To study postoperative complications of arthroscopic anterior cruciate ligament (ACL) reconstruction performed as an outpatient compared with same surgery performed as a regular admission (inpatient).
Material and methodA study was conducted on a historical cohort of 342 patients (115 outpatients vs 227 inpatients) who underwent arthroscopic ACL primary ligamentoplasty (2004–2012). A review was performed on the demographic, surgical and hospital variables. A study was made of early complications (60 days postoperative) including visits to emergency department and readmissions. A descriptive and bivariate distribution analysis was performed between groups, with the grouping criterion: performing of the surgery with or without admission. The Chi-square test was used for qualitative variables and Mann–Whitney U test for quantitative. Limit significance P<0.05.
ResultsOverall, there were 13.2% emergency department visits (mean of 1.24 visits) with an average delay of 8.22 days after discharge. Complications: pain not controlled with analgesia (6.7%), hemarthrosis that required arthrocentesis (4.4%), fever (3.2%), deep vein thrombosis (0.6%), cellulitis (0.6%), septic arthritis that required arthroscopic debridement (0.3%), and others (1.2%) including problems with immobilization. The hospital readmissions (2.3%) were for surveillance and monitoring of the surgical wound. In the bivariate analysis no statistically significant differences were found between groups as regards the sociodemographic characteristics of the patients or the complications recorded.
DiscussionThe most frequent complications recorded were acute pain, hemarthrosis and fever. Serious complications (deep vein thrombosis, septic arthritis or need for hospital readmission) were rare.
Outpatient arthroscopic ACL repair is a common technique that can be performed safely by surgery without admission, with an overall low complication rate with no differences between outpatients and inpatients.
Estudiar las complicaciones postoperatorias de la ligamentoplastia artroscópica del LCA realizada ambulatoriamente (CMA) comparándola con la realizada mediante hospitalización (no-CMA).
Material y métodoCohorte histórica sobre 342 pacientes (115 CMA vs. 227 no-CMA) intervenidos de ligamentoplastia primaria artroscópica del LCA (2004–2012). Revisión de variables sociodemográficas, quirúrgicas y de hospitalización. Estudio de complicaciones precoces (primeros 60 días) incluyendo visitas a urgencias hospitalarias y reingresos. Análisis descriptivo y bivariado de distribución entre grupos: realización de la técnica en CMA o no. Test Chi-Cuadrado para variables cualitativas y test U-Mann–Whitney para cuantitativas. Límite significación P<0,05.
ResultadosUn 13,2% de visitas a urgencias (media de 1,24 visitas), demora media de 8,22 días tras el alta. Complicaciones: dolor no controlado con analgesia (6,7%), hemartros a tensión precisando artrocentesis evacuadora (4,4%), sensación febril (3,2%), trombosis venosa profunda (0,6%), celulitis (0,6%), artritis séptica con desbridamiento artroscópico (0,3%) y otras (1,2%) como problemas con la inmovilización. Un 2,3% de ingresos para vigilancia y seguimiento de la herida quirúrgica. En el análisis bivariado no se encontraron diferencias estadísticamente significativas entre ambos grupos en las características sociodemográficas de los pacientes ni en las complicaciones registradas.
DiscusiónLas complicaciones más frecuentes registradas fueron el dolor agudo, el hemartros y la sensación febril. Las graves (trombosis venosa profunda, artritis séptica o necesidad de reingreso hospitalario) fueron excepcionales.
La CMA de reparación artroscópica del LCA es una técnica frecuente que se puede realizar de forma segura mediante cirugía sin ingreso hospitalario con una tasa global de complicaciones bajas sin diferencias entre hospitalización o sin ingreso.
Surgical repair of the anterior cruciate ligament (ACL) is a common technique at most traumatology and orthopedic surgery services throughout the western world, as well as a highly cost-effective intervention.1
Although the surgery has evolved considerably in recent years, it is not without complications since, at present, around 5–9% of patients suffer some kind of iatrogenic problem.2 The current trend is toward performing the technique without hospital admission, that is, with less than 12h of hospital stay (outpatient surgical procedure, OSP), although there is not enough evidence in the literature regarding its safety compared to performing it with hospital admission (non-OSP). The advantages of carrying out OSP procedures in traumatology and orthopedic surgery which have traditionally been associated to hospital admission are manifold and include an improvement in perceived health (SF-36), cost savings and a lower rate of complications and readmissions.3
Our hypothesis is that the technique we implemented many years ago at our department (ligamentoplasty of the ACL by OSP) is safe and provides similar results in terms of the most frequent complications compared to the technique conducted through non-OSP.
Since we found some unresolved questions in the current literature on this topic, the present work aims to analyze: (1) the overall complications of arthroscopic ligamentoplasty of the ACL in our environment and (2) the differences between performing the technique through OSP or not in terms of the frequency of complications and visits to the emergency service after the surgery.
Material and methodsAfter obtaining approval from the Ethics Committee of our center, we conducted a retrospective assessment of all the patients intervened for ligamentoplasty of the ACL at our department between January 2004 and September 2012. We included all those patients who underwent programmed arthroscopy with a prior diagnosis of ACL tear, excluding patients aged under 15 years or over 50, arthroscopies for revision of prior ACL surgery and patients with a follow-up of complications under 8 weeks. We recorded the age, gender, Charlson comorbidity index,4 surgical technique, associated procedures, readmissions and complications. We evaluated the early postoperative complications of all patients 60 days after the intervention, dividing them into 2 historic cohorts depending on whether they had been treated through OSP or non-OSP. We initially included 368 patients, but subsequently excluded 13 patients due to review surgery, 12 due to their age (4: <15 years and 8: >50 years) and 1 due to lack of adequate follow-up (returned to home country). The remaining 342 patients formed the basis of the final analysis.
Surgical technique5In all cases, patients were admitted on the same day of the intervention and the anesthesia used in all patients was spinal, although in 16 cases (7 OSP and 9 non-OSP) it was combined with laryngeal intubation. All received preoperative antibiotic prophylaxis with a 2g bolus of intravenous cefazolin (or 1g intravenous vancomycin if there was a history of adverse reaction to penicillin and/or derivatives). The standardized position consisted in the supine position, with the knee at 90° flexion on a thigh support and a proximal ischemia cuff inflated to 300mmHg. An explorative arthroscopy was conducted through anteroexternal portals for the 30° optics and anterointernal portals for the surgical instrumentation. The tendons of the semitendinosus (St) and gracilis (G) muscles were extracted through a longitudinal approach on the ipsilateral goose foot with proximal disinsertion using a “stripper” type tenotome and distally by separation from the tibial insertion, plaiting in 4 fascicules with slow-absorption polyglactin 910 reabsorbable suture (Vicryl, Ethicon, NJ, USA) double zero in the proximal and distal ends. An ipsilateral bone-tendon-bone technique was used in cases where the plasty was not satisfactory according to the judgment of the surgeon. Tunneling (single tunnel technique) and introduction of the plasty was conducted through the Crosspin® system (Stryker, Kalamazoo, MI, USA). Bioresorbable, atraumatic, interferential Biosteon® screws (Stryker, Kalamazoo, MI, USA) were used in all cases. Any necessary associated procedures (meniscal suture or regularization, synovectomy and microfractures) according to the diagnosis of the surgeon and findings of the exploratory arthroscopy were performed in the same surgical action.
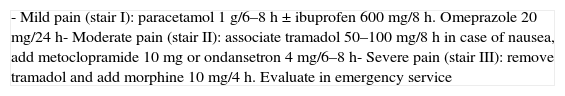
Management upon medical discharge and postoperativelyThe discharge criteria employed were: patients presenting controlled pain with conventional oral analgesia (VAS<5) without requiring the use of potent morphine agents, with a clean bandage with no evidence of bleeding, independence for personal hygiene and capable of walking autonomously with the aid of canes; the remaining criteria are detailed in Table 1. The analgesia prescribed upon discharge was the same in all cases, with some individual adjustments in each case according to the concomitant pathologies and allergies of each patient, and consisting in the systematic application of the therapeutic pain ladder of the WHO adapted to the most common traumatology and orthopedic surgery procedures and agreed with the Pharmacy Service of our hospital (Table 2). In general, patients were discharged 24h after the intervention, after removing the drainage in those cases where it had been necessary, or else on the same day of the surgery if no drainage was needed.6,7 Prophylaxis with low molecular weight heparin was maintained during a maximum of 3 weeks after the intervention, according to the protocol of the hospital, generally removing the treatment at the time that patients began their mobilization exercises.
OSP discharge criteria in traumatology and orthopedic surgery.
| - Independence to walk with crutches- Spontaneous urination- Pain controlled with analgesia (VAS<5). Secured airway- Tolerance to liquids and food without nausea and vomiting- Clean bandage with no evident bleeding- Conscious and oriented (GSC 15/15)- Sufficient home care guaranteed by a family member or caregiver- Understanding the instructions in case of emergency |
Analgesia upon OSP discharge in traumatology and orthopedic surgery.
| - Mild pain (stair I): paracetamol 1g/6–8h±ibuprofen 600mg/8h. Omeprazole 20mg/24h- Moderate pain (stair II): associate tramadol 50–100mg/8h in case of nausea, add metoclopramide 10mg or ondansetron 4mg/6–8h- Severe pain (stair III): remove tramadol and add morphine 10mg/4h. Evaluate in emergency service |
All patients were given postoperative education on basic care after the surgery and were recommended, according to the protocol of the Department of Traumatology and Orthopedic Surgery, to attend the Emergency Service of the hospital or contact the Department by telephone, instead of attending extrahospital centers or their primary care physicians for the evaluation of any possible complications.
Subsequently, a functional orthesis was used on the knee, with limitation of flexion–extension and authorizing immediate partial load with canes if there was no contraindication due to the associated technical procedures. A physiotherapy program in the gym was started 7–10 days after the surgery. All the patients were evaluated 2 weeks after the intervention with the removal of the cutaneous suture and placement of elastic bandage. A new clinical evaluation was conducted after 1, 3, 6 and 12 months.
Data collectionThe database used for the digital clinical history was the program HP Doctor® (Hewlett Packard, Palo Alto, CA, USA).
The clinical history was reviewed during the first 60 postoperative days, along with the report of the visit to the Emergency Service in case the patient had attended it, and all the reports for the first visit, at 2 weeks and 1 month, detailing postoperative condition of the joint (diagnosis of tension hemarthrosis under the criteria of the emergency service physician or traumatologist in consultation), aspect of the surgical wound and/or poor pain control; in all cases a new intervention was conducted by the physician or traumatologist who attended the patient, consisting in an evacuative arthrocentesis and weekly review in the case of hemarthrosis, close monitoring of the surgical wound if there was an alteration and a modification of the analgesic treatment in case of uncontrolled pain. Other variables, such as readmissions and the need for debridement surgery, were also recorded.
Statistical analysisIn order to confirm the statistical power of the study we estimated a prevalence according to previous works of 5% of complications,8 for a 95% confidence level and a precision of 3% a total of 128 patients were required. We decided to select the entire available population since a second main objective was studied (percentage of visits to the Emergency Service).
A descriptive statistical analysis was conducted with the software package SPSS® v.15 (IBM Chicago, IL, USA) using central tendency and dispersion measurements for quantitative variables and distribution of frequencies for qualitative variables, a bivariate distribution analysis between groups with the grouping variable being performance of an OSP or non-OSP technique. We used the Chi-squared test for qualitative variables and the Mann–Whitney U test for quantitative variables. The limit of statistical significance was established at P <.05.
ResultsA total of 342 patients were included in the final analysis. Table 3 details the sociodemographic characteristics and overall complications of the population. A total of 87.7% were males, the mean age was 29.86 years and 87.13% of patients had no comorbidities according to the Charlson index. In 92.1% of patients, the ligamentoplasty was performed using an autologous graft from the ipsilateral goose foot (semitendinosus, gracilis), whilst an ipsilateral bone-tendon-bone technique was used in the remaining cases (7.9%). Fig. 1 shows the proportion of patients who were intervened by OSP or non-OSP over the studied years.
Descriptive analysis. Complete series.
| Total (n=342) | |
|---|---|
| Gender | |
| M | 300 (87.7%) |
| F | 42 (12.3%) |
| Age (years) | 29.86 (σ 8.9) |
| Charlson | |
| 0 | 298 (87.13%) |
| 1 | 32 (9.4%) |
| ≥2 | 12 (3.5%) |
| Technique | |
| StG | 315 (92.1%) |
| BTB | 27 (7.9%) |
| Emergency service | |
| Attended | 45 (13.2%) |
| Average number of visits | 1.24 |
| Delay (days) | 8.22 |
| Associated procedures | 91 (26.6%) |
| Meniscectomy | 49 (14.3%) |
| Meniscal suture | 23 (76.7%) |
| Synovectomy | 8 (2.3%) |
| Microfracture | 4 (1.2%) |
| Complications | |
| Readmission | 8 (2.3%) |
| Hemarthrosis | 15 (4.4%) |
| Pain | 23 (6.7%) |
| Debridement | 1 (0.3%) |
| Cellulitis | 2 (0.6%) |
| Fever | 11 (3.2%) |
| DVT | 2 (0.6%) |
| Others | 4 (1.2%) |
BTB: bone-tendon-bone; DVT: deep vein thrombosis; F: females; M: males; StG: semitendinosus–gracilis.
σ: standard deviation.
Out of the total patients monitored during the first 60 days after the surgery, 45 (13.2%) attended the emergency service, with a mean 1.24 visits per patient (11 patients attended 2 times and none attended more than 2) and a mean delay of 8.22 days. The most common complications were pain uncontrolled with analgesia in 23 patients (6.7%), tension hemarthrosis requiring evacuative arthrocentesis in 15 patients (4.4%), sensation of fever in 11 patients (3.2%), deep vein thrombosis in 2 patients (DVT) (0.6%), cellulitis in 2 patients (0.6%), septic arthritis requiring arthroscopic debridement in 1 patient (0.3%) and others in 4 patients (1.2%), including problems with immobilization. A total of 8 patients (2.3%) required hospital readmission for monitoring and follow-up of the surgical wound.
Out of the 342 patients, 115 were treated by OSP and 227 by non-OSP. Regarding the sociodemographic distribution between both groups (Table 4) we did not find any differences in terms of gender (84.3% vs 84.3% males), age (29.31 vs 30.14 years), comorbidities according to the Charlson index (90.4% vs 85.5%) and technique used in favor of semitendinosus–gracilis (93.9% vs 91.2%). The distribution of associated procedures (25.2% vs 27.5%) was similar between both groups with a proportion of meniscectomies (13.9% vs 14.5%), meniscal sutures (7.8% vs 6.2%), synovectomies (1.7% vs 2.64%) and microfractures (1.7% vs 0.9%) with no significant differences.
Bivariate analysis. Comparison between groups.
| OSP (n=115) | non-OSP (n=227) | P | |
|---|---|---|---|
| Gender | 0.405 | ||
| M | 97 (84.3%) | 203 (84.3%) | |
| F | 18 (15.7%) | 24 (15.7%) | |
| Age (years) | 29.31 (σ 9.4) | 30.14 (σ 8.5) | 0.404 |
| Charlson | 0.465 | ||
| 0 | 104 (90.4%) | 194 (85.5%) | |
| 1 | 9 (7.8%) | 23 (10.1%) | |
| ≥2 | 2 (1.7%) | 10 (4.4%) | |
| Technique | 0.378 | ||
| StG | 108 (93.9%) | 207 (91.2%) | |
| BTB | 7 (6.1%) | 20 (8.8%) | |
| Emergency service | |||
| Attended | 15 (13%) | 30 (13.2%) | 0.964 |
| Number of visits | 1.4 | 1.17 | 0.200 |
| Delay (days) | 13.13 | 5.77 | 0.090 |
| Associated procedures | 29 (25.2%) | 62 (27.5%) | 0.235 |
| Meniscectomy | 16 (13.9%) | 33 (14.5%) | |
| Meniscal suture | 9 (7.8%) | 14 (6.2%) | |
| Synovectomy | 2 (1.7%) | 6 (2.64%) | |
| Microfracture | 2 (1.7%) | 2 (0.9%) | |
| Complications | |||
| Readmission | 2 (1.7%) | 6 (2.6%) | 0.601 |
| Hemarthrosis | 5 (4.3%) | 10 (4.4%) | 0.980 |
| Pain | 10 (8.7%) | 13 (5.7%) | 0.300 |
| Debridement | 0 (0%) | 1 (0.4%) | 0.476 |
| Cellulitis | 0 (0%) | 2 (0.9%) | 0.313 |
| Fever | 4 (3.5%) | 7 (3.1%) | 0.845 |
| DVT | 1 (0.9%) | 1 (0.4%) | 0.623 |
| Others | 0 (0%) | 4 (1.8%) | 0.152 |
BTB: bone-tendon-bone; DVT: deep vein thrombosis; F: females; M: males; OSP: outpatient surgical procedure; StG: semitendinosus–gracilis.
σ: standard deviation.
Regarding the complications registered, in the OSP group we found 2 patients who required readmission (1.7%), to monitor the surgical wound in 1 case (0.4%) and due to DVT in the other case (0.4%), whilst in the non-OSP group there were 6 readmissions (2.6%) of which 2 were to monitor the surgical wound (0.9%), 2 due to fever without a focus (0.9%), 1 due to DVT (0.4%) and 1 due to acute infection (0.4%) requiring reintervention for arthroscopic debridement with positive culture of Staphylococcus aureus with preservation of the plasty and a good clinical and functional result. In total, 10 patients (8.7%) in the OSP group and 13 in the non-OSP group (5.7%) reported poor control of postoperative pain at some point, requiring a significant increase of analgesia. Five (4.3%) and 10 (4.4%) patients respectively presented postoperative hemarthrosis with evacuative arthrocentesis, diagnosed either on the first visit or upon attending the emergency service. Four (3.5%) and 7 (3.1%) patients attended the emergency service reporting fever sensation, with only 2 patients in the non-OSP group (0.9%) requiring admission for this reason. Other complications were registered in 4 patients (1.8%), all in the non-OSP group, and including problems with the bandage (2, [0.9%]), doubts about the evolution (1 [0.4%]) and loss of monitoring in outpatient clinic (1 [0.4%]). No statistically significant differences between the groups were found when the distribution of complications was analyzed (Table 4).
DiscussionSurgical repair of the ACL is a very common technique at most traumatology and orthopedic surgery services, as well as a highly cost-effective intervention,1 albeit not without complications, with around 5–9% of iatrogenic problems.2 Since there is insufficient evidence in the literature about its safety in terms of performing it by OSP or with hospital admission, this work has attempted to study the complications of patients intervened at our department.
The most common complications following ACL ligamentoplasty recorded in the recent literature2,8 include readmission (1.36–2.3%), complications of the surgical wound (0.75%), DVT (0.44%), septic arthritis (0.14–1.7%),9 and reintervention (0.25%), although no data relating to emergency reevaluations were obtained.
In our work, the most commonly observed complications were pain in 23 patients (6.7%) and hemarthrosis in 15 (4.4%). We believe that these could be avoidable and, undoubtedly, knowledge of their frequency will help us to insist on the management of postoperative pain, exhaustive hemostasis during surgery and informing patients about severe symptoms. Acute infection is an infrequent, albeit feared complication. We agree with Parrón et al.9 who proposed that early arthroscopic lavage and debridement along with specific antibiotic treatment represent the basis of the initial treatment of acute infections following repair of the ACL, so that recurrence can be prevented in the majority of cases and the plasty can be maintained with a good final result. In our experience, we have only diagnosed 1 patient (0.3%), who could be treated through arthroscopic debridement, preserving the plasty and achieving a satisfactory resolution of the infection, and who is currently clinically free of infection and with good functionality. DVT is a severe and infrequent complication. In our work it accounted for 0.6%, thus confirming the effectiveness of preventive treatment with low molecular weight heparin. In any case, the fact that there were more complications due to bleeding (hemarthrosis) than to DVT (no cases of pulmonary thromboembolism) leads us to think that, as is the case with hip and knee arthroplasty surgeries, further evidence studies would be necessary which allowed us to evaluate the safety of other, less potent antiaggregants and anticoagulants for arthroscopic knee surgery, so as to prevent DVT and decrease the risk of bleeding. Regarding the proportion of readmissions registered, it is worth commenting that only 8 patients out of the total 342 required readmission (2.3%). Moreover, we believe that the only necessary admission was that of the patient requiring reintervention. In the remaining cases suffering postoperative complications who were readmitted (monitoring of the surgical wound in 3 patients, DVT in 2 patients and fever with no focus in 2 patients), management could have been optimized by proposing a close review in outpatient clinic. We believe it worth noting that 11 of the 45 patients (24.4%) who attended the emergency service had to return due to lack of response to treatment. In the majority of cases (8 patients) the reason for attending the emergency service was the lack of response to the analgesic treatment prescribed, whilst in the rest it was due to persistence of fever (2 patients) and lack of control of pain with a diagnosis of hemarthrosis (1 patient). This proves that the management of pain conducted in the emergency service may not have been the most adequate, since a high percentage of cases returned.
In the USA, the number of arthroscopic procedures conducted on the knee between 1996 and 2006 increased by 49%, going from 15% conducted in OSP in 1996 to 51% in 2006.10 In England, only 20% of the arthroscopic repairs of the ACL were conducted without admission.8 In other countries, like Spain, the prevalence of ACL reconstructions without hospital admission is unknown. In our series, 33% of cases in the past 8 years have been performed by OSP, although this tendency is increasing and in 2012 ACL repairs in OSP accounted for 82% of the total.
The advantages of OSP in traumatology and orthopedic surgery have been studied for many years.11,12 The most notable are economic savings through the costs derived from the intervention13 and higher patient satisfaction,14 with no significant increase in overall complications and readmissions. In recent works, health perception by patients (SF-36) also seemed to be higher.3
In a study of 96 cases of ACL reconstruction conducted by OSP, although without a non-OSP control group, García-Casas et al.15 concluded that the procedure can be performed with similar levels of safety and effectiveness to the technique with admission in addition to establishing savings of 7.9% (436.16€ per procedure). Shaw et al.16 and Kumar et al.17 also established the safety of the technique after analyzing series of cases undergoing outpatient ACL reconstruction. In a work with 46 patients (25 OSP and 21 non-OSP) Kao et al.18 established the viability of the outpatient technique compared to hospitalization. In a work with 40 patients (21 OSP and 19 non-OSP) Krywulak et al.14 concluded that ACL interventions by OSP provided greater patient satisfaction, as did Khan et al.19 in a work with 50 patients in each group.
The published works14–19 present small series; we only found 3 comparative studies,14,18,19 and none of them conducted a comparative analysis of the complications. In addition, the statistical power of all the studies reviewed did not enable conclusions to be extracted with certain evidence on the safety of ACL ligamentoplasty by OSP, since, being a technique with a low incidence of overall complications, studies with a larger number of cases (more than 128 according to our calculations) would be required in order to observe differences over 3% between groups. We believe that this limitation detracts from the conclusions of previously published works (Table 5).
Comparison of the complications of surgery to repair the ACL through outpatient arthroscopy.
| N | Control group (n) | Age (range) | Pain | Readmission | Reinterventions | |
|---|---|---|---|---|---|---|
| Kao et al., 199518 | 25 | 21 | 28 (22–34) | 35.7% (5) | 8% (2) | 0% (0) |
| Kumar et al., 200117 | 20 | – | (20–37) | – | 0% (0) | – |
| García-Casas et al., 200415 | 96 | – | 26.6 (17–52) | 11.6% (11) | 4.2% (4) | 2.1% (2) |
| Krywulak et al., 200514 | 21 | 19 | 27.1 (15–45) | – | – | – |
| Shaw et al., 200516 | 102 | – | – | – | 0.9% (1) | – |
| Khan et al., 201219 | 50 | 50 | 28.3 | 3% (6) | – | – |
| Andrés-Cano et al., 2014 | 115 | 227 | 29.3 (15–56) | 6.7% (23) | 1.8% (2) | 0.3% (1) |
The present work compares 2 extensive cohorts of patients undergoing reconstruction of the ACL (n=342; 115/227) with homogeneity in terms of technique and conducted by the same surgical team, with high reliability and scarce loss of minimum information thanks to the digital clinical history and conducting a complete analysis of acute complications after the surgery. We believe that this represents the main strength of the study. Nevertheless, our work presents some limitations. The analysis of the associated procedures during the surgery (meniscectomies, meniscal sutures, synovectomies and microfractures) which could have influenced the complications (hemarthrosis, acute pain…) could not be stratified because the sample size would have made it invalid; nevertheless, the distribution was homogeneous, as seen in Table 4. Patient satisfaction was another aspect to take into account in our medium and which could not be analyzed, mainly due to the retrospective nature of the study and the long period involved (2004–2012). For all these reasons, we were not able to gather this information by contacting patients with sufficient guarantee of avoiding a memory bias. Moreover, when collecting the information using existing computer databases, we were not able to obtain sufficient data regarding other variables which would have been interesting to analyze, such as surgical time, locoregional anesthetic blocks, functional results and variables which could have influenced the real complications (mainly visits to emergency service, distance and ease of access to the hospital center). Nevertheless, it would be acceptable to think that these variables also had a homogeneous distribution between the groups, as the entire population received the same treatment and postoperative information (attending emergency services or contacting the Traumatology and Orthopedic Surgery service instead of the primary care physician).
The cost and consequent savings per intervention were not analyzed, since in addition to not being an aim of the study, we believe that its true analysis is complex. García-Casas et al.15 proposed savings of 436.16€ for each intervention. In our opinion, the calculation should add the fact that the costs deriving from the procedure do not only depend on the savings obtained from the non-admission of patients at the Orthopedic Surgery wing and reduced pharmacy costs, but also on the possibility of freeing up resources to conduct other, more complex interventions, with the consequent overall optimization of surgical activity. This would require a very detailed study. In addition, the economic results are difficult to extrapolate to other services due to the considerable variability existing between centers depending on the type and volume of activity.
We could also consider as a methodological problem the fact that patients in the hospitalization group were mostly treated with a postoperative drainage. Although this procedure is no longer recommended routinely in the literature,5,6 it is a variable that differs between both groups. Nevertheless, this fact would have been significant if the conclusion had been the alternative hypothesis, instead of the null as was ultimately the case. Another limitation to take into account is that, probably, a percentage of cases in the non-OSP group were patients who were initially intervened by OSP (particularly in the later years of the work), but who had to remain at the hospital overnight after not fulfilling all the OSP discharge criteria. In our opinion, pain control and home care were the main reasons for delaying discharge in that group of patients, in which, although we do not have all the information available, we estimate these represent less than 5%.
This work, as well as the recent literature, has confirmed that arthroscopic surgery of the ACL has a low rate of complications. We believe that further works are required to enable us to identify the preoperative risk factors in ACL surgery20,21 which could recommend conducting the procedure by OSP or not. We recommend emphasizing the multimodal management of postoperative pain by using locoregional blocks,22 as well as early diagnosis and treatment of postoperative hemarthrosis which could compromise the functional results.23 Collaboration of multidisciplinary teams and involving non-medical healthcare staff in the process of arthroscopic ligamentoplasty of the ACL by OSP are essential.
We believe that the clinical data obtained through the present work could provide information to patients who will be intervened, as well as contribute to the overall optimization of the procedure. In addition, it can serve as a basis for subsequent studies with more evidence which analyze questions that remain unresolved, such as the identification of risk factors, satisfaction in our environment and the possible influence of OSP on the functional results.
In conclusion, we highlight the safety of arthroscopic surgery to repair the ACL conducting the technique by OSP, being a major surgery with a low rate of overall complications that is not increased or decreased by the fact that patients are intervened through OSP or not. In our environment, the most common complications were acute pain (6.7%), postoperative hemarthrosis (4.4%) and sensation of fever (3.2%). In the analyzed series, severe complications (DVT, septic arthritis and need for hospital readmission) were exceptional, with a rate below 1%.
Level of evidenceLevel of evidence III.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Andrés-Cano P, Godino M, Vides M, Guerado E. Complicaciones de la reparación artroscópica del ligamento cruzado anterior sin ingreso hospitalario. Rev Esp Cir Ortop Traumatol. 2015;59:157–164.