Morquio syndrome is caused by an inherited autosomal recessive enzyme deficiency. It presents with numerous musculoskeletal anomalies, among which atlantoaxial instability is highlighted, due it being life-threatening. Occipital-cervical arthrodesis surgery (and decompression) is indicated in these cases.
ObjectiveThe cases of two patients with Morquio syndrome that required this type of surgery are presented, along with a review of the literature.
Patients and methodsTwo patients: one boy and one girl, with Morquio syndrome and high cervical instability, with neurological signs and symptoms, who were subjected to surgery using decompression and instrumented occipital-cervical arthrodesis and followed up for 6 months and 1 year, respectively.
ResultsThe neurological problems of both patients improved, and are currently having a normal life for their age.
ConclusionOccipital-cervical arthrodesis with decompression provides a safe biomechanical environment that prevents neurological involvement. It should be indicated before the appearance of symptoms or mechanical instability.
El síndrome de Morquio se produce por un déficit enzimático de herencia autosómica recesiva. Presenta numerosas manifestaciones musculoesqueléticas, entre las que destaca por su riesgo vital la inestabilidad atloaxoidea. En estos casos está indicada la cirugía de artrodesis (y descompresión) occipitocervical.
ObjetivoSe presentan 2 pacientes con síndrome de Morquio que precisaron de este tipo de cirugía, así como una revisión de la literatura.
Pacientes y métodosDos pacientes: un niño y una niña, con síndrome de Morquio e inestabilidad cervical alta, con signos y síntomas neurológicos, que fueron intervenidos quirúrgicamente mediante descompresión y artrodesiso occipitocervical instrumentada; con un seguimiento de 6 y un año respectivamente.
ResultadosAmbos pacientes mejoraron de sus problemas neurológicos, realizando en al actualidad una vida normal para su edad.
ConclusiónLa artrodesis occipitocervical con descompresión proporciona un entorno biomecánico seguro que previene de la afectación neurológica. Estaría indicada ante la aparición de sintomatología o de inestabilidad mecánica.
Mucopolysaccharidoses (MPS) are a family of hereditary diseases involving deposits of lysosomes resulting from an enzyme deficit in the metabolism of glycosaminoglycans (GAG). There are six forms of MPS, each presenting a different phenotypic grade.
Morquio disease (MPS IVA) is an autosomal recessive deficit in the activity of certain enzymes, N-acetylgalactosamine-6-sulfatase (MPS IVA) or β-galactosidase (MPS IVB), resulting in the accumulation of keratan sulfate and chondroitin-6-sulfate.1 Skeletal manifestations in spondyloepiphyseal dysplasia include a delay in growth, odontoid hypoplasia, thoracolumbar kyphosis, hip dysplasia, genu valgo, liver spots and joint laxity, with normal mental capacity. The estimated incidence oscillates between 1/76,000 (Northern Ireland) and 1/640,000 (Western Australia) live births.2 Life expectancy is variable, depending on the degree of severity of the disease, but many patients die in adult age, approximately in the third decade of life, due to cardiopulmonary diseases or sequelae from neurological deficits.
The natural progression of this disease can lead to quadriplegia and sudden death secondary to atlantoaxial instability and spinal compression. Children with MPS IVA suffer odontoid hypoplasia, joint laxity and extradural deposits of GAG anterior to the spine at the C1 level which can result in atlantoaxial subluxation, stenosis and cervical myelopathy. GAG deposits are not observed in radiographs, they can only be detected by magnetic resonance imaging (MRI) which means that occipitocervical stenosis could be more severe than suspected from radiographs.1,3,4 Compression caused by the deposits, added to instability, can result in progressive weakness with myelopathy, thus leading some authors to favor occipitocervical fixation once instability has been demonstrated.1,3–7
Physiopathology of atlantoaxial instability in Morquio syndromeThe joint located between the anterior arch of C1 and the odontoid enables 50% of cervical lateral rotation. The correct function of the transverse and alar ligaments maintains the integrity of the atlantoaxial joint, limiting posterior translation of the odontoid.
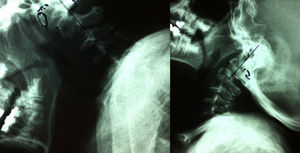
The distance between the anterior C1 arch and the odontoid apophysis (known as ADI), which is normally up to 2.5mm in adults and 5mm in children, is increased in flexion by subluxation of the segment, caused by a tendency toward local instability. This is just an indirect measurement of the space that is left for the spine, the truly important parameter, which is also measured between the posterior C1 arch and the odontoid apophysis (PADI) when there is difficulty to visualize the anterior atlantoaxial joint. In radiographs in flexion, when this displacement (dynamic concept) makes the ADI greater than the limits mentioned previously as normal, or when there is a variation greater than 2mm between the ADI in the lateral radiograph in flexion and in extension, we refer to atlantoaxial instability.2
Atlantoaxial instability is a common finding in MPS IVA and is thought to derive from odontoid hypoplasia, along with associated ligament laxity.8–10 Furthermore, instability in this entity can be multidirectional, both anteroposterior and mediolateral or craniocaudal, or even an association of all these components.
In flexion, the anterior C1 arch is displaced anteroinferiorly. Without competent ligaments which ensure that the odontoid follows the movement of C1, the posterior tilt of the odontoid (impingement) could cause compression of the cervical spine.
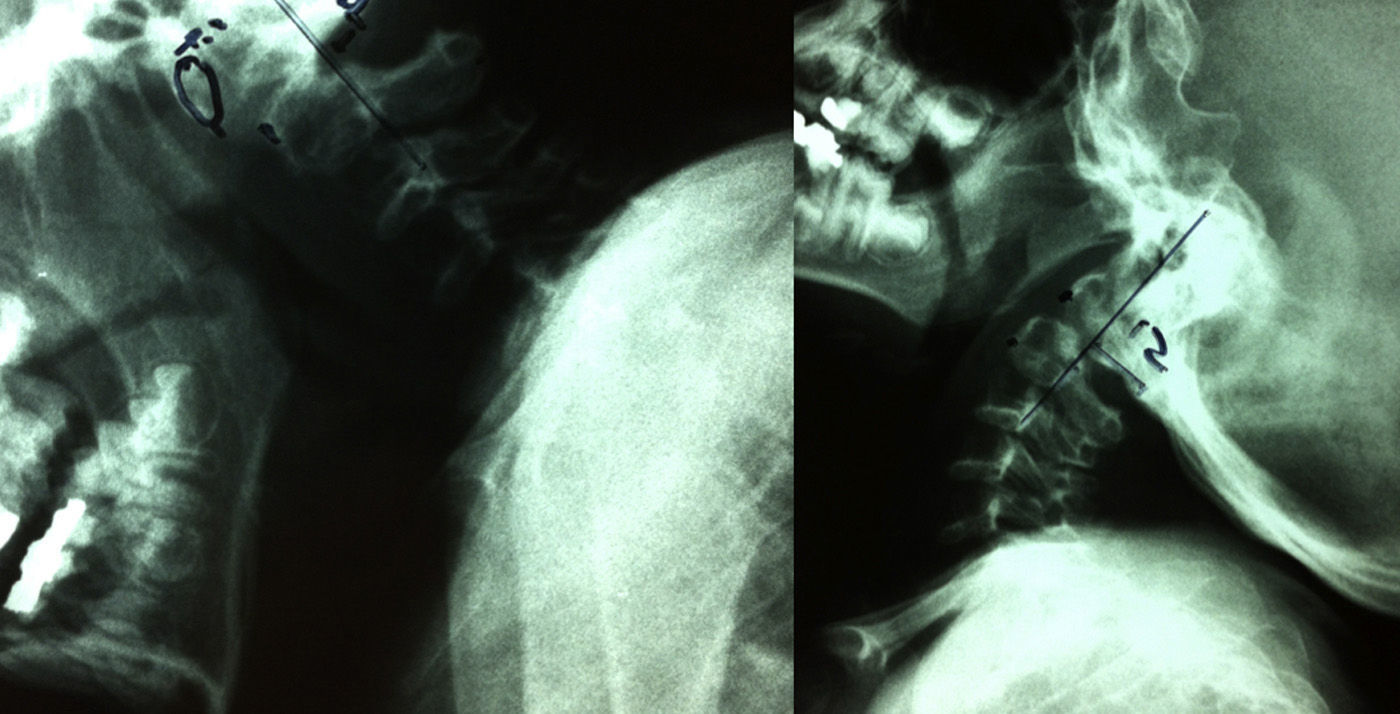
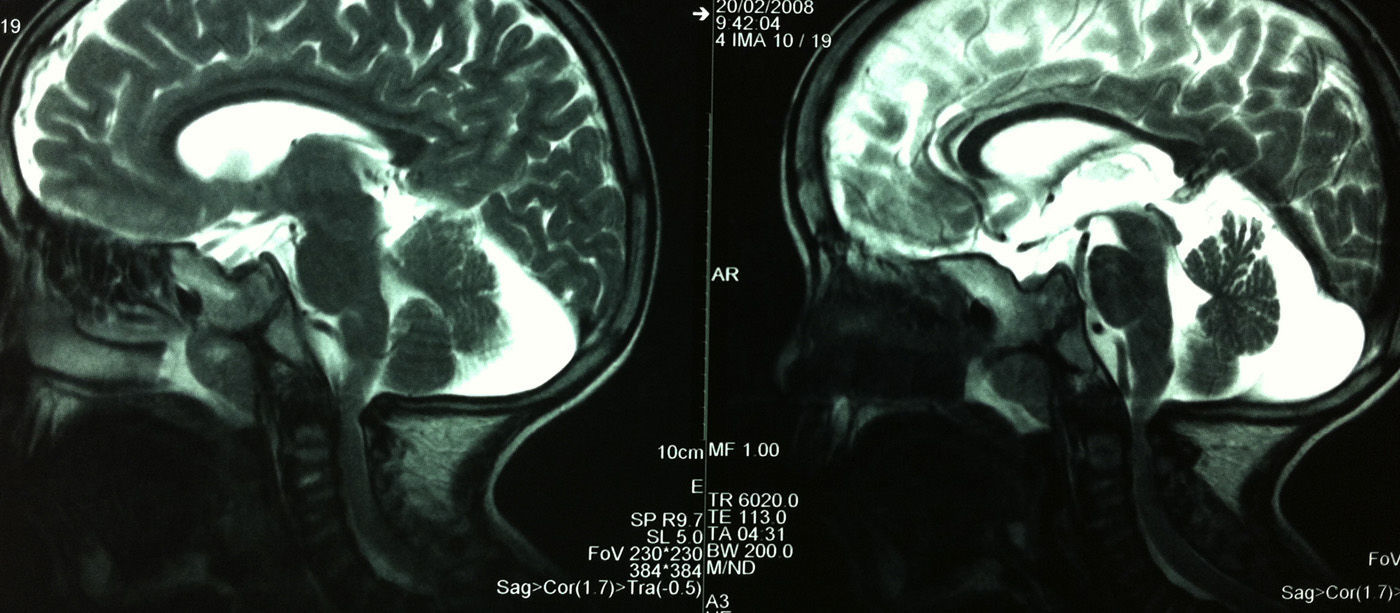
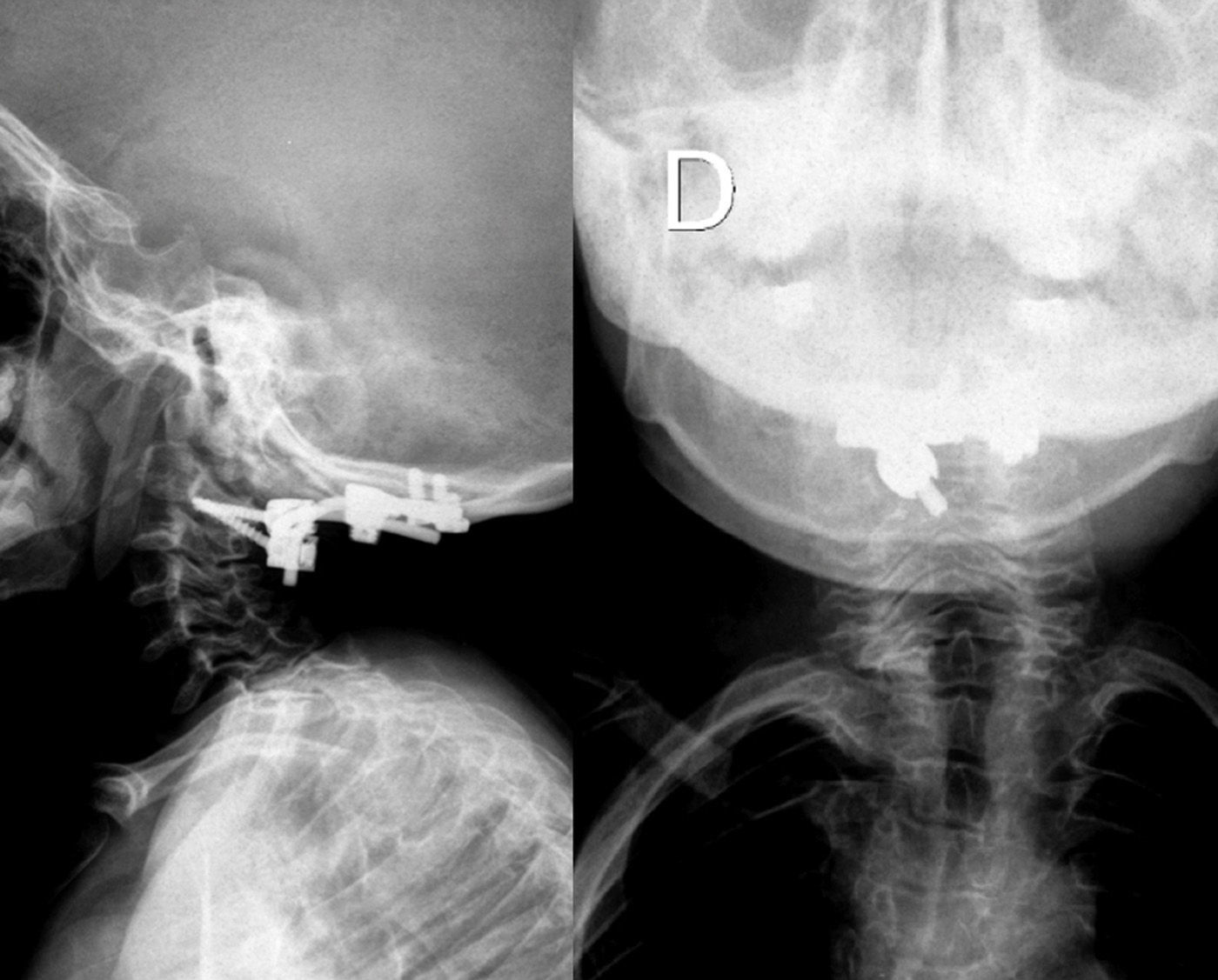
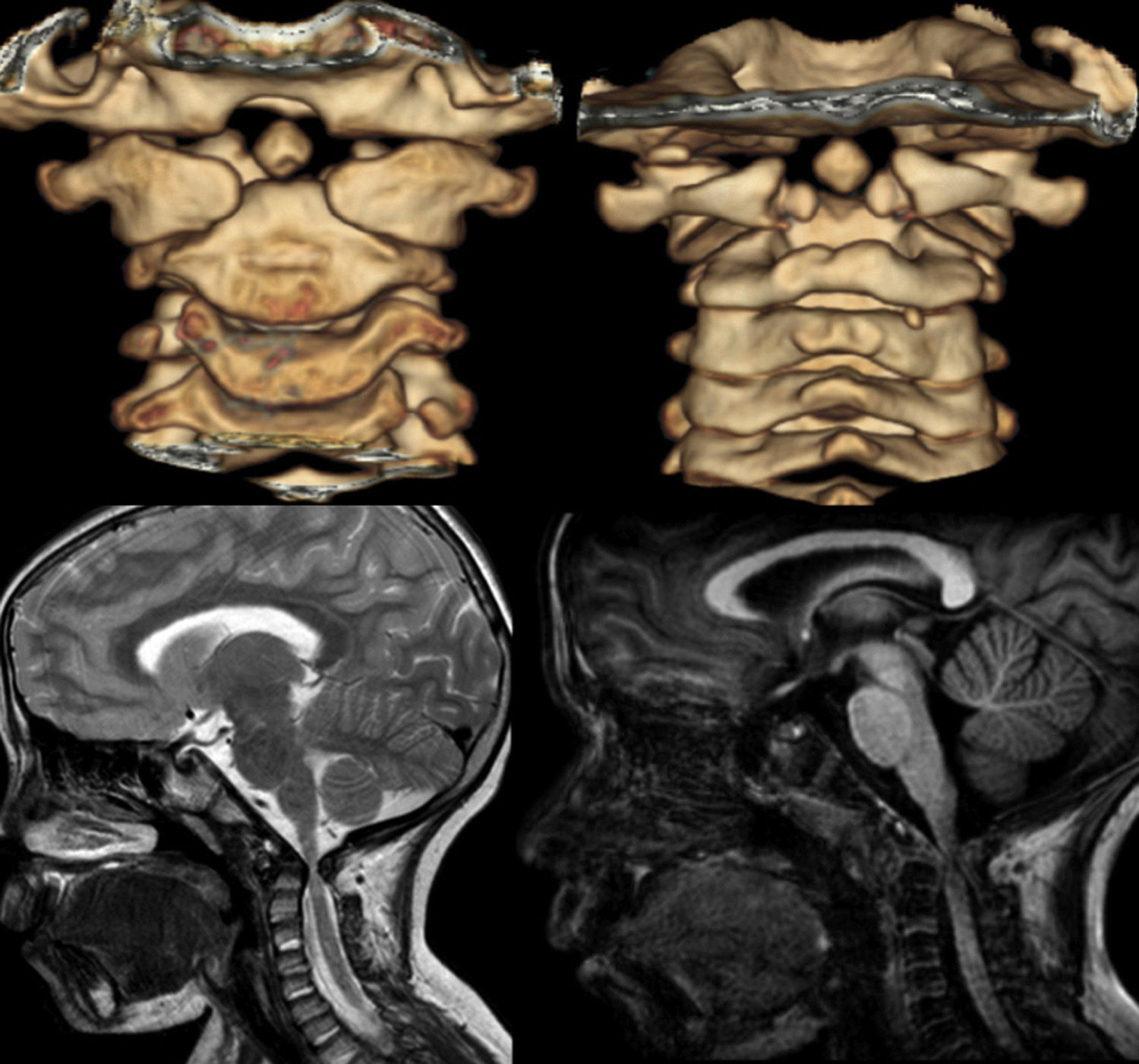
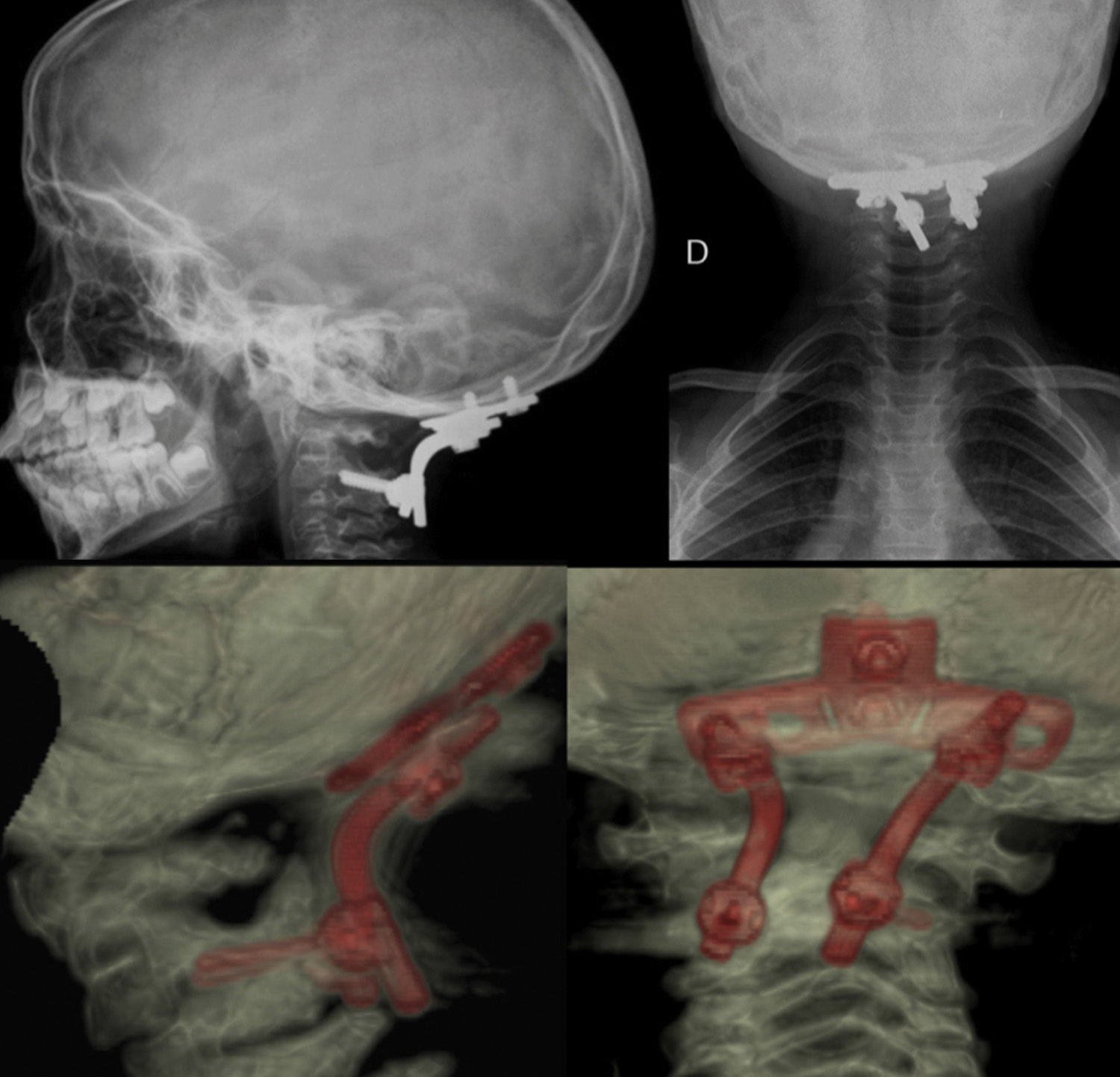
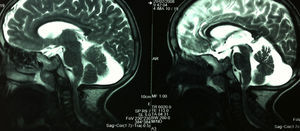
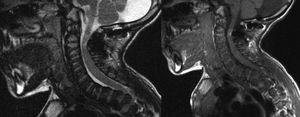
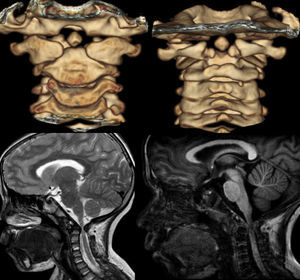
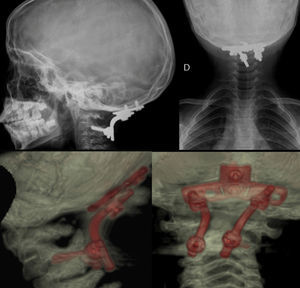
Materials and methodWe present two case reports treated at the hospital of the second author. The first patient was a 4-year-old boy who was referred from the Spine Unit for assessment of multiple epiphyseal dysplasia in a context of Morquio disease. The patient presented pectus carinatum, relative macrocephaly, severe bilateral genu valgo, scoliosis and thoracolumbar kyphosis. Following treatment for kyphoscoliosis with a plaster cast under general anesthesia and a TLSO-type brace, he began to present some signs of C1–C2 instability due to os odontoideum (Fig. 1). The radiographs showed occipitocervical instability and the MRI scan revealed spinal stenosis with a PADI of 5.5mm (Fig. 2). In light of these clinical characteristics, occipitocervical decompression-arthrodesis was indicated at the age of 8 years (Figs. 3 and 4). During the evolution, the patient was included in a study with enzyme replacement therapy.
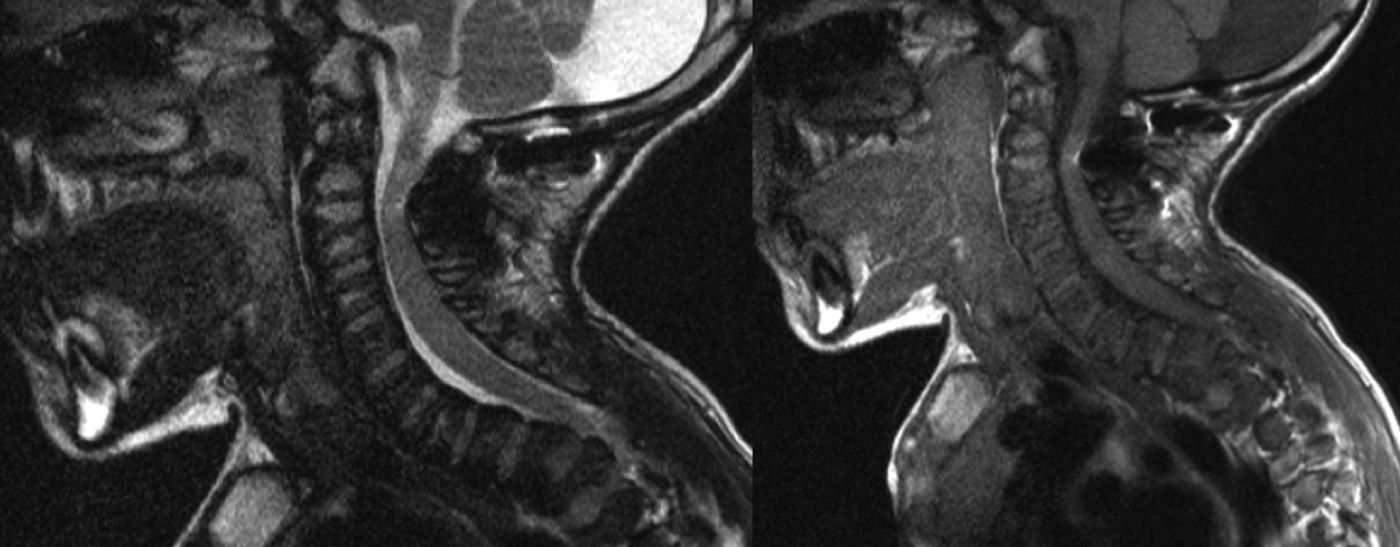
The second patient was an 8-year-old girl. On exploration, she pointed to numbness of hands and feet with frequent falls due to gait instability, with bilateral calf clonus of five to six shakes. Although the static radiograph was unremarkable, dynamic radiographs showed occipitocervical instability (Fig. 5). The study was completed by computed tomography (CT) and MRI (Fig. 6) scans, which confirmed stenosis at the level of the occipitocervical joint (PADI 5.7mm) and fusion anomalies in C1 and C2 which conditioned spinal compression, leading to a proposal of occipitocervical arthrodesis to C2 (Fig. 7).
The first case, with a follow-up period of 6 years, is currently asymptomatic, maintaining an adequate cervical coronal and sagittal axis, with no accompanying symptoms. Furthermore, the patient was also intervened for right genu valgo through hemiepiphysiodesis with an 8-shaped plate.
The postoperative period of the second case developed without incidents. Six months after the intervention, the symptoms improved, the patient fell less often and felt more agile, and numbness in hands and legs disappeared. After 1 year of follow-up, she is currently asymptomatic.
DiscussionMPS are a group of metabolic disorders, each of them characterized by a defect of a lysosomal enzyme. These disorders result in the accumulation of different types of GAG in cells, causing central nervous system, cardiovascular, pulmonary, ophthalmological, auditory and musculoskeletal disorders. Type IV MPS (Morquio syndrome) has predominantly orthopedic manifestations, involving severe problems of the vertebral spine.
Morquio syndrome was first described by Morquio11,12 and Brailsford13 in 1929. This rare, hereditary disorder, transmitted in an autosomal recessive pattern, is characterized by the reduction or absence of activity of N-acetylgalactosamine-6-sulfatase in Morquio type A,14 or β-galactosidase in Morquio type B.15 These enzyme deficiencies lead to a lack of degradation of keratan and chondroitin sulfate, which cause the clinical characteristics of skeletal dysplasia through intracellular accumulation.
In MPS IVA there is an interruption of normal development and maturation of cartilage and bone leading to multiple structural anomalies of the vertebral spine. Incomplete ossification of the odontoid causes local mechanical instability, very frequent in this syndrome. Other vertebral anomalies include platyspondylia, thoracolumbar kyphosis, specific shape of the vertebral bodies sharpened anteriorly in the sagittal plane, posterior vertebral scalloping and widened ribs.
The diagnosis is established by the physical and radiographic characteristics, deficiency in enzyme activity in fibroblast cultures, excessive accumulation of keratan sulfate in urine and confirmation through enzyme analysis.1,5 Prenatal diagnosis is also possible through electrophoresis of GAG in the amniotic fluid.16
Regarding more specific imaging tests, 3D-CT can provide reconstructed images of the superior cervical spine for preoperative planning. Furthermore, it can be an alternative to MRI, as it is faster to perform and is able to study instability with images in flexion and extension. It is important to bear the amount of radiation in mind (specific protocols for low doses of ionizing radiation). Regarding MRI, it is the ideal method to assess the degree of spinal compression, soft tissues, and it can also provide images of the instability in flexion-extension directly. Nevertheless, being a slower test compared to CT, it sometimes requires anesthesia in order to ensure that children remain still long enough to perform the test.
There is currently no data about the value of evoked potentials in the determination of spinal compression in the occipitocervical joint or in other locations in MPS IVA. Solanski et al. do not recommend testing potentials for the diagnosis or follow-up of progression of spinal compression in Morquio syndrome.2
MPS IVA requires a multidisciplinary approach to ensure a correct management of these patients. Close collaboration between the professionals treating these patients is essential to prevent neurological deterioration in those suffering MPS IVA.
Anesthetic management of patients with MPS IVA who are candidates for surgery is very complex. The accumulation of GAG at the level of the airway can cause difficulties for intubation and ventilation. Pulmonary function can be affected by obstruction of the upper airways, restrictive pulmonary disease secondary to scoliosis/thoracic kyphosis, pectus carinatum and respiratory muscle weakness secondary to myelopathy by chronic spinal compression. Since these complications increase the risk of perioperative morbidity and mortality, patients with MPS IVA should be treated by anesthetists with experience in these situations.
Cervical instability and the resulting stenosis are the most common causes of surgical interventions in the spine of patients with Morquio disease.1 The indications for surgery include neurological involvement on instability and spinal compression with changes in the MRI signal (myelomalacia), even without symptoms. Although prophylactic fusion has been recommended to prevent cervical myelopathy with better results in neurological recovery compared to performing fixation once the stenosis has become established,5 this must be assessed together with the family on a case by case basis, since it involves a considerable surgical procedure on a child with perioperative morbidity who, at the time of diagnosis, may be asymptomatic.
The main objectives of this surgery are to prevent the progression of spinal damage through decompression and to correct the instability and the deformity. In the thoracolumbar spine, where the stenosis is associated to kyphosis, decompression and correction of the sagittal and coronal planes are the main objectives.
When atlantoaxial subluxation advances to instability according to the previously mentioned concepts, the advice is to employ posterior cervical arthrodesis for stabilization, occasionally requiring the association of a decompression of the foramen magnum in order to guarantee spinal decompression.
Instrumentation of the superior cervical spine has evolved considerably in recent years. The previous techniques based on cerclage (Brooks, Gallie) have become obsolete through the development of adapted occipital plates, polyaxial screws and the possibility of placing them in a transarticular position, in the lateral masses, C2 pedicle, in the pars or in a transluminal position. Placement of screws through the lamina or pedicle has been proven safer in free hand fixation of the C2 vertebra.17
Occasionally, surgery with fixation to C2 is not possible in very young patients or those with a severely altered anatomy.18
The short-term postoperative results are generally good, with high rates of arthrodesis and considerable neurological improvement. Long-term follow-up is essential to detect and treat any complications. There are very few articles showing long-term results, especially beyond 5 years. A study with a follow-up period of over 16 years observed that the most severe long-term complications were instability at the distal level of the instrumentation, conditioning longer fixations to ensure stability, as well as the possibility of appearance of new stenoses caused by kyphotic deformities at the level of the cervicothoracic or thoracolumbar junction.19
ConclusionInvolvement of the spine is a significant cause of disability and death in MPS IVA.
It is important to correlate clinical and neurological findings with imaging studies. MRI is the most useful imaging technique to assess the degree of stenosis and spinal compression. Arthrodesis and decompression are safe and effective surgical interventions for symptomatic patients, but the long-term results are not clear. Patients showing evidence of spinal compression and/or cervical instability, even asymptomatic ones, can be considered for the intervention in order to prevent neurological lesions. Any elective procedure requires meticulous anesthetic planning based on the characteristics of each patient.
Correlating the genotype and phenotype could serve to assess risk, predict results, guide treatment strategies and aid in the design of new therapies. Regarding its compassionate application, the use of recombinant human bone morphogenetic protein-2 in pediatric patients with MPS IVA has been shown to improve the rates of arthrodesis without a need for bone grafts, and leads to ossification of the odontoid.2 There are currently some clinical studies focusing on enzyme replacement therapy which could lead to a treatment option in the future.
Level of evidenceLevel of evidence V.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that this work does not reflect any patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Ruiz-Picazo D, Díez-Ulloa MA. Inestabilidad occipitocervical en la enfermedad de Morquio. Presentación de 2 casos y revisión de la literatura. Rev Esp Cir Ortop Traumatol. 2014;58:387–394.