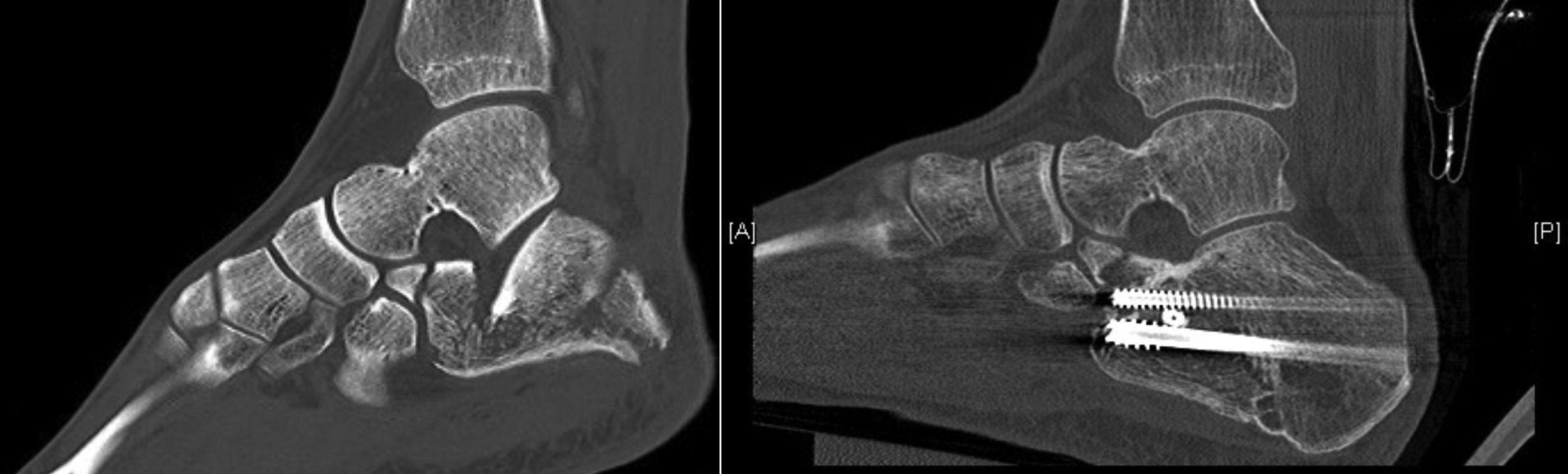
Subtalar osteoarthritis secondary to calcaneal fracture probably has many origins, with major importance being attached to cartilaginous damage produced at the time of impact, and the incongruence or the presence of articular displacement. The 2 mm limit of articular displacements is classically used to indicate surgical treatment of a joint fracture, but in fractures with minimum displacement in which no computerized tomography (CT) has been performed, this limit of 2 mm is impossible to determine by plain x-ray and could explain how, in fractures secondary to apparent low energy injury mechanisms, we observe degenerative radiological changes during the first 2–3 years although not always with medical repercussions. In short, plain x-rays do not detect minimum joint incongruencies. However, although consensus in the literature does exist on the indication for computerized tomography (CT) prior to surgery for precise surgical planning, postoperative CR to verify the absence of articular displacements is not universally accepted.
The aim of our study was to assess the usefulness of postoperative CT in surgically treated calcaneal intraarticular fractures. The working hypothesis is that postoperative CT may not be vital but it is highly useful for assessing the quality of subtalar joint reduction (which is difficult to demonstrate with conventional radiology).
Patients and methodWe conducted a retrospective descriptive study of patients operated on in a tertiary level university hospital in the period from 2007–2015. The study was approved by the hospital ethics committee. The inclusion criteria were as follows:
- •
Surgically treated calcaneal joint fracture.
- •
Absence of previous foot and/or ankle injury which altered functional outcomes.
- •
Informed consent given.
Exclusion criteria were as follows:
- •
Loss of follow-up
- •
Refusal to participate in this study.
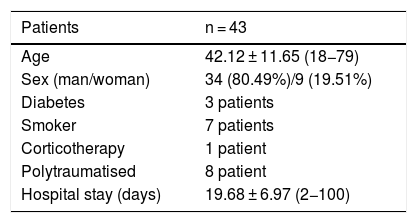
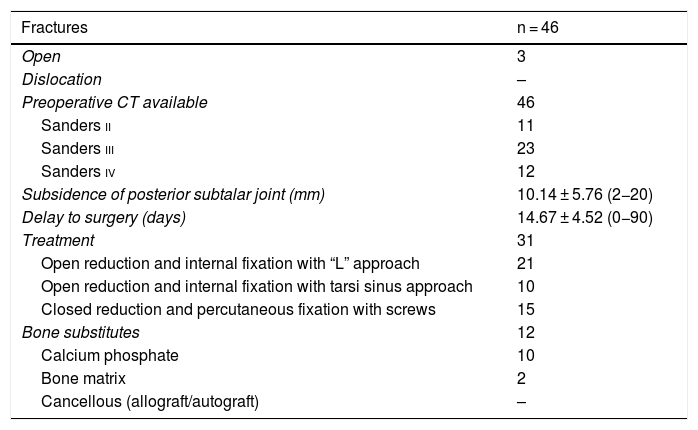
Epidemiological variables, specific fracture data and surgical intervention data were collected (Tables 1 and 2). For fracture classification we used Sanders classification, based on assessment through coronal CT of the posterior subtalar facet, depending on the number of fragments displaced over 2 mm of this facet. This classification has been widely studied and although its high intra and interobserver variability has been criticised, it remains the benchmark classification.8–12 Furthermore, its prognostic value has been demonstrated for predicting subtalar arthrodesis (5.5 times greater probability of determining sanders type IV than Sanders type II in subtalar arthrodesis).12
Fracture data.
| Fractures | n = 46 |
|---|---|
| Open | 3 |
| Dislocation | – |
| Preoperative CT available | 46 |
| Sanders ii | 11 |
| Sanders iii | 23 |
| Sanders iv | 12 |
| Subsidence of posterior subtalar joint (mm) | 10.14 ± 5.76 (2−20) |
| Delay to surgery (days) | 14.67 ± 4.52 (0−90) |
| Treatment | 31 |
| Open reduction and internal fixation with “L” approach | 21 |
| Open reduction and internal fixation with tarsi sinus approach | 10 |
| Closed reduction and percutaneous fixation with screws | 15 |
| Bone substitutes | 12 |
| Calcium phosphate | 10 |
| Bone matrix | 2 |
| Cancellous (allograft/autograft) | – |
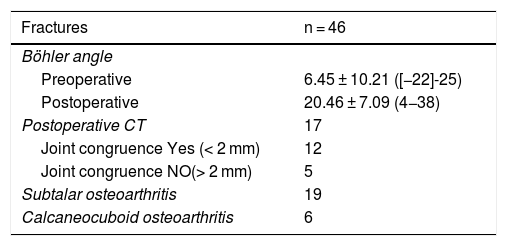
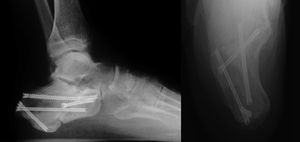
When assessing the radiological outcome of our surgical intervention we calculated Böhler angle in plain radiology in all cases and subsidence or presence of articular displacement higher than 2 mm (incongruence) in the posterior subtalar joint using CT in the patients for whom plain radiology revealed doubts regarding anatomical reduction. We also recorded the presence of subtalar and/or calcaneo-cuboid osteoarthritis in follow-up with plain radiology and confirmed this with CT. Regarding functional outcome, we used the hindfoot and ankle AOFAS scale (functional scale of the American Association of Foot and Ankle Surgery, which ranges from 0 to 100 points) and the VAS scale (visual analogue scale) for the recording of pain.
Statistical analysisCollected data were processed on a database and analysed with the SPSS® programme (Statistical Package for the Social Sciences de IBM; Chicago, Illinois, U.S.A.). Statistical associations were determined using the Fisher exact tests and/or χ2 (qualitative variables) and the Student’s t-test (quantitative variables) depending on the case; p < .05 values were considered to be statistically significant. The strength of epidemiological associations was considered significant by estimating the relative effectiveness of the 95% confidence interval, which was then adjusted by covariables. We analysed the relationship between AOFAS and VAS with the recovery of the Böhler angle and joint congruence.
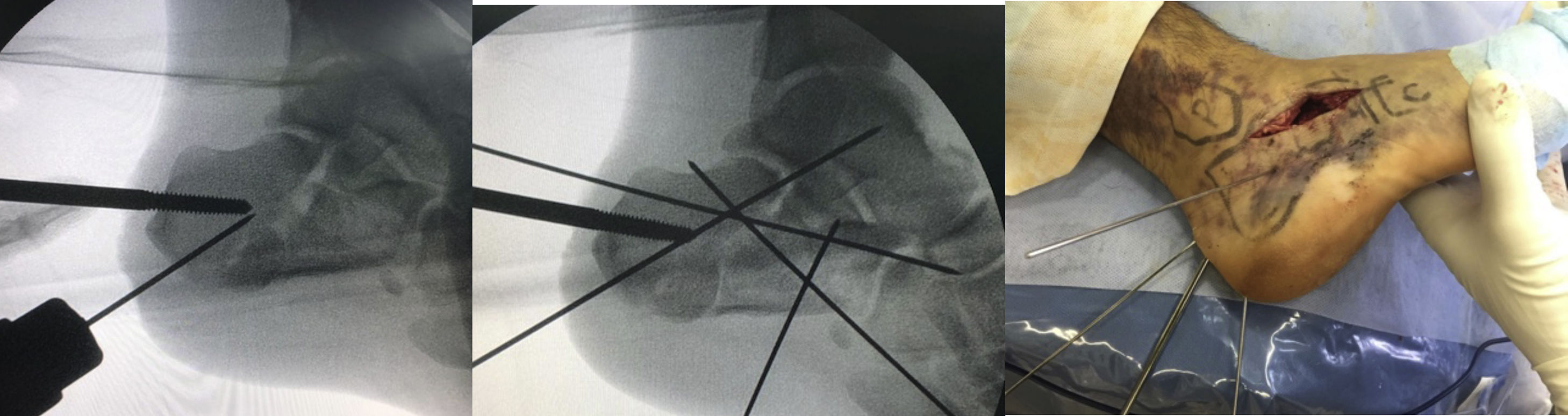
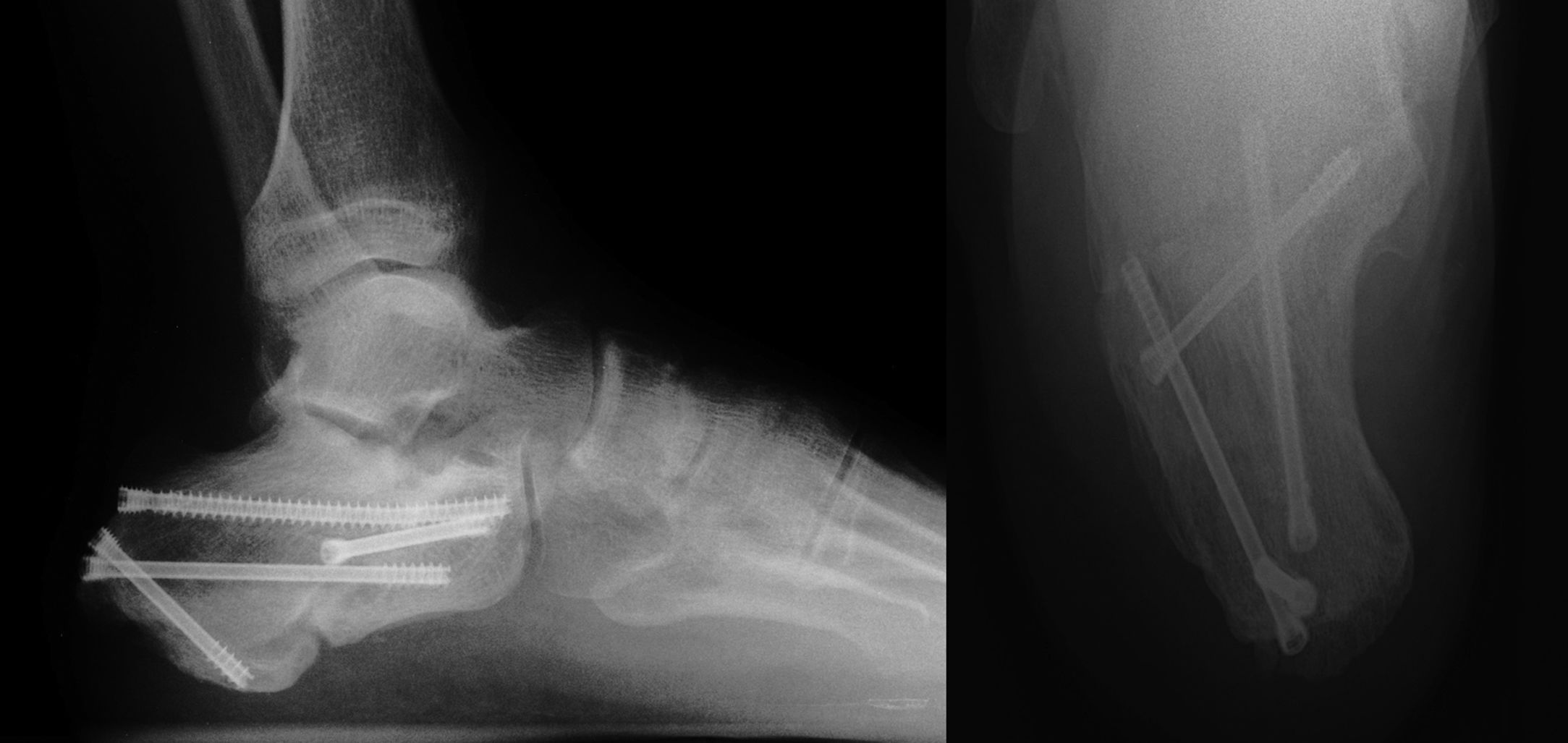
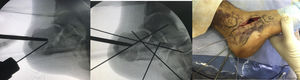
ResultsWe recorded 46 intraarticular fractures in 43 patients (three bilateral). Thirty five were male and eight were female, with a mean age of 42 years (18−79) and a mean follow-up of 57.39 months (33–129). In all cases preoperative CT was performed resulting in: 11 Sanders type II, 23 type III and 12 type IV cases (Table 2). With regard to surgical technique, a standard “L” shaped approach and osteosynthesis with low-profile blocking plates was used in 21 patients (12 Sanders type IV patients and 9 Sanders type III patients), in 10 cases a minimally invasive approach was used of the sinus tarsi (10 Sanders type III cases: four cases synthesized with cannulated screws and six cases with ad hoc anatomical plates with/without cannulated screws (Figs. 1 and 2) and in 15 cases we decided to use an indirect reduction and percutaneous fixation with cannulated screws (11 Sanders type II and four Sanders type III cases) (Fig. 3 ) (Table 2).
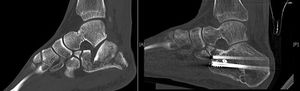
Postoperative CT (defined as that performed prior to hospital discharge of the patient or in the first month of follow-up) was performed only in those cases in which the surgeon considered that pain radiology would not clarify the quality of the joint reduction, resulting in a total of 17 cases (37% of the series, six Sanders type IV patients treated with the “L” approach, nine Sanders type III patients treated by sinus tarsi and two Sanders type II patients treated with closed reduction and fixation with screws). The reduction of the posterior subtalar joint measured by CT was satisfactory in 12 cases (defined as an articular displacement < 2 mm). In the other five cases the displacement was above 2 mm (one Sanders type iv case, one Sanders type iii case of tarsi sinus, one Sanders type iii case with indirect reduction and cannulated screws and two Sanders type ii cases also with indirect reduction). Reintervention was decided in only one case (patient with Sanders type II fracture) with an “L” approach and low-profile plate, with good radiological and functional outcome. Of the remaining four cases the risk/benefit balance of further surgery called for conservative treatment, particularly due to the further aggression to soft tissues. The average preoperative Böhler angle was 6.45 ± 10.21 ([-22]-25) and postoperative angle was 20.46 ± 7.09 (4−38). CT in follow-up (defined as over one year after surgery) was performed in 31 cases, only in those where three was suspicion of a post-traumatic degenerative pathology following analysis of plain radiology: subtalar osteoarthritis was diagnosed in 19 cases (symptomatic in 12, seven of them treated with subtalar arthrodesis) and calcaneo-cuboid osteoarthritis in six cases (only one symptomatic and treated conservatively) (Table 3). The AOFAS was 74.28 ± 18.98 (27−100) and the VAS 4.14 ± 2.98 (2–9).
The most common complication was intolerance of osteosynthesis material, in eight cases: five cases with low-profile osteosynthesis plates due to irritation of the peroneal tendons and three cases treated with cannulated screws, due to discomfort in the area of the heel. We recorded three cases of intraarticular penetration of screws in the posterior subtalar joint, detected by CT in the follow-up of over one year. No re-interventions were performed in any cases due to the absence of medical repercussions. We recorded two infections: one superficial which responded to antibiotic treatment and one deep infection which required debridement, excision of material one year following surgery and subtalar arthrodesis.
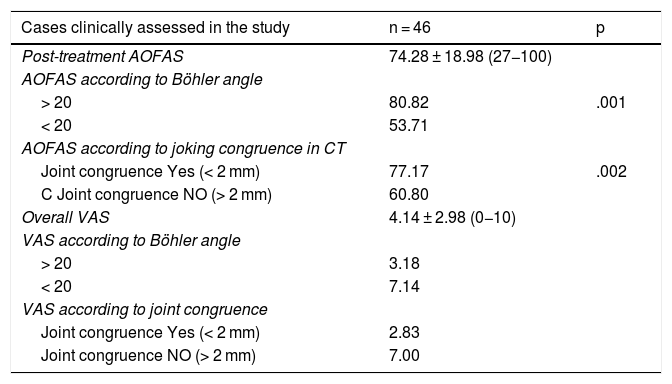
A CT revealing an articular displacement under 2 mm was statistically significant in 12 patients of our series with better outcome in the AOFAS scale (77.17 points on average) and lower than average VAS (2.83), p = .002. Regarding the Böhler angle, the relationship of an angle > 20° with higher AOFAS (80.82) and lower VAS (3.18), p = .001 was significant (Table 4).
Functional results and statistical analysis.
| Cases clinically assessed in the study | n = 46 | p |
|---|---|---|
| Post-treatment AOFAS | 74.28 ± 18.98 (27−100) | |
| AOFAS according to Böhler angle | ||
| > 20 | 80.82 | .001 |
| < 20 | 53.71 | |
| AOFAS according to joking congruence in CT | ||
| Joint congruence Yes (< 2 mm) | 77.17 | .002 |
| C Joint congruence NO (> 2 mm) | 60.80 | |
| Overall VAS | 4.14 ± 2.98 (0−10) | |
| VAS according to Böhler angle | ||
| > 20 | 3.18 | |
| < 20 | 7.14 | |
| VAS according to joint congruence | ||
| Joint congruence Yes (< 2 mm) | 2.83 | |
| Joint congruence NO (> 2 mm) | 7.00 |
The results of this study indicate that postoperative CT is the most reliable imaging technique for verifying accurate anatomical reduction in surgically treated calcaneal joint fractures. We carried out a literature search on the indication of this test in treatment protocol and for this we used the PubMed search engine dated August 2019 with the following key words: calcaneal fractures and treatment, and CT scan, in the last five years. Our aim was to assess the published works on surgically treated calcaneal fractures for which postoperative CT was conducted (Fig. 4). A total of 652 results was obtained. After the elimination of non-related articles and articles published more than five years previously, a total of 117 articles met with our search criteria, of which only 29 requested postoperative CT (Fig. 4). Of these, only two reported on the indication of postoperative CT request,13,14 and in the remaining 27 the cause of the indication for this test was not specified and it was inferred that this simply formed part of their protocol, as occurs in other centres for the assessment of joint fractures before and after surgery. In 2017 De Muinck-Keizer et al.13 conducted a study for the assessment of joint reduction and the correct positioning of osteosynthesis material in calcaneal fractures, highlighting in their article the absence of postoperative protocols based on carrying out postoperative CT; the authors concluded, following the design of a specific point system, that the CT provided extremely valuable information on their two initial aims. Also in 2019, Beerekamp et al.14 carried out an interesting comparative study of different imaging techniques: intraoperative 2D and 3D fluoroscopy for assessment of joint reduction and the positioning of implants, concluding that although 3D intraoperative fluoroscopy is very useful, particularly in the assessment of the positioning of implants, CT remained the study of choice. To sum up, our review of the literature demonstrated that postoperative outcomes are not systematically analysed with postoperative CT or in patient follow-up and it its use is the only way to demonstrate anatomical reduction (displacement under 2 mm) and the correct positioning of implants.
The ideal treatment of displaced calcaneal intraarticular fractures continues to be a topic of intense debate in foot orthopaedics.7,15–20 Regardless of the treatment used, be it surgical or conservative, recovery of the subtalar joint anatomy is essential for obtaining a normal gait pattern,21 an earlier return to work and a reduced need for future arthrodesis.2 In our analysis we confirmed that the postoperative congruence under 2 mm measured by CT was related to the best functional result and this fact has a high prognostic value which patients should be aware of. In the absence of an intraoperative arthroscopy or a direct visualization of the subtalar joint (open techniques), it is enormously difficult, when guided by intraoperative radioscopy, to verify the congruence of the subtalar joint surface. Therefore, we believe that postoperative CT is highly useful for perfecting surgical technique. This factor is particularly salient in the methods of indirect reduction, which are currently so popular because they are less aggressive to the already fragile cover of soft tissues in this región.15–20 Indeed, four of the five patients with articular displacement > 2 mm in the CT were operated on using minimally invasive techniques (one tarsi sinus approach and three percutaneous techniques and osteosynthesis with screws). This fact was already described by DeWall et al. in 2010, who insisted don the need for prospective studies using postoperative CT to assess joint reduction in percutaneous techniques.22
It is a proven fact in the literature that plain radiology is unreliable for assessing the reduction of the subtalar and calcáneo-cuboid joint surface, and for which postoperative CT clearly has proven superiority.18–20 In the article of Labbe et al. almost 35% of fractures in which plain radiology was proven to have good congruence, this was finally proven not to be the case when postoperative CT was performed.23 In our series postoperative CT demonstrated an incongruence of 29.4% of cases which had been found satisfying during surgery, and this constitutes a major prognostic factor which we would communicate to our patients.
Regarding surgery, the lateral “L” approach which was used as the gold standard is not exempt from complications, particularly of soft tissue, with percentages reaching up to 35% in some authors.22 As a result, during the last 10 years indirect, percutaneous techniques or those with minimal incision have been developed, which seek to minimize aggression of soft tissues, respecting joints. These have obtained similar or even superior clinical outcomes to open techniques.24–26 In our series we recorded 25 cases treated with minimally invasive techniques, with an average AOFAS score of 78.45 points. Although this was only recorded in 10 cases, the tarsi sinus approach has in the last 5 years become our technique of choice in most cases. In 2017 a randomised prospective study was published, comparing open surgery using the “L” technique with minimally invasive techniques, showing better radiological results in the minimally invasive technique, but not in functional results. Osteosynthesis techniques using percutaneous screws obtained the poorest results,27 although this was not visible in our series.
However, and although it does not form part of the aim of this study, a confirmed fact was that the number of fractures operated on per surgeons impacts clinical outcomes, with the end of the learning curve being reached.20 Anther possible advantage of postoperative CT therefore would be helping this curve to progress by measuring the quality of our reduction, and particularly in minimally invasive techniques. In fact, in this series, the best functional results regarding anatomical reduction were obtained in the cases where surgery had taken placed during the last three years of the period.
Our study had limitations, in addition to those inherent in the methodology as a retrospective study. We would highlight as the most important drawback the low number of postoperative CT scans requested (17 out of 46 cases) which is the norm in the majority of studies but the conclusions drawn from the study of this series should be cautiously viewed. This situation was so because in the series studied no postoperative CT was protocolised. It only took place if the surgeon had doubts based on plain radiology analysis, even though currently indication has increased and particularly in cases with indirect reduction.
A critical commentary on our study was the consideration of the financial factors and the higher dose of radiation for our patients but it is of note that patients were informed at all times of this situation.
ConclusionsBased on our results, postoperative CT is the most reliable imaging technique for verifying accurate anatomical reduction and positioning of implants in surgically treated calcaneal joint fractures. As authors we consider that it is particularly indicated in the use of the indirect techniques of reduction and osteosynthesis, where it is more difficult to confirm correct intraoperative joint reduction and it may also serve to advance the learning curve with the said surgical techniques. Lastly, studies with a higher number of cases are needed to confirm the advantages of routine use of this additional imaging study.
Level of evidenceLevel of evidence IV (case series).
Ethical liabilitiesProtection of people and animalsThe authors declare that for this research no experiments were conducted on humans or animals.
Data confidentialityThe authors declare they have complied with the protocols of the place of work on the publication of patient data and that all patients included in the study received sufficient information and gave their informed consent in writing to participate in this study.
Right to privacy and informed consentThe authors obtained the informed consent of the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Ojeda-Jiménez J, Rendón-Díaz D, Martín-Vélez P, González-Martín D, Boluda-Mengod J, Méndez-Ojeda M, et al. Fracturas intraarticulares de calcanéo tratadas quirúrgicamente: ¿qué nos aporta la tomografía computarizada postoperatoria? Rev Esp Cir Ortop Traumatol. 2020;64:393–400.