We describe a case of a severely comminuted type IIIa open tibial fracture, with distal loss of bone stock (7cm), total involvement of the tibial joint surface, and severe instability of the fibular-talar joint.
The treatment performed consisted of thorough cleansing, placing a retrograde reamed calcaneal-talar-tibial nail with proximal and distal blockage, as well as a fibular-talar Kirschner nail. Primary closure of the skin was achieved.
After 3 weeks, an autologous iliac crest bone graft was performed to fill the bone defect, and the endomedullary nail, which had protruded distally was reimpacted and dynamized distally. The bone defect was eventually consolidated after 16 weeks.
Currently, the patient can walk without pain the tibial-astragal arthrodesis is consolidated.
Se describe un caso de fractura abierta de tibia grado iiia con gran conminución y pérdida distal de stock óseo (7cm) con total afectación de la superficie articular tibial y gran inestabilidad de la articulación peroneo-astragalina.
El tratamiento realizado consintió en practicar una exhaustiva limpieza, colocándose un enclavado fresado retrógrado calcáneo-astrágalo-tibial con bloqueos proximales y distales, además de una aguja de Kirschner peroneo-astragalina. Se consiguió el cierre primario de la piel.
A las 3 semanas se procedió al aporte de injerto óseo autólogo de cresta ilíaca rellenando el defecto óseo, a la reimpactación del clavo endomedular que estaba protuido distalmente y a la dinamización distal. Se consiguió la consolidación del defecto óseo en 16 semanas.
Actualmente, el paciente deambula sin dolor con la artrodesis tibio-astragalina consolidada.
Retrograde implantation of intramedullary nails in the femur and humerus is a common clinical technique.1–8 Retrograde nailing of the tibia has been described in experimental models by Hofmann et al.,9 in cases of tibiotalar arthrodesis among rheumatic and neuropathic patients,9–11 in posttraumatic sequelae in the ankle and in rescue arthroplasties. It has also been recently described as an option for the acute treatment of ankle fractures in delicate patients with significant osteoporosis.12 In cases describing treatment of neuropathic patients with ankle fractures, retrograde nailing was performed 3 weeks after the lesion.13 We could not find any cases in the literature of retrograde nailing in distal tibial fractures among young patients treated at the time of the trauma.
We present a case of grade IIIa tibial open fracture with large distal bone loss that significantly compromised the functionality of the ankle joint, also presenting joint instability with fibular-talar dislocation. This case was treated by retrograde intramedullary nailing of the tibia, with a contribution of posterior autologous bone, achieving consolidation of the fracture and ankle arthrodesis within 16 weeks.
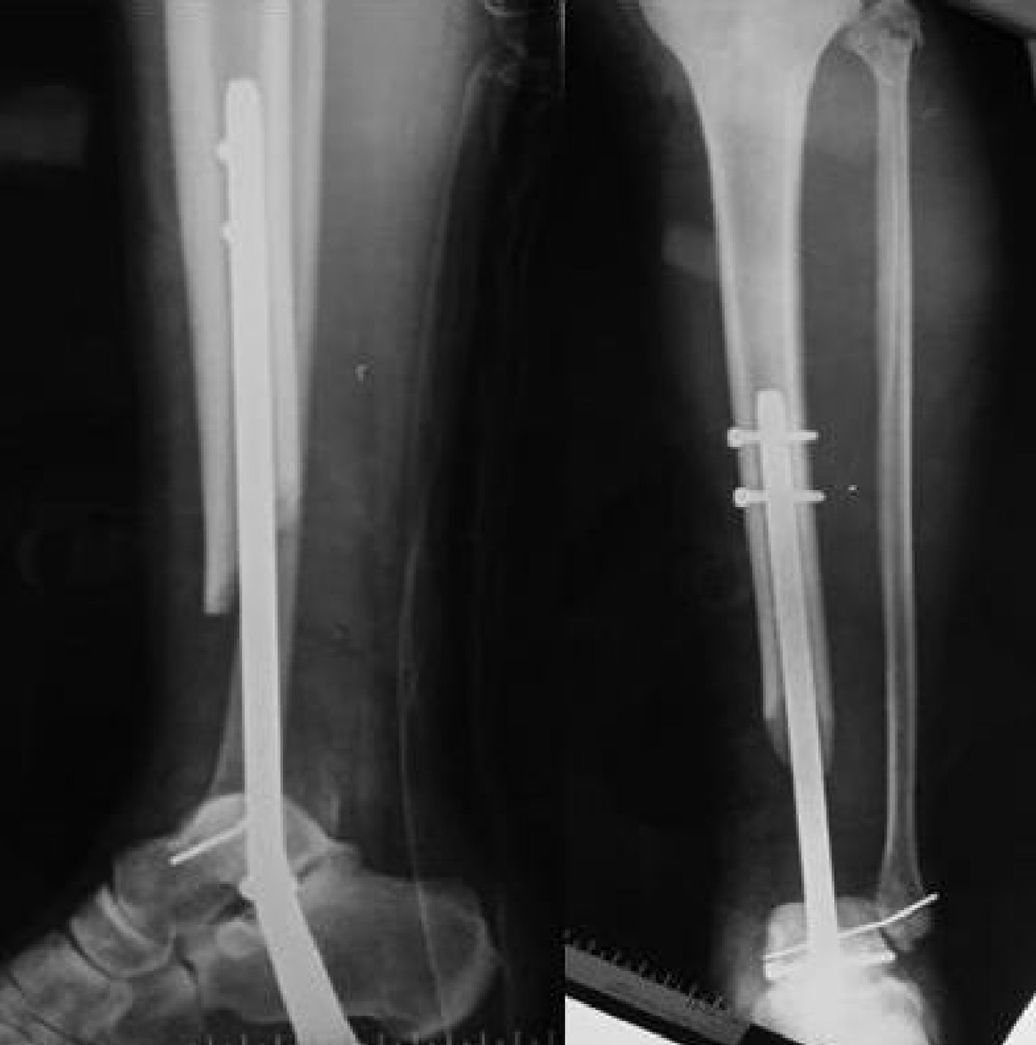
Case reportPatientWe present the case of a 23-year-old patient who was admitted after an aircraft accident (ultralight aircraft) with a diagnosis of grade IIIa open fracture of the distal third of the left tibia with loss of bone substance and fibular-talar dislocation (Fig. 1) and L3–L4 burst fracture.
Method and resultThe patient was treated at the Emergency Service thorough exhaustive cleaning and prophylactic antibiotic (amoxicillin–clavulanate 2g/8h/5 days) and anti-tetanus treatment. We proceeded to stabilize the tibial fracture by intramedullary retrograde reamed nailing of the calcaneus-talus-tibia (Synthes, Solothurn, Switzerland) with distal and proximal locking, and completing the procedure with fixation using a fibular-talar Kirschner wire (Fig. 2). Primary skin closure was achieved. We also performed L2–L5 lumbar arthrodesis (or fusion).
The patient had a good postoperative evolution and did not present any septic signs.
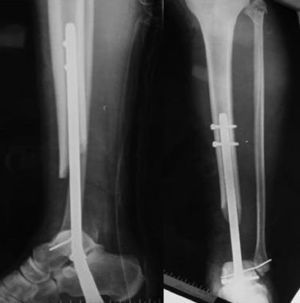
At 3 weeks we carried out a graft of autologous iliac crest bone to fill the bone defect. We also reimpacted the intramedullary nail, which protruded slightly in a distal direction and performed distal dynamization. Consolidation of the bone defect was achieved at 16 weeks.
After 3 years of follow-up, the patient was able to walk without pain, with a consolidated tibiotalar arthrodesis and with an arthrodesis of the subtalar joint caused by the nailing (Fig. 3).
DiscussionFractures of the distal end of the tibia often occur as a result of high energy trauma with great comminution and severe tissue damage. In such lesions, surgical treatment with internal fixation has shown a high rate of infection and pseudoarthrosis.14
In our case there was a considerable loss of bone substance at the distal end of the tibia, as well as great instability of the rest of the fibular-talar joint, which prevented the function of the ankle joint. We considered a system that would provide sufficient stability of the focus and facilitated the final arthrodesis of the joint as a stabilizing treatment for the lesion.
We did not consider external fixation because distal fixation of the talus and/or calcaneus did not guarantee the stability of the focus due to the considerable instability of the fibular-talar joint and it would not represent a definitive treatment. In addition, although this represents an alternative treatment, external fixation also presents a high rate of infection at the level of the pins, deep infections and septic arthritis.15 In the long term, external fixation also presents a high rate of pseudoarthrosis.16
Tibial-talar-calcaneous fusion is a widespread procedure for the treatment of rheumatoid and posttraumatic arthritis, avascular necrosis of the talus, Charcot neuropathy and other deformities secondary to neuromuscular diseases. It has also been used as a rescue therapy in ankle arthroplasty failures. Intramedullary tibial-talar-calcaneous fixation can be achieved by antegrade and retrograde nailing of the tibia. The rate of pseudoarthrosis of the arthrodesis using retrograde intramedullary nailing has been reported at between 5% and 15%.17 The disadvantage of this treatment in open fractures is the risk of infection and the need for a subtalar fusion.
Retrograde intramedullary nailing is used as a routine technique in femoral and humeral fractures.1,2,4–7,11,12 Its use has been described to achieve tibiotalar fusion in rheumatic and neuropathic patients.10,13,17 Its use in acute distal tibial fractures in young patients has not been described, probably due to iatrogenic involvement of the tibiotalar and subtalar joints, with the method of choice to treat this type of fracture being osteosynthesis, external fixation or a combination of both techniques. The use of intramedullary nailing has recently been described as an option for the acute treatment of ankle fractures in elderly patients suffering significant osteoporosis.12
In some cases, primary arthrodesis has been described as a good method for the treatment of non-reconstructable fractures of the tibial pilon with metaphyseal defects. In these cases, the arthrodesis was performed at 20 weeks of the lesion,18 using fusion plates requiring good soft tissue coverage, which could have been compromised at the time of the lesion. Furthermore, fusion with plates provides limited results in cases with severe bone defects where compression of the focus is not possible. On the other hand, the use of intramedullary nails provides axial and rotational stability, in addition to a stable fixation.4
A successful arthrodesis is linked to the stability of the fixation.19 In cases with metaphyseal bone loss in which compression by osteosynthesis cannot be performed, the use of plates and screws for arthrodesis is limited. On the other hand, synthesis or fixation by intramedullary nailing provides both axial and rotational stability.20
Although retrograde nailing affects the subtalar joint iatrogenically, it has been reported that the long-term evolution of an isolated tibiotalar arthrodesis also significantly affects the subtalar joint.21 In this case the effect of nailing also produces a subtalar arthrodesis which, although limiting hindfoot mobility, allows patients to walk without pain.
Based on the outcome of the present case, we consider that, in tibial pilon fractures with severe joint involvement in which the function of the ankle is hardly feasible, intramedullary nailing with retrograde entry reaming can be a technique to consider.
Level of evidenceLevel of evidence V.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that this work does not reflect any patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Please cite this article as: Valls-Mellado M, Martí-Garín D, Fillat-Gomà F, Marcano-Fernández FA, González-Vargas JA. Enclavado retrógrado en fractura tibial. Rev Esp Cir Ortop Traumatol. 2014;58:196–199.