The aim of this study was to investigate the clinical results and radiographic findings after superior capsular reconstruction (SCR) of postero-superior symptomatic irreparable rotator cuff tears (PSIRCT) using a new SCR technique using autologous hamstring graft.
Material and methodsFrom 2014 to 2016, 8 shoulders of 8 patients (mean age 59.6 years) with PSIRCT underwent SCR using autologous hamstring graft.
Physical examination, X-ray and MRI were performed before the surgery and 12 months after it. A descriptive analysis was performed of the variables, and the non-parametric test of signs comparing the measurements taken before the operation and 12 months after it.
ResultsWe found an improvement in the Constant test from 49 before the SCR to 77.25 one year after the operation. The mean active flexion significantly increased from 99.3° to 142.5°. The mean preoperative AH distance increased from 5.25 (range from 3 to 7) before surgery to 8.18 (range from 6 to 10.5) after the SCR. There were no tears of the graft during follow-up.
ConclusionSCR with a hamstring graft improves the function of the shoulder in PSIRCT, and is an alternative technique for treating these injuries without closing the door to other types of surgery.
El objetivo de este estudio es investigar los resultados clínicos y los hallazgos radiográficos tras la reconstrucción de la cápsula superior (RCS) en las roturas irreparables posterosuperiores sintomáticas (RIPS) del manguito de los rotadores mediante una nueva técnica de RCS utilizando injerto autógeno de isquiotibiales.
Material y métodosDesde 2014 hasta 2016, 8 hombros en 8 pacientes (edad media de 59,6 años) con RIPS fueron tratados con la RCS utilizando injerto autógeno de isquiotibiales. El examen físico, Rx y RM fueron realizados antes de la cirugía y a los 12 meses. Se ha realizado un análisis descriptivo de las variables y se ha utilizado test no paramétrico de los signos para comparar las medidas tomadas antes de la cirugía y a los 12 meses.
ResultadosEncontramos una mejoría en el test de Costant: de 49 antes de ser intervenido a 77,25 al año de la RCS. La media de flexión activa aumentó de forma significativa de 99,3° a 142,5°. La distancia media HA preoperatoria aumentó de 5,25mm (rango de 3 a 7mm) antes de la cirugía a 8,18mm (rango de 6 a 10,5) tras la RCS. No hubo roturas del injerto durante el seguimiento.
ConclusiónLa RCS con injerto de isquiotibiales mejora la función del hombro en las RIPS. Es una técnica alternativa al tratamiento de dichas lesiones sin cerrar las puertas a otras cirugías.
Treating patients with irreparable rotator cuff tear remains a challenge for orthopaedic surgeons. Several surgical treatments have been used, such as: debridement with or without biceps tenotomy,1–4 partial repair,5–10 tendon transfer,11,12 interposition grafting13–15 or reverse prosthesis.16 However, the results of these techniques are not optimal for treating young patients.
There is now a new option, originally developed by Dr. Mihata,17 who demonstrated the importance of the superior capsule of the shoulder as a stabilising structure, so that in the event of a postero-superior irreparable symptomatic tear (PSIRCT) the capsule at least, should be reconstructed in an attempt to restore the shoulder's normal fulcrum, and thus enable shoulder stability and function. In the original description, superior capsule reconstruction (SCR) was performed with fascia lata. There is no information on this reconstruction using an autologous graft other than fascia lata.
The aim of this study was to research the clinical results and radiographic findings after SCR for PSIRCT using a new SCR technique using autologous hamstring graft.
Our hypothesis was that SCR using the hamstring could increase the acromiohumeral (AH) distance and improve the functional results of PSIRCT.
Materials and methodsA clinical, prospective study, on a pilot sample of 8 patients to evaluate the clinical results and radiographic findings of an SCR using autologous hamstring graft.
The subjects included in the study were patients on the waiting list from our hospital's clinics, who were admitted between 2015 and 2016 with a PSIRCT, and who met the following inclusion criteria: complete irreparable tear of the supraspinatus or infraspinatus; conservative treatment failure; no or minimal joint degeneration; aged between 40 and 65 years at the time of first consultation, and having given their written consent for intervention.
A tendon was considered irreparable when it could not be repaired to its original footprint at the major tuberosity and, although the final decision was intraoperative, we were guided by various signs of irreparability such as: upper migration of the humerus with an AH distance of less than 7mm, Patte stage 3 tendon retraction, Goutallier grade 3 and 4 fatty infiltration, and Thomazeau's stage 3 muscle atrophy.
The exclusion criteria were: joint degeneration (Hamada18 stages 3, 4 or 5), severe upper migration of the humeral head that did not descend with arm traction, deltoid deficiency, irreparable injury to the subscapularis or shoulder rigidity.
The patients were assessed by the same surgeon in the clinic, with a standard history and physical examination that included the Constant and SST test, before the operation, and at 12 months following it. Forward flexion was measured at the patient's side, with the axis of the goniometer arm over the arm axis, and the other goniometer arm following the trunk axis, supported on the ribcage. We measured external rotation in front of the patient asking them to perform active and non-painful external rotation manoeuvres; we measured internal rotation from behind the patient, and asked them to perform active, non-painful internal rotation manoeuvres; we observed the point that they could reach with the tip of the thumb. We assessed strength with a dynamometer: the patient's spine supported by the back of a chair, they lifted their arm on the plane of the scapula, with their hand in pronation and palm facing towards the floor. Tying the strap to the proximal hook of the dynamometer supported by the wrist, we pulled the distal hook downwards exerting constant force, and the cursor showed us on the scale the kg that the patient managed to bear. We took 3 measurements, and took the maximum score achieved as the benchmark.
An imaging study was performed using plain X-rays in 2 views (true AP and Y). Glenohumeral degeneration was also measured by the Hamada scale, and AH distance by the method described by Ellman.19 MR images were taken on the coronal, sagittal and axial planes, enabling us to assess the type of tear, its size, its retraction and the quality of the tendons affected, and to gain an idea of its repair capacity. We assessed fatty degeneration using Goutallier's system.20 The plain X-rays and MRI were undertaken preoperatively, and at one year's follow-up.
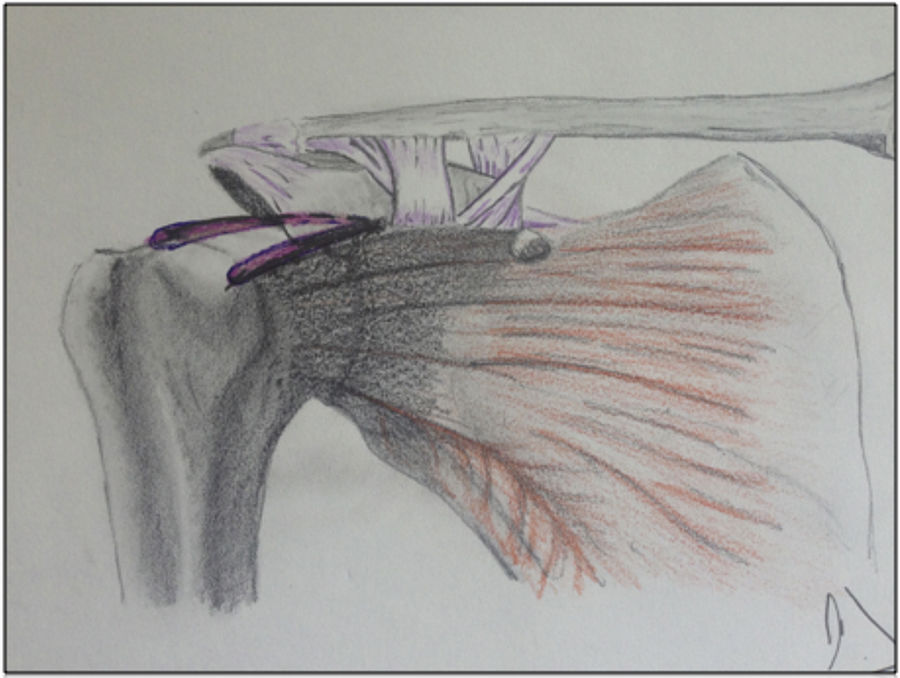
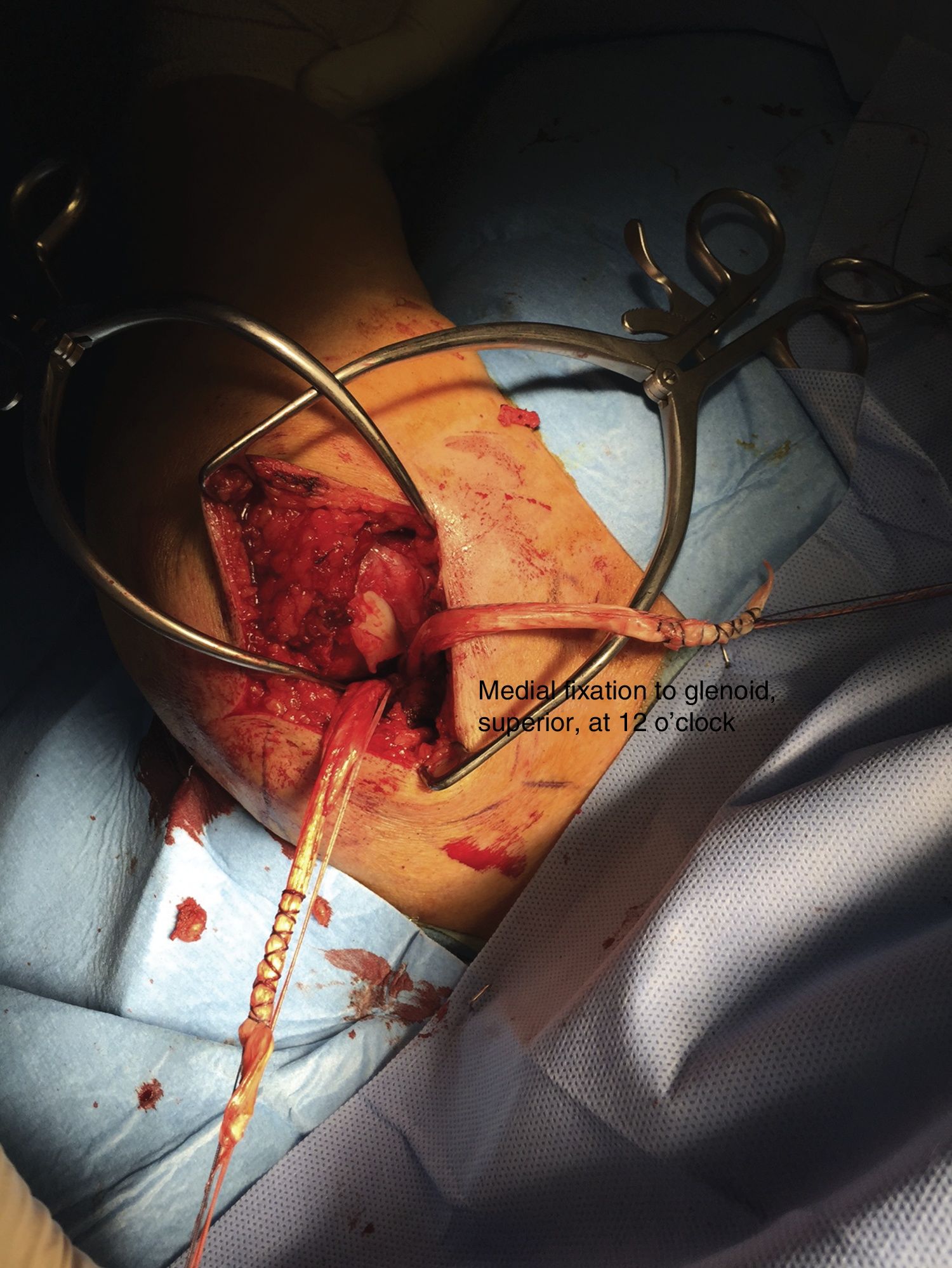
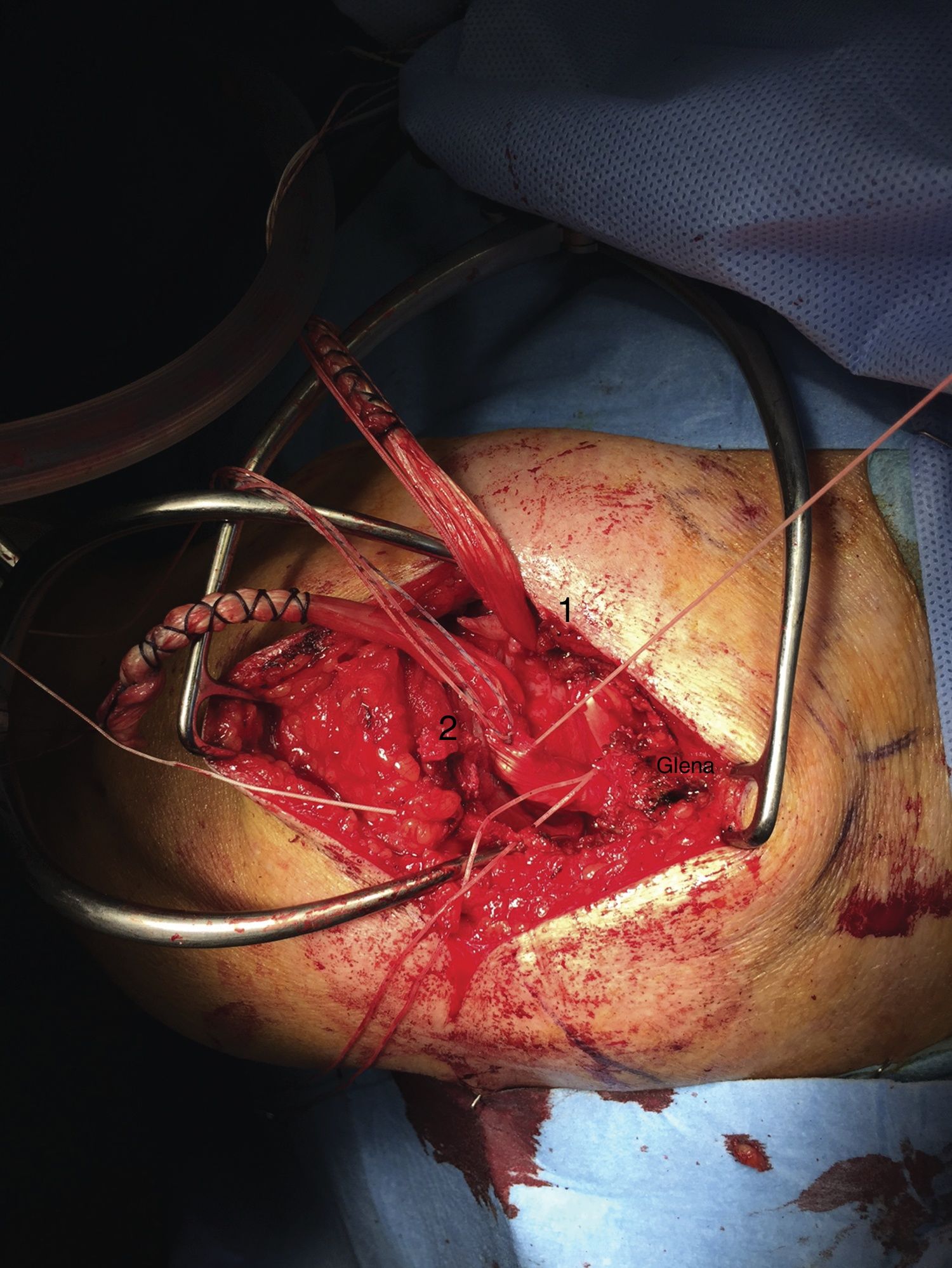
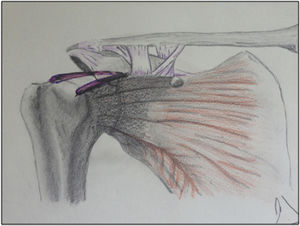
All the interventions were performed under general anaesthesia, with the patient in the deckchair position, and by the same surgeon. After the superior approach, the irreparability was assessed of the tendon tear and of the tendons involved. Only one patient underwent subacromial decompression due to a type 3 acromion. Once the injury had been assessed, the SCR was performed with a hamstring allograft. After gentle debridement of the upper area of the glenoid and the footprint of the greater tuberosity, medial fixation was obtained to the glenoid bone in its upper area, at 12 o’clock, from the central area of the graft (with metallic screw 5 with 4 strands). Lateral fixation was also obtained (with the same type of screw as in the glenoid cavity) of the 2 ends of the graft in the humeral head at two points: one antero-superior, next to the entry area of the bicipital groove and to the area of the interval and subscapularis; and a second fixed behind, in the postero-superior area near the infraspinatus, which was also sutured to the plasty (Figs. 1–3). The lateral fixation was performed under tension and in an arm position at about 30° abduction, neutral rotation, and 20–30° flexion.
All the subjects followed the same protocolised rehabilitation regimen, using a sling for 2 weeks, starting passive exercises at 2 weeks, active exercises at 6–8 weeks, and strengthening exercises for the cuff and scapula stabilisers from 10 to 12 weeks.
A descriptive analysis of the variables was performed, and the non-parametric sign test was used, comparing the measurements taken before the operation, and at 12 months after it.
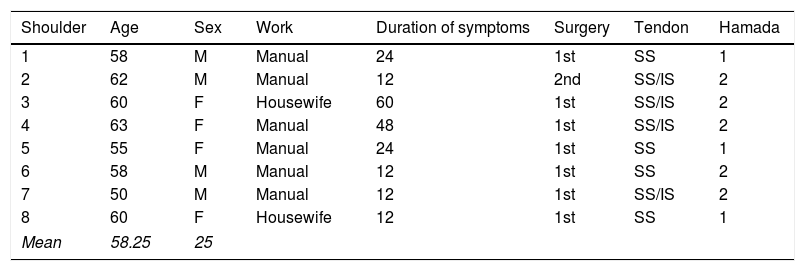
ResultsFour males and four females were operated, with a mean age of 59.66 years (range from 55 to 63 years) at the time of the surgery. The mean duration of symptoms (pain and functional) before the operation was 25.3 months (from 12 to 60 months). The stage of arthrosis prior to surgery was classified using the Hamad system21: we found 3 shoulders in stage 1, and 5 in stage 2 (Table 1).
Summary of the patients.
| Shoulder | Age | Sex | Work | Duration of symptoms | Surgery | Tendon | Hamada |
|---|---|---|---|---|---|---|---|
| 1 | 58 | M | Manual | 24 | 1st | SS | 1 |
| 2 | 62 | M | Manual | 12 | 2nd | SS/IS | 2 |
| 3 | 60 | F | Housewife | 60 | 1st | SS/IS | 2 |
| 4 | 63 | F | Manual | 48 | 1st | SS/IS | 2 |
| 5 | 55 | F | Manual | 24 | 1st | SS | 1 |
| 6 | 58 | M | Manual | 12 | 1st | SS | 2 |
| 7 | 50 | M | Manual | 12 | 1st | SS/IS | 2 |
| 8 | 60 | F | Housewife | 12 | 1st | SS | 1 |
| Mean | 58.25 | 25 | |||||
The non-parametric signs test was used, with statistically significant differences in the Constant test (p<.01). We observed an improvement from 49 before the SCR to 77.25 one year after it.
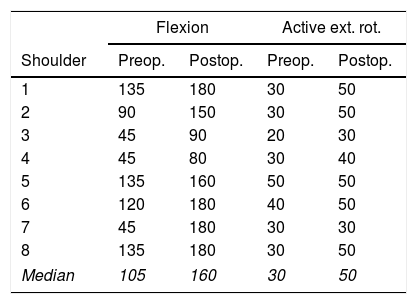
The range of active motion significantly improved after the SCR until the end of follow-up (12 months). Mean active flexion increased from 99.3° preoperatively to 142.5° (p<.01); mean external rotation increased from 32.5° to 43.7° (p<.01) (Table 2, Fig. 4).
There were no surgical, intraoperative or postoperative complications in the year of follow-up.
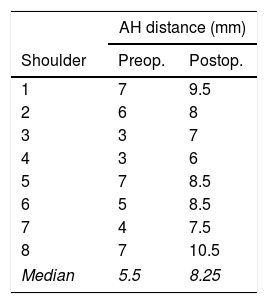
The mean preoperative AH distance was 5.25mm (range from 3 to 7mm), in 5 shoulders it was less than 7mm. After the SCR, the mean AH distance increased significantly to 8.18 (range from 6 to 10.5) (Table 3).
No tears were observed on MRI during follow-up of the implanted hamstring plasty.
DiscussionThe results in this paper show a functional improvement in patients with irreparable rotator cuff tear. In those who underwent a SCR with autologous hamstring graft, we observed, at one year's follow-up, an increased AH distance, and improved active flexion.
Patients with PSIRCT have a defect of the superior joint capsule. SCR for PSIRCT restores superior glenohumeral stability and improves shoulder function.22,23
Because most rotator cuff tears are reparable, the treatment of patients with PSIRCT remains a challenge for orthopaedic surgeons. The available treatments include traditional patch grafts using different materials inserted in the injured tendon, but they have shown a high re-tear rate24-26 without significantly altering the AH distance.
Audenaert et al.27 published that the AH distance was not significantly modified after conventional patch grafts placed medially to the tendon, and laterally to the greater tuberosity for massive rotator cuff tears.
Clitherow et al.28 described an autologous hamstring graft reconstruction to augment retracted rotator cuff tendons, attempting to restore the length of the musculotendinous unit, but without performing an SCR.
Despite the interest in this technique, current knowledge on SCR is based essentially on biomechanical studies29-31: there are few clinical studies on SCR for irreparable rotator cuff tears. In addition to Mihata's classical clinical study with autogenous fascia, with 24 shoulders in 23 patients, we only found one multicentre study with dermal allograft by Denard.32 We saw clear differences between both studies: there was a low rate of graft healing with the dermal allograft (45%), and they found no increase in AH distance one year afterwards, which is different to Mihata's results with autogenous fascia lata. However, 100% of the patients with a healthy graft had successful results, which makes us believe that it is important to prevent the graft tearing after an SCR, and that we must define the type of graft to be used to achieve this outcome.
Our data indicate that SCR, using the described hamstring graft technique, results in an increased mean AH distance of 5.25–8.18mm. This is in line with the data published by Mihata21 where the SCR, using fascia lata graft, obtained an increased mean AH distance of .46–8.7mm (significant increase of 4.1±1.7mm after SCR). We, like this author, had no tears of the graft we used.
The functional results of PSIRCT repair with fatty degeneration of the infraspinatus have been traditionally disappointing. Our results with SCR using hamstring allograft, like those of Mihata, provided improvement, despite fatty infiltration of the infraspinatus.
These data confirm the stabilising role of the superior shoulder capsule, so the rotator cuff is neither the only nor the main stabiliser of the shoulder. It undertakes dynamic action, reinforces stabilisation of the capsule, and restores the strength of the shoulder. This fact explains how when faced with an PSIRCT we can, at least, reconstruct the capsule restoring the normal fulcrum of the shoulder, and thus enable it to become stable and functioning.
This study's limitations are the small number of patients, the lack of a control group, and the short follow-up time. The statistically significant differences, despite the small sample size, are because the effect size (pre- and postoperative difference) is very large.
We believe that it is important to show the preliminary results of this new technique given the current interest and debate surrounding it, and because there are so few published clinical studies. We are aware that there are important aspects that we do not know, such as the most appropriate graft, the indications or the time it might last, and that we must approach all new techniques with due care.
ConclusionsSCR with hamstring allograft improves the function of the shoulder in PSIRCT: it is an alternative treatment technique for these injuries without closing the door to other surgery.
Level of evidenceLevel of evidence iii.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Rosales-Varo AP, Zafra M, García-Espona MA, Flores-Ruiz MA, Roda O. Reconstrucción de la cápsula superior en las roturas irreparables del manguito mediante injerto autógeno de isquiotibiales. Rev Esp Cir Ortop Traumatol. 2019;63:1–6.