To describe the results of tibiotalocalcaneal arthrodesis (TTC) using a humeral locking plate.
Methods and materialsA retrospective, observational study was conducted between January 2007 and December 2013 in the Hospital Militar Central de Bogotá. The study included patients with symptomatic osteoarthritis diagnosed clinically and radiologically, and who underwent TTC arthrodesis using a humeral locking plate with a minimum follow up of 6 months.
ResultsThe total number patients was 35, of whom 7 (20%) were women and 28 (80%) men, with a mean age 36.3 years (19.77). Aetiology: 74% with post-traumatic arthritis, most of them secondary to gunshot wounds and fragmentation weapons, and neuropathic in 20%. An autogenous graft was used in 13 cases, and 14 cases using both, with a mean consolidation time of 4.37 months. Complications include, delayed union in 3 cases, and surgical site infection in 4. The postoperative functionality (AOFAS) mean was 66.7/100 points, with a score of 2.35 on a visual analogue pain scale.
ConclusionTTC arthrodesis using a humeral locking plate is a suitable option for fixing this type of arthrodesis, with a low rate of complications, and postoperative results that revealed satisfactory improvement in pain and consolidation.
Describir los resultados obtenidos en la artrodesis tibiotalocalcánea (TTC) con placa humeral bloqueada.
Métodos y materialesEstudio descriptivo observacional, retrospectivo tipo serie de casos, entre enero de 2007 y diciembre de 2013 en el Hospital Militar Central de Bogotá. Se incluyó a pacientes con artrosis TTC sintomática diagnosticada tanto clínica como radiológicamente tratados mediante artrodesis TTC con placa humeral bloqueada con seguimiento mínimo de 6 meses.
ResultadosUn total de 35 pacientes: 7 (20%) mujeres y 28 (80%) hombres. Edad promedio 36,3 años (19,77). Etiología: 74% con artrosis de origen postraumático, en la mayoría de los casos, secundaria a heridas por arma de fragmentación y heridas por proyectil de arma de fuego; neuropáticas 20%. El injerto utilizado fue autógeno en 13 casos y combinado en 14 casos, con un tiempo de fusión promedio de 4,37 meses. Respecto a complicaciones, se presentó retraso en la consolidación en 3 casos e infección del sitio operatorio en 4. La puntuación postoperatoria promedio en la escala AOFAS fue: 66,7/100 puntos con un puntaje en la Escala Visual Análoga del dolor de 2,35.
ConclusiónLa artrodesis TTC con placa humeral bloqueada es una adecuada opción para la fijación de este tipo de artrodesis con una baja tasa de complicaciones y con resultados postoperatorios satisfactorios en cuanto a mejoría de dolor y consolidación.
Patients with complaints that involve the foot as well as the ankle may have significant pain, deformity and functional limitation. Many conditions can cause degeneration in the ankle and subtalus joint. Arthrodesis is indicated in many complaints, chiefly rheumatoid arthritis, degenerative arthrosis, injury or infection.
Other less common indications are avascular necrosis of the talus, neuroarthropathy, osteochondral lesions of the ankle and subtalus which are not treatable in other ways, and rescue surgery such as the total arthroplasty of failed ankles.1,2
In our fourth level hospital, the most common complaint is injuries caused by fragmentation weapons (antipersonnel mines) which compromise the lower limbs. They make it necessary for the reconstructive surgery team to innovate or use osteosynthesis products supplied by commercial companies for other purposes (such as humeral osteosynthesis) to resolve complex fractures in other joints.
The standard orthopaedic treatment of ankle and subtalus joint degeneration when conservative management has failed is tibiotalocalcaneal (TTC) arthrodesis. One of the first descriptions of this technique was given by Lexter in 1908.3–6 He had used this procedure in the ankle and subtalus joints with boiled bones from corpses.
Several materials may be used for TTC arthrodesis: current implants include screws,7,8 plates,9,10 intramedular nails11–13 and external fixation.9,14
There is little information in the literature about the use of locked plates in vivo for TTC arthrodesis.
Nevertheless, within the most representative studies of this technique at an international level, the one by Ahmad et al.15 stands out. In this he found that the use of a locked plate in this technique increased the stability of the construct with consolidation in up to 94% of cases.
In this work we report the clinical and functional results of patients treated using TTC arthrodesis with fixation by a humeral locking plate.
Materials and methodsA descriptive observational and retrospective study of a series of cases from January 2007 to December 2013 in the Hospital Militar Central, Bogotá. This is a fourth level hospital.
This study includes all of the patients diagnosed with symptomatic arthrosis of the tibiotalar and subtalar joints that did not improve with medical management, and who also presented risk factors for pseudoarthrosis or poor consolidation, such as obesity, poor bone quality or deformities, among others. They were treated using TTC arthrodesis, with a locking humeral plate and a transfibular approach. Patients with TTC arthrosis were included after clinical or X-ray diagnosis, with functional evaluation prior to surgery using the American Orthopaedics Foot and Ankle Society (AOFAS) scale, and with a follow-up of at least 6 months.
Data were collected in a predesigned base for subsequent analysis using the SPSS 21 statistical analysis programme.
The exclusion criteria ruled out those patients with large scars or lesions on the side of the ankle, or ones which required Plastic Surgery for treatment, without excluding lesions on the soft medial or anterior parts of the ankle.
This study was approved by the Independent Ethics Committee of the Hospital Militar Central.
Surgical techniquePreoperatorative evaluation:
It is important to evaluate bone quality before the procedure, as if there is significant deformity the other limb must be compared as a template to estimate the position of the arthrodesis. In addition to X-rays, computerised tomography is recommended to evaluate failed joints and bone defects, particularly when the integrity of the tibia metaphysis is in question.
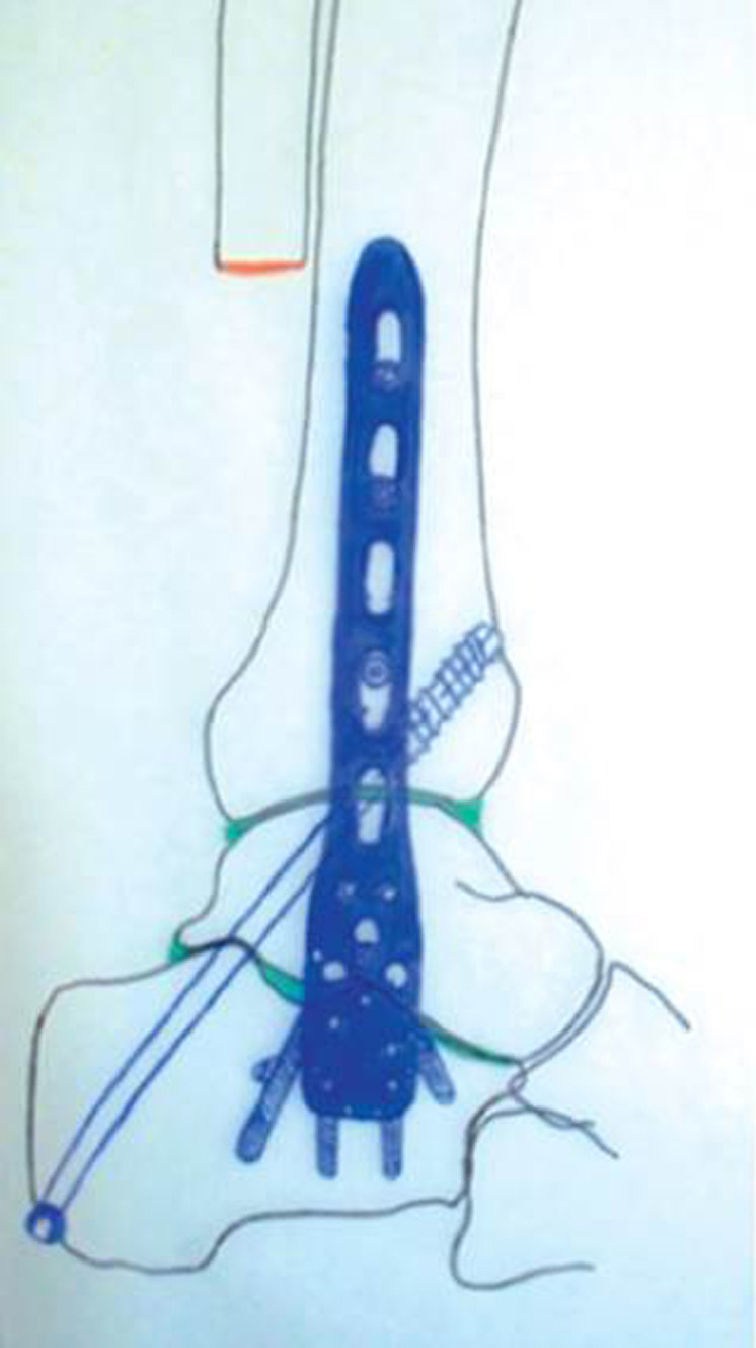
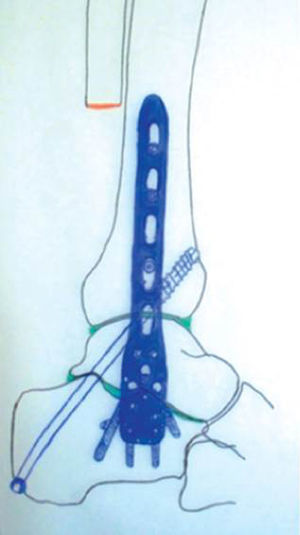
It is very important to take implant adaptation into account, as it was designed for another purpose. Preoperational planning takes place (Fig. 1).
The surgical technique described below is the one used by the authors and is analysed in this study:
- 1.
The patient is positioned supine with a support under the ipsilateral hip and internal rotation of the ankle to facilitate exposure of the fibula.
- 2.
A standard transfibular longitudinal incision is made of 8–12cm, after which the distal fibula is resected to expose the tibiotalar and subtalar joint, dissecting the distal portion of the calf nerve (Fig. 2). The incision is extended to the base of the fourth metatarsus, making it possible to raise the digitorum brevis extensor muscle to suitably expose the subtalar joint.
- 3.
The remaining cartilage in the arthritic joint and subchondrial bone tissue is removed until the bleeding bone is visible.
- 4.
Cuts in the bone are made and the soft tissues are freed to correct any deformity in the previous alignment of the limb.
- 5.
After preparing the joint surfaces bone grafts must be put into place by filling or covering highly fragmented bone defects. In some cases structural grafts must be put into place to prevent the limb from shortening (obtained from previously partially dried fibula and the bone bank) (Fig. 3).
- 6.
A grooved 7.3mm screw with a partial thread is placed posterior-inferior to anterior-superior through the calcaneus to the astragalus and distal tibia, compressing the ankle joint as well as the subtalar joint. This screw is placed perpendicular to the locked plate, with the screw in the sagital plane and the plate in the coronal plane, to increase the rotational stability of the fixation.
- 7.
The proximal part of the locked humeral plate is fixed to the calcaneus and astragalus by locked screws in multiple planes of fixation (putting them into position inversely). The distal part of the plate is fixed to the distal tibia by a combination of cortical and locked screws. In the majority of cases fixing is achieved in the calcaneus using 4 locked screws, with 2–3 in the talus and 4 bicortical screws in the distal tibia (Fig. 4).
Immediately after the operation patients are fitted with a short immobiliser of the posterior calf and foot splint type until the bone callus is seen in the X-rays.
In all cases this immobilisation time lasts from 6 to 12 weeks after surgery, especially in patients who are overweight or have severe osteopenia; and most especially those with Charcot's arthropathy are immobilised during 10–12 weeks after the procedure.
Once X-rays show consolidation a physiotherapy programme commences, in which more weight is gradually supported, increasing this by 25% of body weight every 2–3 weeks.
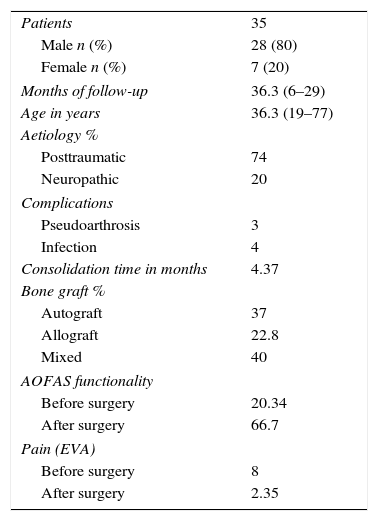
Results35 patients were evaluated: 7 (20%) women and 28 (80%) men. The average age was 36.3 years old, ranging from 19 to 77 years old and with a median age of 32 years old (Table 1).
Results.
| Patients | 35 |
| Male n (%) | 28 (80) |
| Female n (%) | 7 (20) |
| Months of follow-up | 36.3 (6–29) |
| Age in years | 36.3 (19–77) |
| Aetiology % | |
| Posttraumatic | 74 |
| Neuropathic | 20 |
| Complications | |
| Pseudoarthrosis | 3 |
| Infection | 4 |
| Consolidation time in months | 4.37 |
| Bone graft % | |
| Autograft | 37 |
| Allograft | 22.8 |
| Mixed | 40 |
| AOFAS functionality | |
| Before surgery | 20.34 |
| After surgery | 66.7 |
| Pain (EVA) | |
| Before surgery | 8 |
| After surgery | 2.35 |
Respecting the aetiology of the arthrosis, this was post-traumatic in 26 cases (74%), in the majority of cases secondary to wounds caused by fragmentation weapons or firearm projectiles; it was neuropathic in 7 cases (20%), chiefly due to diabetic arthropathy; it was metabolic in one case, caused by gout arthritis in one case (2.8%) and congenital in one case (2.8%) due to fibula hemimelia.
The graft used was autogenous from previously dried fibula in 13 cases (37.1%), an allograft (demineralised bone matrix) in 8 cases (22.8%) and combined in 14 cases (40%).
The bone took an average of 4.37 months to fuse, with a rate of joining as detected by X-ray of 91.4% at 6 months.
Among the complications which arose with this procedure, consolidation was delayed in 3 cases, due to which 2 were operated again and one is awaiting programmed revision surgery for arthrodesis, with a new placement of autogenous iliac crest bone graft. Secondly, there are 4 cases of infections at the site of the operation. 2 of these cases were resolved using antibiotics as outpatients, while the other 2 were resolved with the aid of surgical washing.
Functionality was evaluated using the AOFAS scale. The median functionality score before surgery was 20.34/100 points, and after surgery it was 66.7/100 points, with an overall improvement of 46 points on this scale with a value of P<.05. This shows a statistically significant improvement in the patients after the operation.
On the VAS pain scale the average score prior to surgery was 8, and after surgery it was 2.35. The average time taken to consolidate was 4.5 months, and patients began walking again without support or pain after 6 months.
DiscussionTTC arthrodesis using locked plates is a useful tool when it is necessary to fuse large bones, ones with defects and angular deformities that have to be corrected, and when the substrate is weakened bone and, in many cases, the soft tissues are in poor condition.
Several systems have been used historically and are now used to fix arthrodesis, including crossed screws, endomedular nails and even external fixation.
Several attempts have been made to determine which implant is superior in biomechanical terms.
Bennett et al.16 found that using 3 crossed screws gave better biomechanical stability than retrograde endomedular nails and 2 crossed screws. Chiodo et al.17 compared the use of retrograde nails with fixation using plates at a fixed angle and one screw. They found the latter system to be biomechanically superior in osteoporotic bone, with a low rate of complications and that it failed to join in 7–14% of cases.
Subsequently, Chodos et al.18 compared the use of a fixed angle plate with a plate locked at a variable angle. They found the latter to be more stable, a more rigid construct and able to support greater loads with less deformation. This is mainly due to the characteristics of the locking mechanism of the system and its divergence in the distal screws, which allows it to include more of the astralagus and calcaneus in the fixation.
In 2014, Heck et al.,19,20 in their study of 12 patients treated using TTC arthrodesis with a locked humeral plate, showed 100% consolidation and only one case of delayed consolidation, with an incidence of infection at the site of the operation of 15% that improved without any subsequent complications.
In our institution high energy trauma is the main cause of extensive lesions that compromise these joints, especially wounds caused by firearms and fragmentation weapons. We have therefore tried to standardise this technique with the aim of performing the procedure in a single operation while, together with achieving a suitable level of stability, correcting any deformities that may be present.
The results in our series of cases are similar to those in other works in the literature in terms of consolidation time, percentage of joining and functionality. It even shows fewer complications when compared with other patients having similar characteristics. In our experience, the locked humeral plate may be of use in patients with severely compromised bone at the level of the ankle that requires arthrodesis as rescue surgery and in patients with a very high risk of failure to join, while always understanding that it is an alternative form of management in comparison with different types of implants.
ConclusionThe patients included in this work presented a wide range of medical conditions that altered the bone quality and functioning of the joint. Nevertheless, a high rate of bone consolidation was achieved, with suitable stability of the construct and postoperative functionality. This is a reproducible technique that gives good postoperative results which agree with those reported in the literature, so that it should be taken into account when treating a patient with TTC arthrodesis.
Level of evidenceLevel of evidence iv.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Cabrera Méndez MP, Gamba C, Hernández E, Molano J, Andrade JC. Artrodesis tibiotalocalcánea con placa humeral bloqueada. Rev Esp Cir Ortop Traumatol. 2016;60:119–124.