The aim of the study was to evaluate the clinical and radiological results obtained in the treatment of carpal scaphoid non-union treated at the University Hospital of Valladolid using the Fisk-Fernández technique.
Materials and methodsA review was performed on 43 cases of surgically treated non-union using Fisk-Fernández technique with a minimum of 6 months follow-up. The time until surgery, previous treatment, the mechanism of injury, type of non-union, and the existence of radio-carpal arthrosis were evaluated.
A subjective evaluation was performed using the “Scaphoid Score” and the DASH, plus an objective assessment with the modified Green & O’Brien, together with the measurement of the intra-scaphoid, radioulnar, scapholunate angles, and carpal height.
ResultsThe median time to healing in the series was between 16 and 24 weeks, except in 3 patients who failed to heal and required salvage surgery.
There was a statistically significant variation between the preoperative and postoperative angles and carpal height measured in the X-rays.
DiscussionThere are different osteosynthesis techniques and materials for the treatment of non-union. The evaluation of results performed using objective and subjective scales showed variable results between studies.
Different techniques are aimed at preventing the progression of the disease.
ConclusionThe Fisk-Fernández technique enables the deformity of the scaphoid to be corrected by wedge grafting and internal fixation with Kirschner wires or screws.
Valorar los resultados clínicos y radiológicos obtenidos en el tratamiento de la seudoartrosis de escafoides del carpo inestable en los pacientes tratados en el Hospital Clínico Universitario de Valladolid con la técnica de Fisk Fernández.
Material y métodoRevisión de 43 casos de seudoartrosis intervenidos quirúrgicamente mediante técnica de Fisk Fernández, con un seguimiento mínimo de 6 meses, en la que se han valorado el tiempo hasta la intervención quirúrgica, el tratamiento previo, el mecanismo de lesión, tipo de seudoartrosis y la existencia de artrosis radio-carpiana.
Hemos realizado una evaluación subjetiva utilizando el cuestionario Scaphoid Score y el DASH y una valoración objetiva mediante la escala modificada de Green & O¿Brien, junto con la medida de los ángulos intraescafoideos, radiolunar, escafolunar y la altura del carpo.
ResultadosEn nuestra serie el tiempo medio hasta consolidación fue entre 16-24 semanas, excepto en 3 pacientes que no consolidaron y precisaron cirugías de rescate.
La variación entre los ángulos y la altura pre y postoperatorios del carpo medidos en las radiografías muestra que esta diferencia ha sido estadísticamente significativa.
DiscusiónExisten diferentes técnicas y materiales de osteosíntesis para el tratamiento de la seudoartrosis. La evaluación de resultados se realiza con escalas objetivas y subjetivas mostrando resultados variables entre estudios.
Las diferentes técnicas van encaminadas a evitar la progresión de la enfermedad.
ConclusiónLa técnica de Fisk Fernández permite la corrección de la deformidad del escafoides, mediante injerto en cuña y la osteosíntesis con agujas de Kirschner o tornillos.
The carpal scaphoid bone acts as the link between the proximal and distal rows of the carpus, making it a key element in wrist kinematics.
This bone has a complex three-dimensional structure composed by cancellous bone surrounded by cartilage in 80% of its surface.
The vascularization of the scaphoid is scarce and terminal. It mainly stems from branches of the radial artery in which 2 types of circulation can be distinguished: extraosseal and intraosseal circulation.1
The dorsal vessels originate from the radial artery or the dorsal intercarpal artery, entering the dorsal crest and supplying 70–80% of the intraosseal vascularization. The palmar vessels stem from the radial artery or the superficial palmar branch of the radial artery and, accessing through the scaphoid tuberosity, provide 20–30% of the remaining vascularization. Therefore, the vascularization of the proximal pole depends on the intraosseal flow, thus explaining the high frequency of pseudoarthrosis (or non-union) and avascular necrosis of the proximal pole in scaphoid fractures.2
Scaphoid fractures account for 60% of fractures in the carpus3 and evolve toward pseudoarthrosis in 8–10% of cases, even reaching 55% in the case of unstable fractures. They can appear in fractures in which a correct orthopedic treatment and follow-up have been applied, in untreated fractures and even be detected in radiographs obtained for a different reason.
The factors which determine the evolution toward scaphoid pseudoarthrosis are a lack of diagnosis, inadequate treatment, displacement of fracture fragments, ligament instability, presence of vascularization alterations and the complexity of the fracture.
The diagnosis of scaphoid pseudoarthrosis is based on the symptoms and imaging tests, such as radiographs, computed tomography (CT) and magnetic resonance imaging (MRI) scans.
The treatment of pseudoarthrosis has evolved from orthopedic treatment, which is currently not employed, to surgical treatment through different techniques, such as non-vascularized bone grafts (Matti-Russe,4 Fisk-Fernández5), vascularized bone grafts (pronator quadratus,6 first dorsal septal artery or the artery from the first or second dorsal intermetacarpal spaces7), arthroscopic treatment and even prosthetic scaphoid arthroplasties.8
Treatment must be applied early and adapted to the condition of the wrist in order to avoid sequelae. However, in spite of the various existing techniques, there is currently no golden standard to treat these lesions.
The aim of our study is to verify whether the morphology of the scaphoid is restored through the Fisk-Fernández technique, as well as to assess the clinical and radiographic results obtained in the treatment of scaphoid pseudoarthrosis through the aforementioned Fisk-Fernández technique.
Materials and methodsThis was a retrospective, protocolized, observational cohort study including all patients undergoing interventions for scaphoid pseudoarthrosis through the Fisk-Fernández technique at the Hand Surgery Unit of Valladolid University Hospital.
The inclusion and exclusion criteria were the following:
- 1.
Inclusion criteria:
- -
Patients with scaphoid pseudoarthrosis operated through the Fisk-Fernández technique.
- -
Patients who attended postoperative revisions prescribed by the Hand Surgery Unit.
- -
Minimum follow-up period of 6 months.
- -
- 2.
Exclusion criteria:
- -
Scaphoid pseudoarthrosis with absence of symptoms.
- -
Wrists presenting Scaphoid Non-union Advanced Collapse (SNAC) from grade II in which salvage surgery was indicated.
- -
Presence of avascular necrosis.
- -
The resulting sample included 43 patients intervened by the same surgeon during the period between June 1998 and April 2012. All patients were males, with a mean age of 31.28 years and a standard deviation of 12.57 years (range: 15–66 years) (Table 1).
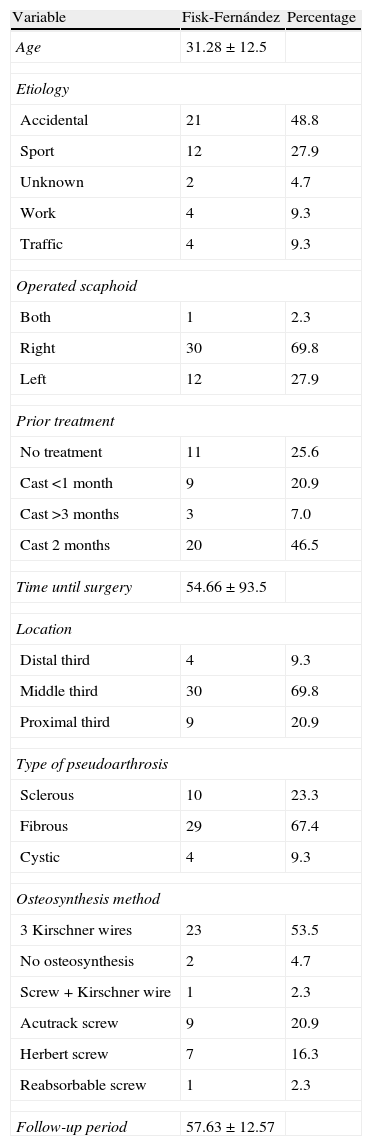
Fisk-Fernández. Variables studied.
| Variable | Fisk-Fernández | Percentage |
| Age | 31.28±12.5 | |
| Etiology | ||
| Accidental | 21 | 48.8 |
| Sport | 12 | 27.9 |
| Unknown | 2 | 4.7 |
| Work | 4 | 9.3 |
| Traffic | 4 | 9.3 |
| Operated scaphoid | ||
| Both | 1 | 2.3 |
| Right | 30 | 69.8 |
| Left | 12 | 27.9 |
| Prior treatment | ||
| No treatment | 11 | 25.6 |
| Cast <1 month | 9 | 20.9 |
| Cast >3 months | 3 | 7.0 |
| Cast 2 months | 20 | 46.5 |
| Time until surgery | 54.66±93.5 | |
| Location | ||
| Distal third | 4 | 9.3 |
| Middle third | 30 | 69.8 |
| Proximal third | 9 | 20.9 |
| Type of pseudoarthrosis | ||
| Sclerous | 10 | 23.3 |
| Fibrous | 29 | 67.4 |
| Cystic | 4 | 9.3 |
| Osteosynthesis method | ||
| 3 Kirschner wires | 23 | 53.5 |
| No osteosynthesis | 2 | 4.7 |
| Screw+Kirschner wire | 1 | 2.3 |
| Acutrack screw | 9 | 20.9 |
| Herbert screw | 7 | 16.3 |
| Reabsorbable screw | 1 | 2.3 |
| Follow-up period | 57.63±12.57 | |
The surgical technique employed was the Fisk-Fernández technique. The first step consisted in preoperative planning based on prior comparative radiographs of the contralateral hand which were used to determine the length and position of the scaphoid. Once the patient was placed on the operating table, the surgical fields were prepared for the obtention of a homolateral iliac crest graft, and the hand to be intervened was placed on a radiotransparent table with the arm in abduction. The Matti approach was employed to reach the focus of pseudoarthrosis and extract the fibrous tissue, performing curettage of the pseudoarthrosis margins with gauges and chisels until the healthy bone was reached, and leaving 2 concave surfaces on the edges of the pseudoarthrosis.
The following step was to create perforations in the remaining bone in order to verify its viability, noting the presence of bleeding points in the bone. After preparing the scaphoid, the cortico-cancellous graft was extracted from the iliac crest using an oscillating saw which afforded a better control of the direction of the cut than chisels.
The cancellous bone used to fill the concave areas in the edges of pseudoarthrosis was taken from the graft site using gauges. The role of this cancellous bone was to create an optimal space to receive the tricortical graft. This graft, formed by cortical bone-cancellous bone-cortical bone, was shaped to give it an adequate size and morphology to correct the scaphoid deformity created by the pseudoarthrosis. In 95% of cases, the graft was obtained from the homolateral iliac crest of the same patient, whilst in 1 case we used a graft from the distal radius and in 1 case from the distal radius associated to BMP.
Lastly, we established traction on the axis of the first finger in order to increase the space between both bone fragments and placed the cortico-cancellous graft shaped as a wedge with a palmar base, thus recovering the length of the scaphoid. Subsequently, we synthesized with Kirschner wires or screws (Acutrack, Herbert and reabsorbable) (Table 1) under scopy guidance. A minimum of 3 Kirschner wires were placed from the distal pole to the proximal, under scopy control and without surpassing the proximal joint cartilage, so that the iliac crest graft was fixed in different planes to prevent its rotation.
After ensuring through radiography that the placement of the graft and osteosynthesis material was correct, we closed the capsule and the radio-capitate ligament, closed the skin with reabsorbable suture and immobilized with plaster casts, 1 short palmar and 1 long dorsal, with the first finger in abduction.
The drainage was removed on the first postoperative day and patients were readmitted to the rehabilitation service after 3 weeks to start rehabilitation treatment including magnetotherapy.
Immobilization was maintained for a mean period of 9.5 weeks, (range: 8–12 weeks) after which the casts and Kirschner wires were removed in the clinic under local anesthesia, after verifying graft consolidation through radiographs.
Revisions were conducted on:
- ∘
The first day after the intervention.
- ∘
Third week.
- ∘
Second month (8–12 weeks), generally to remove the wires.
- ∘
Sixth month.
- ∘
Final revision: study protocol.
The protocol used studied the following parameters:
- -
Patient data: identification, medical history, affected hand, profession, mechanism of trauma, prior treatment, presence of associated lesions, time elapsed until surgery.
- -
Objective data: modified Green & O’Brien9 scale and measurement of intrascaphoid, radioulnar and scapholunate angles and height of the carpus in anteroposterior and lateral radiographs of the wrist, both preoperative and postoperative.
The Green & O’Brien scale assesses pain, functional state, range of movement and grip strength, assigning a value between 0 and 25 to each item and returning a poor value when the result is below 65 points, average between 65 and 79, good between 80 and 89 and excellent above 90 points.
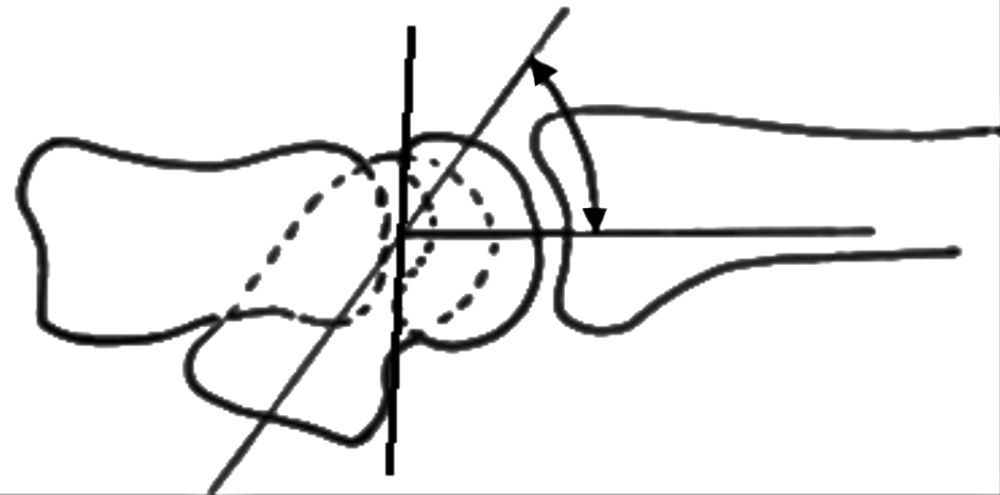
For the intrascaphoid angle in sagittal plane we used the measurement of the angle resulting from tracing a parallel line to the anterior cortical of the proximal scaphoid and another line running parallel to the posterior cortical of the distal scaphoid. The intrascaphoid angle in the frontal plane was measured between a line running parallel to the inferior cortical surface of the proximal pole and another running parallel to the cubital edge of the distal pole. For the radiolunate angle we used the measurement between the axis of the radius and a line running perpendicular to the tangent between the 2 poles of the semilunate, and for the scapholunate angle, that created between the axis of the semilunate and the axis of the scaphoid, taking into account that the distal pole thereof is used as reference in cases of pseudoarthrosis (Fig. 1).
Lastly, the height of the carpus was calculated using the Youm index,10 resulting from the coefficient of the carpal height between the lengths of the third metacarpal.
These measurements were carried out by the authors of the present article.
- -
Subjective data using the Scaphoid Score11 and DASH12 scales: the Scaphoid Score for self-assessment evaluates pain, function, mobility and overall satisfaction of the patient, returning a score between 0 and 11 points, which is considered poor below 5 points, average for 6 or 7 points, good for 8 or 9 points and excellent for 10 or 11 points.
The DASH questionnaire is used to assess the overall functional capacity of the upper limbs of patients in the study after the intervention. It scores 2 components: (a) a first mandatory component linked to symptoms, capacity or ability to carry out certain daily activities (30 sections with scores 1–5); and (b) a second optional component (4 sections with scores 1–5) regarding work-related tasks and hobbies. This score is transformed into a 0–100 scale, subtracting 1 from the average obtained and multiplying by 25. Patients are classified according to the greater disability, as the scores obtained become higher, considering variations as clinically relevant when they surpass 10 points.
The statistical analysis was carried out using the descriptive analysis of the clinical characteristics of each patient (age, gender, etc.) and the results of the objective and subjective assessment scales, comparing them with other series described in the literature.
In parallel, we carried out a comparative study of the preoperative and postoperative values of the angles and the height of the carpus, verifying the existence of statistically significant differences among them.
The quantitative variables of our study were presented through the mean, median and standard deviation, and the qualitative through the frequency distribution.
The comparison of quantitative values was carried out through the Student t test for related samples. This was done according to the analysis of measurements taken before and after surgery.
The data were analyzed using the statistical software package SPSS version 20.0 for Windows, and those values presenting a P<.05 were considered statistically significant.
ResultsIn total, 70% of the patients in the series presented pseudoarthrosis in the right scaphoid. The etiology of the lesion was accidental in 48% of cases, whilst 2 patients, (4.7%) did not recall the cause of pseudoarthrosis (Table 1).
The mean period until surgery was 54.66 months, with a standard deviation of 93.5 months.
The mean follow-up period was 57.63 months with a standard deviation of 12.57 months.
Out of the 43 lesions in the series, 40 became consolidated in a period between 16 and 24 weeks.
Pseudoarthrosis was located in the middle third of the scaphoid in 70% of the cases, in the proximal third in 21% and in the distal third in the remaining 9%. In total, 67% of the cases corresponded to fibrous pseudoarthrosis, a term employed by Eggli and Fernández13 to refer to cases in which, upon opening the focus of pseudoarthrosis, a soft tissue was observed and easily extracted.
A total of 50% of patients presented grade I radioscaphoid arthrosis, according to the classification by Knirk and Jupiter.14
We used Kirschner wires as an osteosynthesis system for surgery in 23 patients (53%), whilst in 17 patients (38%) we used screws (Table 1).
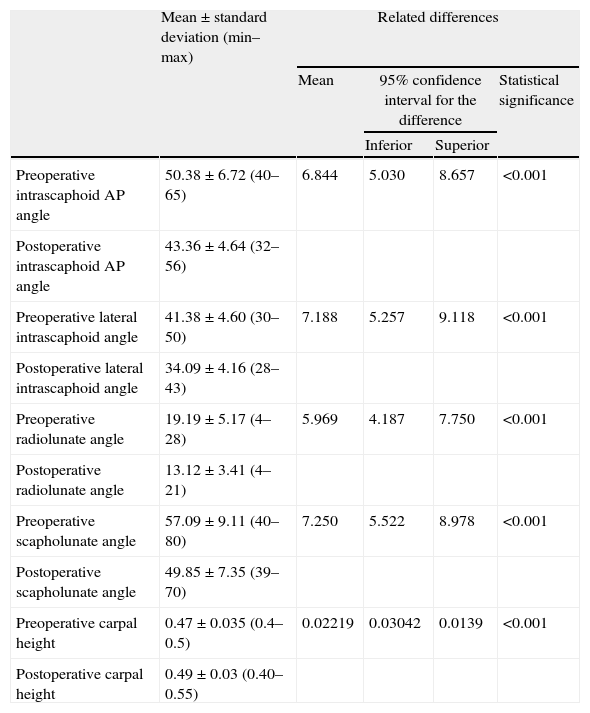
Table 2 shows the variation of the carpal angles between the preoperative and the postoperative states, so that the intrascaphoid angle in the anteroposterior plane went from a mean value of 50.38±6.72 (range: 40–65) to 43.36±4.64 (range: 32–56), the lateral intrascaphoid angle from 41.38±4.60 (range: 30–50) to 34.09±4.16 (range: 28–43), the radiolunate angle from 19.19±5.17 (range: 4–28) to 13.12±3.41 (range: 4–21) and the scapholunate angle from 57.09±9.11 (range: 40–80) to 49.85±7.35 (range: 39–70).
Variation of carpal angles.
| Mean±standard deviation (min–max) | Related differences | ||||
| Mean | 95% confidence interval for the difference | Statistical significance | |||
| Inferior | Superior | ||||
| Preoperative intrascaphoid AP angle | 50.38±6.72 (40–65) | 6.844 | 5.030 | 8.657 | <0.001 |
| Postoperative intrascaphoid AP angle | 43.36±4.64 (32–56) | ||||
| Preoperative lateral intrascaphoid angle | 41.38±4.60 (30–50) | 7.188 | 5.257 | 9.118 | <0.001 |
| Postoperative lateral intrascaphoid angle | 34.09±4.16 (28–43) | ||||
| Preoperative radiolunate angle | 19.19±5.17 (4–28) | 5.969 | 4.187 | 7.750 | <0.001 |
| Postoperative radiolunate angle | 13.12±3.41 (4–21) | ||||
| Preoperative scapholunate angle | 57.09±9.11 (40–80) | 7.250 | 5.522 | 8.978 | <0.001 |
| Postoperative scapholunate angle | 49.85±7.35 (39–70) | ||||
| Preoperative carpal height | 0.47±0.035 (0.4–0.5) | 0.02219 | 0.03042 | 0.0139 | <0.001 |
| Postoperative carpal height | 0.49±0.03 (0.40–0.55) | ||||
In turn, the carpal height increased from a preoperative value of 0.47mm±0.03 (range: 0.40–0.50mm) to a postoperative value of 0.49mm±0.03 (range: 0.40–0.55mm) (Table 2).
Among our patients, the Scaphoid Score presented a good or excellent result in 65% of the cases, and a mean value of 7.90±1.99 (range: 4–11) and mean DASH of 13.72±16.37 (range: 0–66.66).
The Mayo Clinic scale presented a good or excellent result in 58% of the patients, with a mean value of 76.27±15.08 (range: 35–100).
We registered 2 intraoperative complications: 1 breakage of the guide needle and 1 scaphoid burst fracture when introducing the screw; and 9 postoperative complications: 1 case of DSRC, 6 screw protrusions and the 3 lacks of consolidation mentioned previously.
DiscussionThe natural evolution of pseudoarthrosis is toward wrist SNAC.
The treatment of pseudoarthrosis to avoid this evolution has employed several different treatments, including conservative measures with immobilization techniques plus magnetotherapy, which are less effective than surgical treatment, so their use is currently obsolete.
The classical technique was that of Matti-Russe, which offered good long-term results, with up to 90% consolidation. However, it also resulted in 55% of consolidations in malposition.
Fisk15 postulated that the reduction of the deformity through the interposition of an anterior wedge graft would enable consolidation in the correct position, and subsequently, Fernández5 modified the technique through the interposition of a wedge-shaped iliac crest graft and the use of internal fixation, obtaining good results. Other authors have also employed this technique with varied results regarding consolidation. For example, Chen16 reported consolidation in 100% of cases, Daly17 in 95% and Finsen18 in 89% of the patients in his series, although many of these series correlated the results with the percentage of union, rather than alignment.
In our work, we observed consolidation in 93% of cases.
The graft fixation systems in the scaphoid have varied over the years. Thus, Fisk15 did not use any method of osteosynthesis if the graft was intrinsically stable. Several studies have used Kirschner wires for synthesis, including those by Chen,16 Takami,19 Stark,20 and Finsen,18 whilst many others have employed screws, such as those by Daly17 and Beris.21
Some of these works, such as those by Carter22 and Planchal,23 report a greater compression force of screws. However, after using both methods, we did not observe statistically significant differences between both osteosynthesis methods regarding consolidation, objective and subjective assessment and carpal angles.
Instead, we consider the use of wires more practical, since 3 wires in different axes traversing the graft from the proximal to the distal pole allow us to obtain good consolidation of the lesion with fewer complications. Instead, the use of screws resulted in 6 protrusions, which led to a removal thereof, as well as 1 breakage of the needle used to guide screw placement.
In our series, the objective assessment was carried out using the modified clinical scale by Green & O’Brien (Mayo Clinic), which observed that 52% of the patients presented a good or excellent result. Other authors also employed this scale to assess their results, including Inoue,24 who obtained an excellent result in 5 cases, good in another 5, average in 5 and poor in only 1 case, and Matsuki,25 who assessed his patients over a mean period of 26 months, obtaining a mean value of 91.4 points in the modified Mayo scale, with the result being excellent in 6 cases and good in 5 cases. In addition, Tsuyuguchi26 reported a mean wrist score of 81.2 points. These data mean that our results were similar to those described by other authors.
Regarding the subjective assessment, measured through the Scaphoid Score, we obtained good or excellent results in 65% of patients. This scale has also been employed by other authors to assess their series. Robbins11 analyzed 17 patients intervened for pseudoarthrosis and obtained an excellent result in 6 patients (35.29%), good in 5 (29.41%), average in 4 (23.52%) and poor in 2 (11.76%), whilst Steinmann27 treated 14 patients with vascularized graft and obtained excellent results in 2 of them (14.28%), good in 7 (50%), average in 4 (28.57%) and poor in 1 (7.14%).
The results of the DASH questionnaire in our series presented a mean value of 13.72±16.37 (range: 0–66.66) obtained in the final review. In his series, Schreuder28 obtained a mean result of 17, with a standard deviation of 18.4, whilst Finsen18 obtained a mean value of 2 (range: 0–33) in a revision, conducted after 10 years, of 39 cases of pseudoarthrosis synthesized with Kirschner wires.
Consolidation of pseudoarthrosis is an insufficient criterion to determine the success of treatment, since consolidation must be obtained whilst preserving the anatomy of the scaphoid in order to avoid sequelae derived from non-union.29
In our series, after surgery patients presented carpal angle values compatible with normality, except for 3 patients who did not achieve consolidation and required salvage surgery through the use of vascularized bone grafts, with a favorable subsequent evolution.
These results show a decrease in the value of the intrascaphoid, radiolunate and scapholunate angles between the preoperative and postoperative periods.
Moreover, carpal height experienced an increase of the postoperative mean compared to the preoperative, until an adequate height was obtained.
Other authors have also measured angles related to the scaphoid in their work. Matsuki25 did not find statistically significant differences between preoperative and postoperative radiographs, although he did achieve an improvement of the radiolunate angle and carpal height, but not of the scapholunate. Bertelli30 reported an improvement of the scapholunate and radiolunate angles and the carpal height following the surgical intervention.
Tsuyuguchi26 did obtain a statistically significant difference regarding the scapholunate and radiolunate angles, going from a preoperative radiolunate angle value of −5.5° to −0.1° in the postoperative period, as well as a change from 65 to 55° in the scapholunate angle, although he also reported a limitation of wrist function in those cases in which a correct alignment of the scapholunate angle could not be achieved. In his series, this author reported a slightly lower mean evolution period to that in our series, and also mentioned considerable variability in the measurement of the radiolunate angle, attaching greater importance to the scapholunate angle, whose data were similar to ours.
It is important to point out the technical complexity inherent to the measurement procedure of scaphoid angles, to which we must add the difficulty of obtaining reproducible measurements. One of the factors influencing this fact may be due to the occasional absence of pure lateral and anteroposterior radiographs in a strict sense.
There are different publications, like that by Larsen,31 explaining that the standard deviation in the interobserver variability lies between 2.60 and 18.15° whilst the intraobserver variation ranges between 1.89 and 4.66, so the recommendation is to measure the 3 angles to assess carpal alignment.
By measuring the radio-semilunar, radio-scaphoid and radio-capitate angles in 9 radiographs of wrists in flexion, extension and neutral inclination, García-Elias32 determined a mean overall error of 7.4° in the measurement of the angles carried out by 7 surgeons, 6 of which were hand specialists, thus giving an approximate idea of the difficulty of establishing this measurement.
The study had several limitations, including being a retrospective study. Another undisputable limitation is that all patients were intervened by the same surgeon.
The data were gathered from medical histories and personal interviews with patients, which could entail that part of the information was lost or even that patients did not accurately remember their condition or the trauma in cases where a long time had elapsed since the lesion or surgery until the interview. To this we must also add the fact that we have no preoperative data regarding the DASH, Scaphoid Score and Mayo Clinic scales.
Nevertheless, we conducted a personal interview with each patient, in which we objectively assessed the current clinical and radiographic condition, and during which the patients completed the subjective tests in person.
ConclusionThis study shows that treatment of carpal scaphoid pseudoarthrosis through palmar base wedge grafts enables correction of the angular deformity and achieves an anatomical consolidation in a high percentage of patients.
Level of evidenceLevel of evidence III.
Conflict of interestsThe authors have no conflict of interests to declare.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Please cite this article as: Hernández-Ramajo R, Martin-Ferrero MA, Simón-Pérez C, Muñoz-Moreno MF. Resultados del tratamiento quirúrgico de la seudoartrosis de escafoides carpiano con la técnica de Fisk-Fernández. Rev Esp Cir Ortop Traumatol. 2014;58:229–236.