Pneumocephalus is an uncommon but serious complication of spinal surgery and its management and pathophysiology are not widely recognized. The incidence of symptomatic tension pneumocephalus secondary to posterior spinal arthrodesis is unknown.
Case reportThe case is reported of a rare case of a 41-year-old woman with diagnosis of L3–L4, L4–L5 disc disease and left disc herniation L4–L5. A posterior spinal arthrodesis L3–L5, L3–L4 and L4–L5 discectomies and release of the left L5 root, was performed without apparent complications. Twenty-four hours after surgery the patient developed generalized headache, neck stiffness, and dysarthria. MRI and CT scans revealed a huge pneumocephalus in the subarachnoid space, predominantly in the left frontal lobe without midline shift, which originated in the lumbar spinal canal. The patient was treated conservatively, with progressive neurological improvement after 72h, and clinical and radiological normalization after 7 days.
DiscussionPneumocephalus is a rare but potentially serious complication of spine surgery related in most cases with inadvertent dural tear during the operation. Most collections are small, behave benign, and respond to conservative therapy. In the present case, an inadvertent dural tear, produced a pneumocephalus. A high degree of suspicion is needed to make the diagnosis, prompt treatment, as well as remedying the source of air to prevent unwanted morbidity and mortality.
El neumoencéfalo es una complicación poco frecuente pero grave de la cirugía de la columna vertebral, su manejo y fisiopatología no es ampliamente conocida. La incidencia de neumoencéfalo sintomático a tensión, secundario a una artrodesis vertebral posterior es desconocida.
Caso clínicoPresentamos el caso de una paciente mujer de 41 años de edad, con diagnóstico de discopatía L3-L4, L4-L5 y hernia discal izquierda L4-L5. Se realizó una artrodesis vertebral posterior L3-L5, discectomías L3-L4 y L4-L5 y liberación de la raíz L5 izquierda, sin complicaciones aparentes. Transcurridas 24h después de la cirugía, la paciente inicia cuadro de cefalea generalizada de fuerte intensidad, rigidez de nuca y disartria. Se realizan TAC y RMN que muestran un enorme neumoencéfalo en el espacio subaracnoideo, a predominio del lóbulo frontal izquierdo, sin desplazamiento de la línea media, con origen en el conducto raquídeo lumbar. La paciente fue tratada de forma conservadora, presentando a partir de las 72h mejoría neurológica progresiva, hasta la normalización clínica y radiológica después de 7 días.
DiscusiónEl neumoencéfalo es una complicación rara pero potencialmente grave de la cirugía de columna, relacionada en la mayoría de los casos con desgarro dural accidental durante la cirugía. La mayoría de las colecciones son pequeñas, se comportan de forma benigna, y responden al tratamiento conservador. En un gran número de pacientes, puede comportarse como cualquier lesión ocupante de espacio, por lo que se necesita un alto grado de sospecha clínica para hacer el diagnóstico y tratamiento oportuno, y prevenir la morbimortalidad no deseadas.
Pneumocephalus, also known as intracerebral aerocele or pneumatocele is defined as the presence of gas within any intracranial compartment (intraventricular, intraparenchymatous, subarachnoid, subdural and epidural).1 The first case of pneumocephalus was described by Lecat in 1866, but the term pneumocephalus was first used by Wolff in 1914, to describe this infrequent condition.2,3 Pneumocephalus is generally associated to lesions of the cranial vault following trauma, facial trauma and as a consequence of neurosurgery or otolaryngology procedures for the treatment of skull base tumors. It is infrequent after spinal surgery, and in very few occasions it can appear spontaneously.4 A large number of factors can contribute to the development of pneumocephalus, among them, the position of the head during surgery, the duration of the surgery, the use of nitrous oxide for anesthesia, hydrocephalus, intraoperative osmotherapy, hyperventilation, spinal anesthesia, barotrauma, continuous leak of cerebrospinal fluid (CSF) through a lumbar puncture, epidural anesthesia, infections and neoplasms. The clinical presentation can vary significantly depending on the size and tension of the pneumocephalus, and includes headache, nausea, vomiting, seizing, dizziness and worsening of the neurological condition which may even lead to death.4 In clinical practice it is essential to be able to differentiate a “simple pneumocephalus” from a tension case. The latter refers to a collection of air at a lower pressure than the outer atmospheric pressure, thus creating a valve mechanism that causes the entry of air and prevents it from escaping, establishing a pressure differential and a cascade of adverse effects for the patient.1
The incidence of pneumocephalus secondary to posterior vertebral arthrodesis is unknown. There are few reports published of tension pneumocephalus following vertebral spinal surgery.1–3
Case reportThe patient was a 41-year-old female, with no relevant pathological history, who had been operated at another center in 2007 for an L4–L5 disc herniation affecting the root of the left L5 nerve (L4–L5 lumbar discectomy), who attended our hospital in October 2009 with a history of left L3–L4 radiculopathy since November 2008. We obtained a magnetic resonance imaging (MRI) scan which showed a left posterolateral protrusion of the L3–L4 and L4–L5 discs, which reduced the foraminal space of the left L3 and L4 roots.
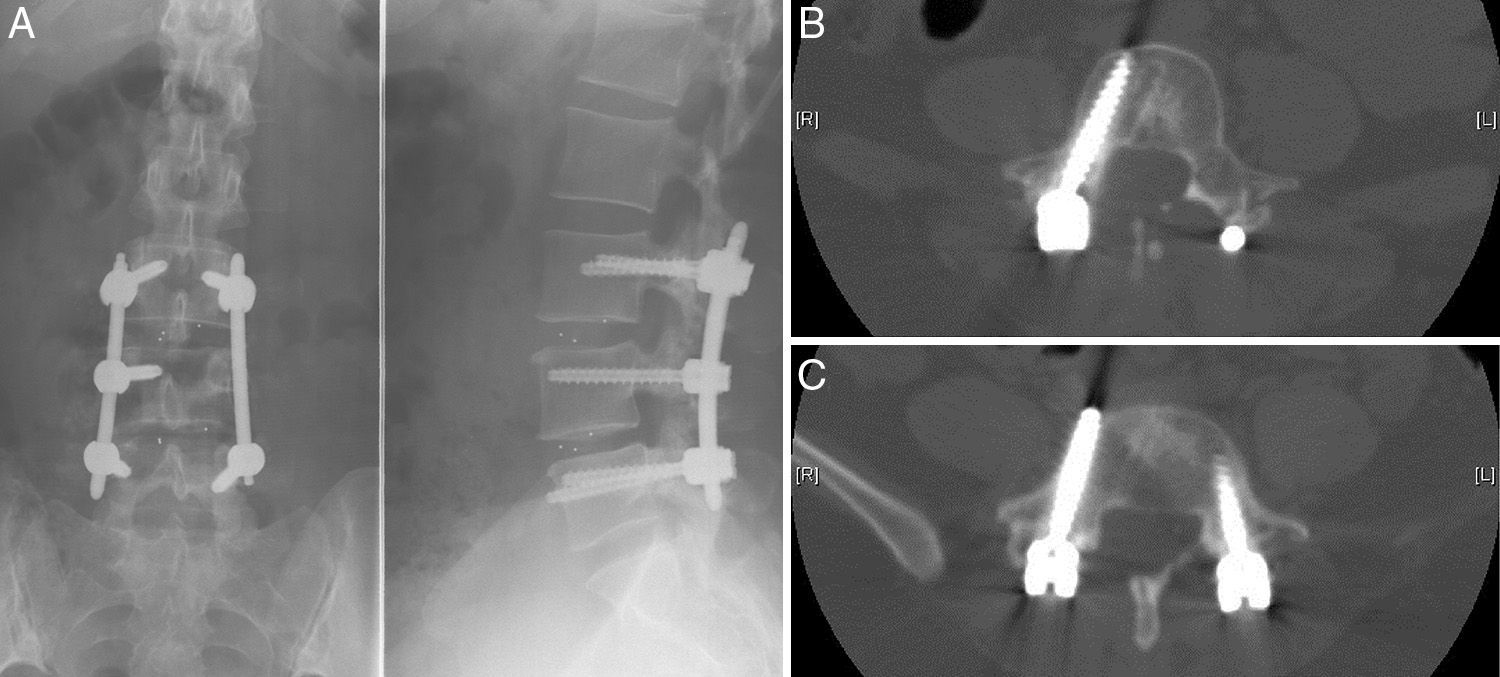
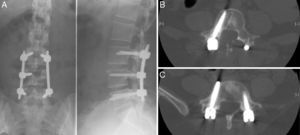
Following this diagnosis we conducted, after a routine preanesthetic evaluation, a posterolateral intersomatic fusion procedure at the L3–L5 levels, with a mini-open approach (percutaneous) on the left side and open procedure on the right side, using two pedicular 6mm×40mm screws in L3, 1 right pedicular 6mm×40mm screw in L4 and two pedicular 6mm×40mm screws in L5 (Fig. 1). There were no apparent complications during surgery. We used a vacuum suction drainage system in the area of the open approach in the surgical field, and observed a mild–moderate loss of fluid with a bloody-aspect from the start of the postoperative period, compatible with the normal evolution of this kind of surgery. The patient recovered without complications in the immediate postoperative period, but presented hypoesthesia and paresis in the right L5 metamere. After 24h, the patient developed an intense and constant frontal and retro-orbital headache, which worsened when standing, accompanied by photophobia, neck rigidity and dysarthria, with no other associated neurological signs and symptoms.
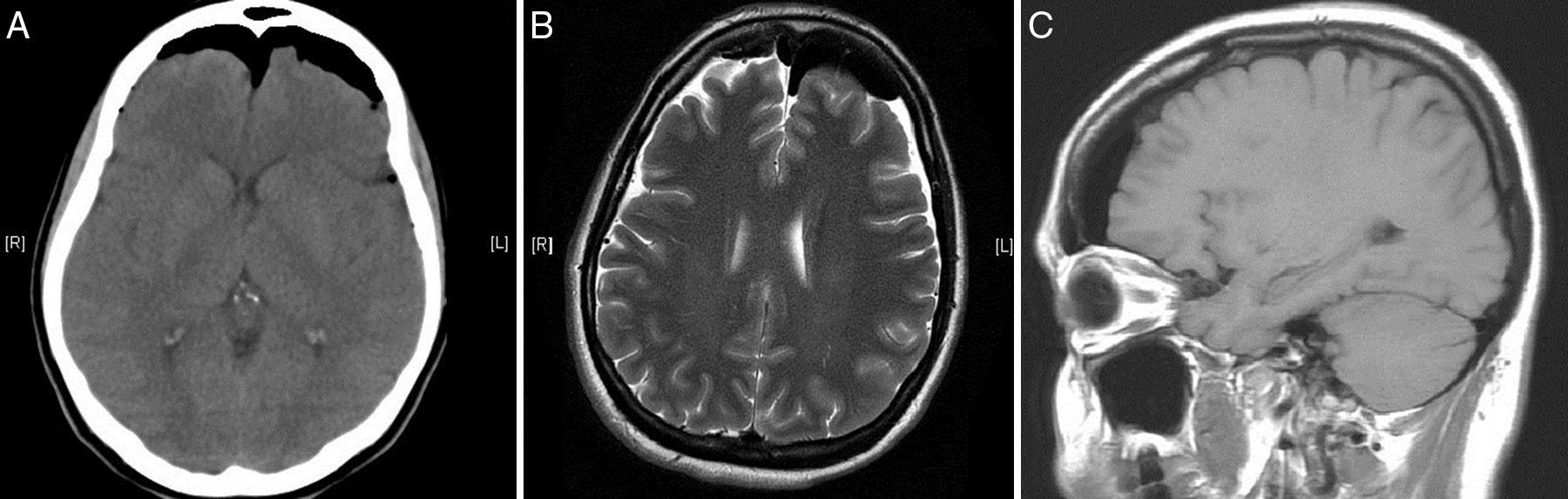
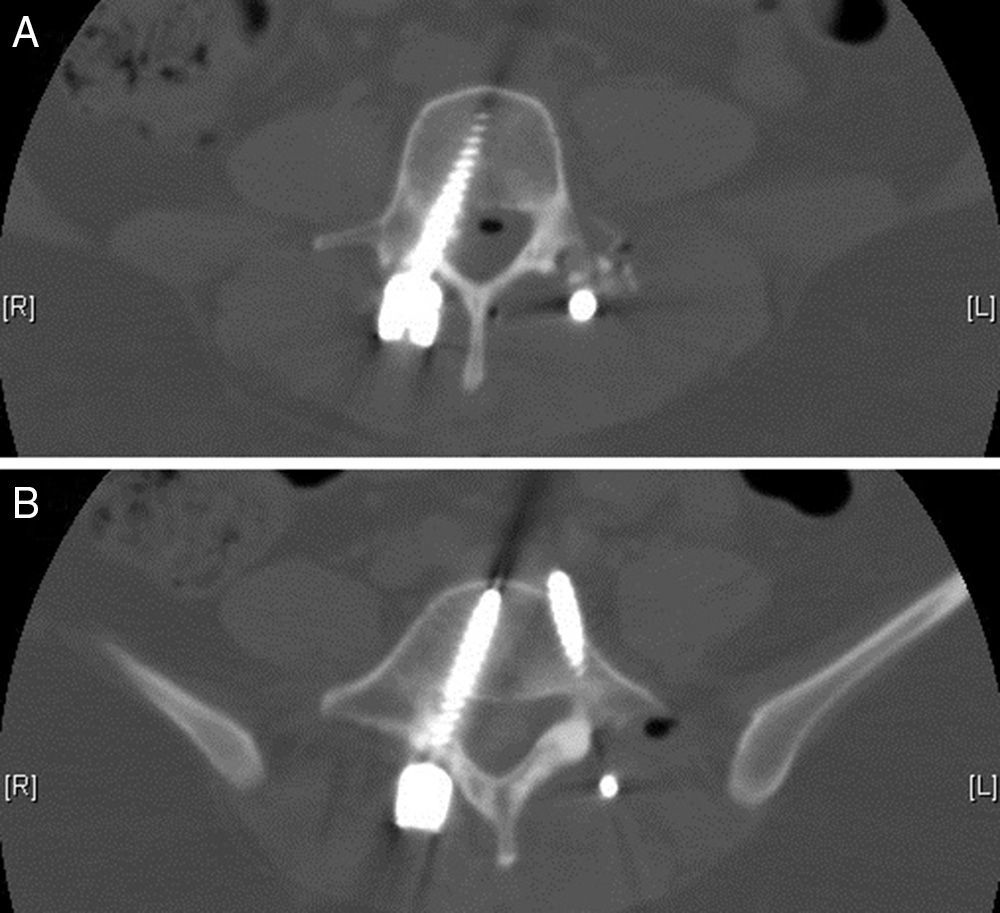
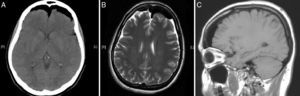
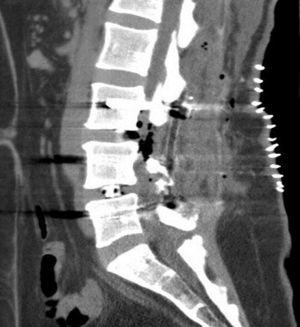
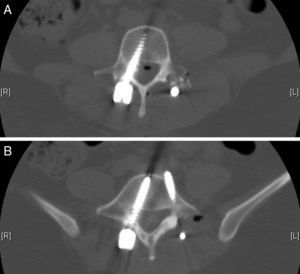
We obtained urgent vertebral spinal and cranial computed tomography (CT) and MRI scans (Figs. 2 and 3), which showed aerial images in the bifrontal subarachnoid space (with left predominance) adjacent to the left medial cerebral artery. The ventricular and cistern system presented a normal size and morphology with no displacement of the midline. No signs of parenchymatous hemorrhage or ischemia were detected. The circle of Willis had permeable vessels with size and morphology within the normal range. There were air bubbles in the epidural space of the lumbar spinal canal, postoperative changes related to L3–L5 fusion, medialization of the right screws of L4 and L5 (Fig. 4), and no evidence of hematomas or significant collections in the surgical field.
The conclusions of the cranial and vertebral spinal CT and MRI were: bifrontal subarachnoid pneumocephalus with left predominance, originating from the lumbar spinal canal; medialization of the right screws of L4 and L5. No anatomical defects were observed that could have caused the pneumocephalus.
TreatmentThe prescribed treatment was bed rest, analgesic and antiemetic drugs and hyperhydration, in addition to interruption of the suction drainage. We conducted continuous neurological evaluation and obtained a new cranial CT, which showed no changes in the first 48h. After 48h, the patient began to show rapid and progressive clinical and radiographic improvement until the full disappearance of the neurological symptoms associated to pneumocephalus after 1 week, with normalization of the imaging studies after 9 days.
Two weeks after recovering, the patient underwent a new intervention, this time under electrophysiological monitoring. Using a right posterior lumbar Wiltse approach we proceeded to remove the right L4 and L5 pedicular screws, and replace them (Fig. 5) under electrophysiological monitoring (two new 6mm×40mm screws), along with right L4–L5 hemilaminectomy and search for signs of dural damage. We found a dural lesion in the right L5 root at the level of the shoulder, approximately 0.5mm in length, which was the origin of the air entry which caused the pneumocephalus, as well as a severe intradural lesion in the right L5 root, with no electrophysiological response, so we proceeded to release it up to an extraforaminal level and seal the dural defect with Tissucol® (Baxter, Illinois, USA) fibrin adhesive. The postoperative period elapsed without incidents. The patient presented a progressive and full recovery of the sensory deficit and a partial recovery of the L5 paresis after 6 months.
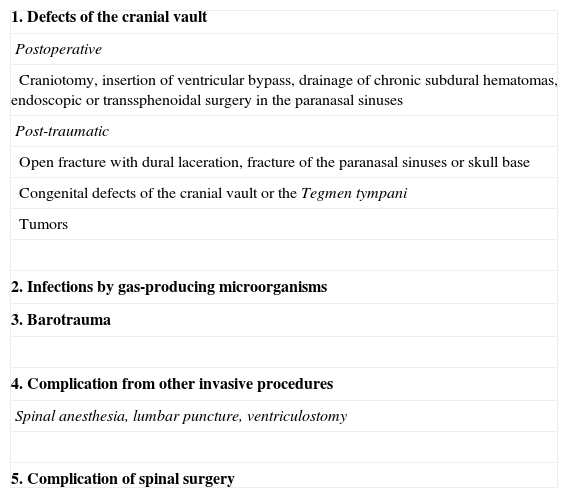
DiscussionA considerable number of etiologies can cause the formation of a pneumocephalus; the most relevant are summarized and classified in Table 1.
Etiology of pneumocephalus.
| 1. Defects of the cranial vault |
| Postoperative |
| Craniotomy, insertion of ventricular bypass, drainage of chronic subdural hematomas, endoscopic or transsphenoidal surgery in the paranasal sinuses |
| Post-traumatic |
| Open fracture with dural laceration, fracture of the paranasal sinuses or skull base |
| Congenital defects of the cranial vault or the Tegmen tympani |
| Tumors |
| 2. Infections by gas-producing microorganisms |
| 3. Barotrauma |
| 4. Complication from other invasive procedures |
| Spinal anesthesia, lumbar puncture, ventriculostomy |
| 5. Complication of spinal surgery |
Craniotomies represent the most frequent cause of this disease. A certain amount of pneumocephalus cases are an inevitable result of this intervention.5,6 Reasoner et al.5 reported that 66% of postcraniotomy CT studies showed between 5% and 10% of the intracranial volume occupied by air in at least 1 axial section of the CT. Although generally asymptomatic, pneumocephalus cases with a larger volume have been linked to symptoms like postoperative lethargy, headache, confusion, hemiparesis and paralysis of the 6th cranial nerve.
Less frequently, pneumocephalus may present as complication of an intervention on or fracture of the paranasal sinuses and skull base, insertion of a ventricular-peritoneal bypass, cranial fractures with dural lacerations, following drainage of subdural hematomas, and as a consequence of different types of tumors in this anatomical region.1,3
Different diagnostic procedures, mostly harmless, such as lumbar puncture, ventriculostomy and spinal anesthesia can cause the passage of air by an intrathecal route and lead to a significant pneumocephalus.7 Barotrauma secondary to rapid changes in air pressure can turn benign, subclinical cases of pneumocephalus into symptomatic of tension pneumocephalus which require urgent treatment and evacuation.8
The reported incidence of postoperative CSF fistulas as a complication of spinal surgery, can reach 5%. However, cases complicated by pneumocephalus are rare and their frequency is unknown.1–3
Pneumocephalus is an infrequent but severe complication of spinal surgery, and its management and physiopathology are not fully known.1–3
In the present case, the physiopathology of pneumocephalus can only be explained by the use of a vacuum drainage system after a posterior lumbar arthrodesis which allowed the passage of air into the subarachnoid space through an iatrogenic dural defect that went unnoticed during surgery. There have been reports of cases in which a drainage system led to the formation of a valve-type mechanism which allowed the entry of air into the cranial/spinal subarachnoid space but prevented its exit, generally among postoperative patients who remained in a decubitus position of over 30°.1
From a technical standpoint, we consider that a hermetic dural closure through different surgical methods, such as the use of fibrin, albumin and collagen tissue adhesives and glutaraldehyde glues, minimizes the risk of this complication.9,10
In common clinical practice, pneumocephalus with a spinal origin is usually associated to fractures caused by a spinal trauma, penetrating lesions, tumors, infections or iatrogenic causes, including, as previously mentioned, certain diagnostic and therapeutic methods.7
In the majority of patients with pneumocephalus, a conservative treatment, consisting in bed rest, hyperhydration, analgesics, sedatives and antiemetics, is normally sufficient, and the symptoms are progressively resolved after 1–3 weeks.1–3
ConclusionsPneumocephalus is a rare but potentially severe complication of spinal surgery, in most cases related to accidental dural tear during surgery. The majority of these air pockets are small, behave benignly, and respond to conservative therapy. However, in some cases they may behave as any other space-occupying lesion. A high degree of clinical suspicion is required to establish the correct diagnosis and treatment, avoiding the progression of the collection, and thus preventing unwanted morbidity and mortality.
The complex field of spinal surgery has found it particularly difficult to reach a constructive consensus describing these undesired and unforeseen events, which appear during or after the surgical intervention. We consider it extremely important to make further efforts to understand the physiopathology of the complications of spinal surgery, thus minimizing their incidence, and to disseminate their knowledge.
Level of evidenceLevel of evidence V.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Please cite this article as: Andarcia-Bañuelos C, Cortés-García P, Herrera-Pérez MU, Deniz-Rodríguez B. Neumoencéfalo: una inusual complicación de la artrodesis lumbar. Caso clínico y revision de la literatura. Rev Esp Cir Ortop Traumatol. 2015;59:222–226.