The aim of this paper is to describe the prevalence of Delirium and the factors associated with its presentation and complications identified in a geriatric unit in Colombia.
Material and methodsThis is a retrospective observational study that included all patients admitted consecutively for two years in a geriatric unit of a hospital in Bogotá, Colombia. We assessed delirium prevalence with the Confusion Assessment Method (CAM). The independent variables were age, sex, functional impairment (Barthel<90), malnutrition (MNA<12), pressure ulcers at admission, state of the social support network, number of comorbidities, polypharmacy (5 or more drugs), complications such as ICU requirement, hospital stay, in-hospital functional impairment and mortality were also evaluated. As an exclusion criterion: not having CAM registered in the medical record, all the patients had this information.
ResultsWe studied 1599 subjects with a mean age of 86 years (IQR 9). Delirium prevalence was 51.03%. Delirium was associated with a higher rate of: pressure ulcers on admission [OR 3.76 (CI 2.60–5.43 p<0.001)], functional impairment [OR 2.38 (CI 1.79–3.16 p<0.001)], malnutrition [OR 2.06 (CI 1.56–2.73 p<0.001)], and infection [OR 1.46 (CI 1.17–1.82 p<0.001)]. Moreover delirium has a higher association with mortality [OR 2.80 (1.03–7.54 p=0.042)], in-hospital functional decline [OR 1.82 (1.41–2.36 p<0.001)], and longer hospital stay [OR 1.04 (1.04–1.09 p=0.006)]; independently of age, sex, pressure ulcers on admission, functional impairment, malnutrition, dementia, infection and limited social network.
ConclusionOur study suggests that infectious diseases and geriatric syndromes such as, functional dependence, pressure ulcers, malnutrition or major cognitive impairment are independently associated with the presence of delirium on admission. Additionally, the presence of delirium is independently associated during hospitalization with complications, longer hospital stay, functional impairment and mortality.
El objetivo de este trabajo es describir la prevalencia del delirium, los factores asociados a su presentación y sus complicaciones, en una unidad de geriatría en un hospital de Colombia.
Material y métodosEste es un estudio observacional retrospectivo en el que se incluyeron todos los pacientes ingresados de forma consecutiva durante 2 años, en una unidad geriátrica de un hospital en Bogotá, Colombia. Se evaluó la prevalencia del delirium con el método de evaluación de confusión (CAM). Las variables independientes fueron edad, sexo, dependencia funcional (Barthel <90), malnutrición (MNA<12), úlceras por presión al ingreso, estado de la red de apoyo social, número de comorbilidades, polifarmacia (5 o más fármacos), complicaciones tales como requerimiento de la UCI, también se evaluó la estancia hospitalaria, el deterioro funcional intrahospitalario y la mortalidad. Como criterio de exclusión: no contar con CAM registrado en la historia clínica, todos los pacientes contaban con esta información.
ResultadosEstudiamos 1.599 sujetos con una mediana de edad de 86 años (IQR: 9). La prevalencia del delirium fue del 51,03%. El delirium se asocia con la presencia de úlceras por presión al ingreso (OR: 3,76 [IC: 2,60-5,43; p<0,001]), dependencia funcional al ingreso (OR: 2,38 [IC: 1,79-3,16; p<0,001]), de malnutrición (OR: 2,06 [IC: 1,56-2,73; p<0,001]) y de infección (OR: 1,46 [IC: 1,17-1,82; p<0,001]). También se asocia con desenlaces adversos como la mortalidad (OR: 2,80 [1,03-7,54; p=0,042]), complicación hospitalaria (OR: 2,79 [1,68-4,63; p<0,001]), deterioro funcional intrahospitalario (OR: 1,82 [1,41-2,36; p<0,001]) y mayor estancia hospitalaria (OR: 1,04 [1,04-1,09; p=0,006]); esta asociación es independiente de la edad, el sexo, las úlceras por presión al ingreso, la dependencia funcional al ingreso y la malnutrición e infección.
ConclusiónNuestro estudio sugiere que las enfermedades infecciosas y los síndromes geriátricos como dependencia funcional, úlceras por presión, malnutrición o de deterioro cognitivo mayor se asocian de forma independiente a la presencia del delirium al ingreso. A su vez, la presencia del delirium se asocia de manera independiente durante la hospitalización con un mayor deterioro funcional, frecuencia de complicaciones, estancia hospitalaria media y mayor mortalidad.
Delirium is a geriatric syndrome that presents with an acute decline in cognitive functioning characterized by altered mental status and impaired attention.1–4 It can affect as much as 50% of older adults (those aged 65 and older).5 Its presentation is heterogeneous, having a sudden onset and a fluctuating course; further, it is often triggered by an underlying medical disorder.1,2 Delirium is a serious under recognized condition and often fatal, a formal cognitive assessment and history should be done detailing the onset and course of symptoms in order to make a precise diagnosis.5 Delirium might be preventable in up to 30–40% of the cases, making it a potential target to public health interventions.6,7 We can understand this condition as an acute brain failure, with evidence suggesting that it might lead to permanent cognitive decline and dementia in some patients.5
Although delirium is a prevalent condition related to adverse outcomes, there is a lack of clear estimates of its actual rates in low- and middle-income regions like in Latin America,8,9 precise estimates of delirium rates are necessary for service development in an increasing older population.5 Although the prevalence of delirium in the community is low, close to 1%, a recent review reports a prevalence of 18–35% at admission by medical and old age medicine wards.5 The incidence during a hospital stay ranges from 6% to 56% and is even higher in more specialized populations, for example 15–53% of surgical elderly patients develop postoperative delirium and in elderly patients in intensive care units the incidence can reach up to 70–87%.10 In Latin America and also in Colombia is hard to estimate the real prevalence and incidence of delirium because of under estimated diagnosis and lack of studies.
Delirium might be triggered by a single factor, but it is usually multifactorial, moreover it has been widely associated to other geriatric syndromes conditions such as cognitive impairment or dementia, multiple comorbidity, functional impairment and impaired mobility making older adults vulnerable to delirium,4,5 it is well related to adverse outcomes such as mortality, institutionalization and dependency,11 risk of falls, incontinency, pressure ulcers12,13 and therefore increased hospital costs.1,2
The importance of recognizing Delirium is to develop strategies for its prevention and its negative outcomes, regarding medical attention it is as well an attention quality indicator in geriatric patients because of the complexity of its treatment and its implications to hospital services.14 Despite the improvements in clinical assessment, delirium is still underdiagnosed, progressively increasing its burden. This article aims to give rate estimates concerning delirium and associated geriatric syndromes and common complications in a University Hospital benchmark in the management of the elderly, hoping to improve its prevention, early diagnosis and proper treatment.
MethodsStudy designThe present is a retrospective observational study. We used data from medical records from all the admitted patients in an Old age medicine ward at a University Hospital in Bogotá, the Hospital Universitario San Ignacio in the period between January 1 of 2016 and December 31 of 2017. Researchers of the Geriatrics department revised all medical records, following the protocol approved by the institutional ethics committees.
The Old medicine ward unit has the following criteria for admission: patients 75 years and older; patients with 60 years and older with at least one of the following criteria: multi-morbidity, chronic disability, polypharmacy, cognitive impairment, frequent hospitalization, social disturbances or any geriatric syndrome. We analyzed 1599 medical records, inclusion criteria comprised having a complete medical record containing the variables of interest, including the Confusion Assessment Method (CAM) evaluation, which the complete number of subjects had, since these variables are collected systematically for every patient following the institutional protocol. All the scales and indexes were assessed at admission and at discharge.
VariablesDependent variableOur dependent variable was Delirium. We assessed it at admission using the Confusion Assessment Method (CAM) we considered delirium was present if at least 3 of the 4 criteria were present. The delirium screening tool was applied to every patient admitted by the geriatrics service during the period of interest.
Independent variablesThe independent variables were: age measured in years; sex; functional impairment was defined using the Barthel index for activities of daily living (ADL), if the score was less than 90 and independent if equal or superior than 90. History of dementia reported at admission interview was used to create this variable. The malnutritional assessment in its short form (MNA-SF) was used for nutritional evaluation, then we considered normal nutritional status (12–14 points) and malnutrition, those at risk (8–11 points) and malnourished (7 points or less). We assessed pressure ulcers presence during the admission. Social network was evaluated as one of the main domains during the geriatric interview at admission, social risk was defined whether or not the patient identified an adequate support network, patients were classified into 3 categories: strong social network, social risk, poor social network, we used it as a dichotomic variable; strong or limited social network for the social risk and poor social network. Number of comorbidities and polypharmacy were explored during the admission and used as a continuous variable. Polypharmacy was defined as the use of 5 or more medicines daily.
We report Hospital stay in days. Readmission was defined as patients that had been hospitalized in the previous 20 days for the same cause. We clustered the diagnosis in those with infectious diseases and others by dichotomizing the variable. We also evaluated during the patient hospitalization in-hospital functional decline with a loss of 10 or more points in Barthel index for ADL on discharge compared to baseline. Complications included infections (except respiratory, gastrointestinal and urinary infections), other complications concerned cardiovascular, respiratory, gastrointestinal, endocrinological, hematological, psychiatric, thrombotic and dermatological conditions presented during hospitalization, Intensive Care Unit (ICU) requirement and mortality were dichotomized.
Statistical analysisAfter making an exploratory analysis, we carried a descriptive analysis using the previous variables, reporting the number of events and percentage values, we used median and interquartile range for the continuous variables with no parametric distribution. Bivariate models were then used to identify associations with delirium. We analyzed delirium first as a dichotomous variable. We used Chi-square tests to compare with categorical variables, and for continuous variables with no-normal distribution we used a U-Mann–Whitney test.
Finally, we made a multivariate regression model adjusting by sex, age and independent variables, obtaining an odds ratio (OR) with 95% confidence intervals (CI), unadjusted and adjusted for confounding variables. We set the statistical level of significance at p<0.05. Data was analyzed using STATA 14®.
Ethical issuesThe study was approved by research an ethics committee at the Hospital Universitario San Ignacio and Pontificia Universidad Javeriana.
ResultsWe studied 1599 patients with a mean age of 84.87±6.55 years vs 85.84±6.07 years. In the delirium group the majority were female, 57.29%. The Barthel scale at admission had a median of 50 (IQR 70). 1091 subjects had dementia (68.23%) and 79.86% malnutrition. 228 patients presented pressure ulcers at admission (14.25%). 259 had a limited social network (16.19%). The mean number of comorbidities was of 5 (IQR 3). 1018 patients had polypharmacy at admission (63.66%). The mean days of hospitalization was 5 (IQR 5). 608 of the patients had an infection (38.02%). 213 of the subjects were readmitted patients (13.32%). 469 presented in-hospital functional decline (29.33%) and 148 had in-hospital complications (9.26%). Finally, 66 patients required Intensive Care Unit (4.13%) and 195 died during hospitalization (12.19%).
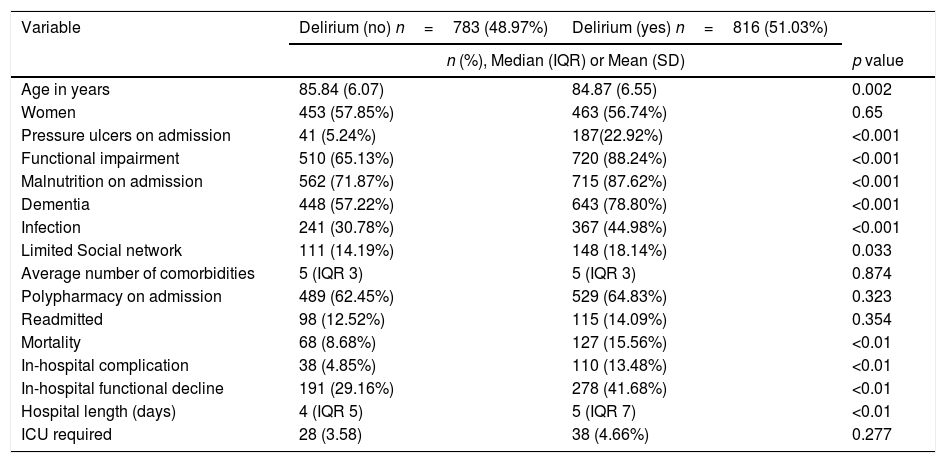
We show bivariate analysis and the population characteristics of both groups in Table 1. We found significant differences in the following variables: Mean age was 86 years for both groups, IQR of 8 for the delirium group and of 9 for the no-delirium group (p<0.01). In the delirium group, 187 (22.92%) patients presented pressure ulcers at admission compared to 41 (5.24%) in the non-delirium group (p<0.01). In the delirium group, functional impairment was present in 720 (88.24%) and in the non-delirium group 510 (65.13%) (p<0.01). Regarding malnutrition, 715 (87.62%) patients presented it in the delirium group while in the non-delirium it was present in 562 (71.87%) (p<0.01), one patient missed information about this diagnosis on admission. Dementia prevalence was 643 (78.80%) in the delirium group vs 448 (57.22%) (p<0.01) The 44.98% of the patients in the delirium group had an infection diagnosis at admission compared to the 30.87% in the non-delirium group (p<0.01). We found 57% of patients in the delirium group had limited social network, comparing to 43% in the non-delirium group (p=0.03), one patient missed information about social network.
Baseline characteristics according the presence or not of delirium during hospitalization.
| Variable | Delirium (no) n=783 (48.97%) | Delirium (yes) n=816 (51.03%) | |
|---|---|---|---|
| n (%), Median (IQR) or Mean (SD) | p value | ||
| Age in years | 85.84 (6.07) | 84.87 (6.55) | 0.002 |
| Women | 453 (57.85%) | 463 (56.74%) | 0.65 |
| Pressure ulcers on admission | 41 (5.24%) | 187(22.92%) | <0.001 |
| Functional impairment | 510 (65.13%) | 720 (88.24%) | <0.001 |
| Malnutrition on admission | 562 (71.87%) | 715 (87.62%) | <0.001 |
| Dementia | 448 (57.22%) | 643 (78.80%) | <0.001 |
| Infection | 241 (30.78%) | 367 (44.98%) | <0.001 |
| Limited Social network | 111 (14.19%) | 148 (18.14%) | 0.033 |
| Average number of comorbidities | 5 (IQR 3) | 5 (IQR 3) | 0.874 |
| Polypharmacy on admission | 489 (62.45%) | 529 (64.83%) | 0.323 |
| Readmitted | 98 (12.52%) | 115 (14.09%) | 0.354 |
| Mortality | 68 (8.68%) | 127 (15.56%) | <0.01 |
| In-hospital complication | 38 (4.85%) | 110 (13.48%) | <0.01 |
| In-hospital functional decline | 191 (29.16%) | 278 (41.68%) | <0.01 |
| Hospital length (days) | 4 (IQR 5) | 5 (IQR 7) | <0.01 |
| ICU required | 28 (3.58) | 38 (4.66%) | 0.277 |
IQR, interquartile range.
15.56% patients died in the delirium group in comparison with the 8.68% patients of the no delirium group. (p<0.01). In-hospital complication was present in 13.48% patients in the delirium group and in 4.85% in the non-delirium group (p<0.01). In-hospital functional decline presented in 278 (41.68%) patients in the delirium group and in 191 (29.16%) in the non-delirium group (p<0.01). And finally, the mean hospital stay was 5 days (IQR 7) for the delirium group and 4 days (IQR 5) for the non-delirium group (p<0.014).
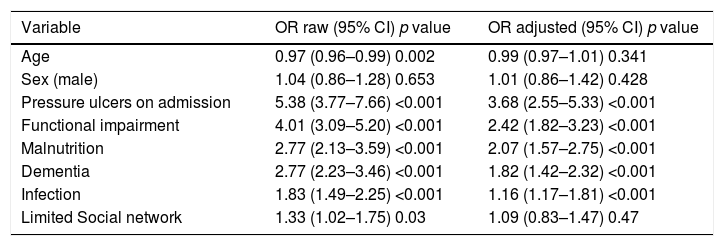
Risk factors associated with delirium presentation were: pressure ulcers at admission OR 5.38 (CI 3.77–7.66 p<0.001), Functional impairment OR 4.01 (95% CI 3.09–5.20 p<0.001), Malnutrition OR 2.77 (CI 2.13–3.59 p<0.001), history of dementia OR 2.77 (CI 2.23–3.46 p<0.001), Infectious disease at admission OR 1.83 (CI 1.49–2.25 p<0.001), Limited social network OR 1.33 (CI 1.02–1.75 p=0.03). After adjusting for sex, age and each of the outcomes and risk factors presented in Table 2 delirium showed independent associations with: Pressure ulcers at admission OR 3.76 (IC 2.60–5.43 p<0.001) Functional impairment shows an OR of 2.38 (CI 1.79–3.16 p<0.001), Malnutrition OR 2.06 (CI 1.56–2.73 p<0.001), Dementia had an OR 1.82 (CI 1.43–3.06 p<0.001), Infection OR 1.46 (CI 1.17–1.82 p<0.001), Limited social network at admission OR 1.11 (CI 0.82–1.49 p=0.47).
Factors associated with delirium prevalence during hospitalization: Multivariate analysis.
| Variable | OR raw (95% CI) p value | OR adjusted (95% CI) p value |
|---|---|---|
| Age | 0.97 (0.96–0.99) 0.002 | 0.99 (0.97–1.01) 0.341 |
| Sex (male) | 1.04 (0.86–1.28) 0.653 | 1.01 (0.86–1.42) 0.428 |
| Pressure ulcers on admission | 5.38 (3.77–7.66) <0.001 | 3.68 (2.55–5.33) <0.001 |
| Functional impairment | 4.01 (3.09–5.20) <0.001 | 2.42 (1.82–3.23) <0.001 |
| Malnutrition | 2.77 (2.13–3.59) <0.001 | 2.07 (1.57–2.75) <0.001 |
| Dementia | 2.77 (2.23–3.46) <0.001 | 1.82 (1.42–2.32) <0.001 |
| Infection | 1.83 (1.49–2.25) <0.001 | 1.16 (1.17–1.81) <0.001 |
| Limited Social network | 1.33 (1.02–1.75) 0.03 | 1.09 (0.83–1.47) 0.47 |
OR, odds ratio; CI, confidence interval, adjusted by age and sex, pressure ulcers, functional impairment, malnutrition, dementia, infection and limited social network.
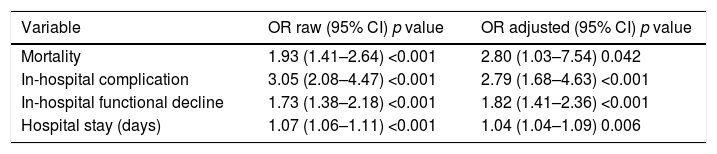
Regarding negative outcomes: with: In-hospital functional decline OR 1.73 (CI 1.38–2.18 p<0.001). Hospital stay OR 1.08 (CI 1.06–1.11 p<0.001). In-hospital complication OR 3.05 (CI 2.08–4.47 p<0.001) (Table 2). And Mortality OR 1.93 (CI 1.41–2.46 p<0.001) for delirium. When adjusting for sex, age and each of the outcomes and risk factors presented in Table 2 delirium showed independent associations with: Mortality OR 2.80 (1.03–7.54 p=0.042), In- hospital complication OR 2.79 (1.68–4.63 p<0.001) In–hospital functional decline OR 1.82 (1.41–2.36 p<0.001). For Hospital stay OR 1.04 (1.04–1.09 p=0.006) (Table 3).
Negative outcomes associated with delirium during hospitalization: Multivariate analysis.
| Variable | OR raw (95% CI) p value | OR adjusted (95% CI) p value |
|---|---|---|
| Mortality | 1.93 (1.41–2.64) <0.001 | 2.80 (1.03–7.54) 0.042 |
| In-hospital complication | 3.05 (2.08–4.47) <0.001 | 2.79 (1.68–4.63) <0.001 |
| In-hospital functional decline | 1.73 (1.38–2.18) <0.001 | 1.82 (1.41–2.36) <0.001 |
| Hospital stay (days) | 1.07 (1.06–1.11) <0.001 | 1.04 (1.04–1.09) 0.006 |
OR, odds ratio; CI, confidence interval, adjusted by age, sex, risk factors presented in Table 2, mortality, in-hospital complication, in-hospital functional decline and hospital stay.
To our knowledge this is the first in-hospital geriatric study in Colombia evaluating associated factors to delirium. prevalence during admission was 51.03%, higher than previous publications in other countries; in a Saudi elderly population, a prevalence of 21.8% in the first 24h of admission was found.15 In the multicentric Italian Delirium Day study, the prevalence was of 22.9% in a population of 1867 older patients across 108 acute and 12 rehabilitation wards in Italian hospitals16 and a systematic review shows a prevalence of delirium during the admission ranged from 10 to 31%.8 Only in one study among elderly hospitalized patients in a single hospital in India the prevalence was of 53%.17 In Latin America, one study in Chile found a prevalence of 35.4%.14 This differences in the prevalence could be explained by a higher prevalence of polypharmacy and multimorbidity treated in our institution as a reference center.18,19 or due to a higher frequency of diagnosis given our systematic evaluation of the CAM to all patients on admission.
Additionally, our sample is older in comparison with a mean age of 86 years in comparison to reported ranges explored by a systematic review with mean ages range of 68.8–84.8 years having 40 studies evaluated.8 This could be significant explaining the higher prevalence of Delirium in our sample, this association was significant in the multivariate analysis, however when adjusting for confounding factors, age lost significance, this is important to highlight the importance of other conditions and geriatric symptoms since age is not the only predisposal for delirium onset.
Geriatric syndromes like malnutrition, were higher on admission in the delirium group. This agrees with the literature that has shown malnutrition as risk factor for delirium, as demonstrated in the systematic review and meta-analysis conducted by Suman Ahmed et al.18,20 Nutritional status plays an important role in delirium development,21 this can affect cognitive status and restoring nutritional balance could lead to resolution of delirium.22 Finally, when performing the multivariate analyzes we found a positive relationship between delirium and malnutrition.
Pressure ulcers during admission were significantly more frequent in the population with delirium. These findings correlate with previous publications in which individuals with delirium developed more pressure ulcers in comparison with those without delirium.3,23 This association could be explained due to stress, inflammation and infection triggered by the injury itself,23,24 malnutrition and immobility that led to develop of both entities.25 In our multivariate analysis a positive relationship was found between delirium and pressure ulcers.
Functional impairment has been described in the literature as a predisposing factor for the development of delirium.4,26 Our results agree with this statement, since, regarding the previous functional status, the prevalence of patients with functional impairment was higher in the delirium than in the no-delirium group, we also found an independent association as well. These results agree with the results of the “Delirium day” study, which evaluated the functional status prior to admission with the Activities of Daily Living (ADL) score, with a positive association between delirium and functional impairment.16 The multiple comorbidities and the high prevalence of dementia increase the impact of functional impairment and increase the risk of delirium.10,25
Dementia displayed a higher prevalence in the delirium Group. We also found an independent significant association between dementia and delirium. This association has been widely described, and the current understanding is still subject of controversy.4,18,25,27,28 In elderly patients is the most important predisposal risk factors for delirium, being present in up to two-thirds of all cases of delirium. Both conditions are associated with decreased cerebral blood flow or metabolism, cholinergic deficiency, and inflammation.10 These results are similar to other population-based cohort study, which found delirium increased the risk of incident dementia.29 And with the results of the “Delirium day” study, in which dementia was associated with delirium.16
We also found and association between delirium and infectious disease at admission which had been classified as a precipitant risk factor of delirium.18,30 We found a higher prevalence of infectious diseases on admission in the delirium group. Furthermore, we found an independent association between infectious diseases and delirium. A cohort study conducted in Colombia by Torres-Contreras found the same association.26 A limited social network was more common in the delirium group which may be related to isolation, poor medication control, low access to preventive and medical services, allowing disease progression and a greater functional decline before going consulting medical services.31–33 There are other risk and precipitating factors that have been described in the development of delirium including alcohol abuse, psychoactive medication use, history of transient ischemia/stroke, dehydration, illness severity, hearing and vision impairment and surgery. However, we did not include these in our study which might be important in further studies in our population.5
Complications among the delirium group were also higher, the frequency of functional decline was higher in the delirium group, similar results have been seen in other cross-sectional studies.34,35 Patients are highly susceptible to different stressors, which at the same time contribute to the presentation of complications and functional decline.36 Hospitalizations were longer in the delirium group, there was as well an independent association with hospital stay. A systematic review, showed an increased hospital in delirium groups.20
Finally, mortality in the bivariate analysis was higher in the delirium group, and when performing the multivariate analysis, the patients with delirium were more likely to die during hospitalization. This association was independent to all other outcomes, as well to associated risk factors (Table 2) such as previous functional decline, dementia and comorbidities, etc. This has been previously reported in different studies, in which the patients with delirium were more likely to experience 90-day mortality 24% vs. 6%.3,8 This outcome could be explained by the accumulation of all the comorbidities described, development of hospital-acquired conditions, the need for additional interventions, functional decline presented at baseline.3 However it is important to highlight we adjusted for these other conditions and the association remained significant.
Our study has some limitations, as a cross sectional study causality cannot be inferred, neither can we establish a directionality. The conclusions described are the result of the interpretation of the data by the authors with a previous knowledge of the pathophysiology of the aforementioned pathologies and the possible course of the disease. Some strengths of our study include the validity given by previous studies reporting similar results, as well as the associations that were statistically significant most of the time.
Although this is a retrospective study information was collected systematically, additionally there was almost no loss of information, since only two patients missed information on the controlled variables of malnutrition and social network. Moreover, the sample was pooled from a reference center regarding Old age medicine. Thanks to the results of this study we hope that by revealing some of the associated factors of this entity, efforts can be maximized for prevention and to diminish the impact of its complications.
ConclusionThe results of this study show statistically significant associations between delirium at admission and presence of other geriatric syndromes like functional impairment, malnutrition, pressure ulcers, cognitive decline, multiple comorbidities and polypharmacy. Presence of these factors should alert physicians including geriatricians and other practitioners on patients who are at a higher risk of presenting delirium in whom delirium should be ruled out and prevention strategies applied as well. Functional impairment, malnutrition, pressure ulcers and polypharmacy for instance can potentially be modified or prevented, and use as a target to prevent delirium and its complications in the older adults.
Delirium is not a presented as a mere consequence of aging, but rather of other geriatric syndromes or of conditions. Additionally, our results show for the first time in the Colombian population independent associations with negative outcomes like in-hospital deterioration, increased hospital length, in-hospital complications and mortality. This gives an insight to challenges presented in older adults with delirium, we recommend further research addressing risk factors on local communities in order to prompt decision makers to develop public health strategies for delirium prevention and management in older adults.
Source of fundingThis study was supported by the Hospital Universitario San Ignacio. This research did not receive any funding from agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestsNone.
We thank to all the members of the student research group: Semillero de Neurociencias y Envejecimiento from the Pontifical Xavierian University. Bogotá, Colombia. And the Ageing institute at Hospital Universitario San Ignacio.