Article

Revista Española de Medicina Nuclear e Imagen Molecular (English Edition)
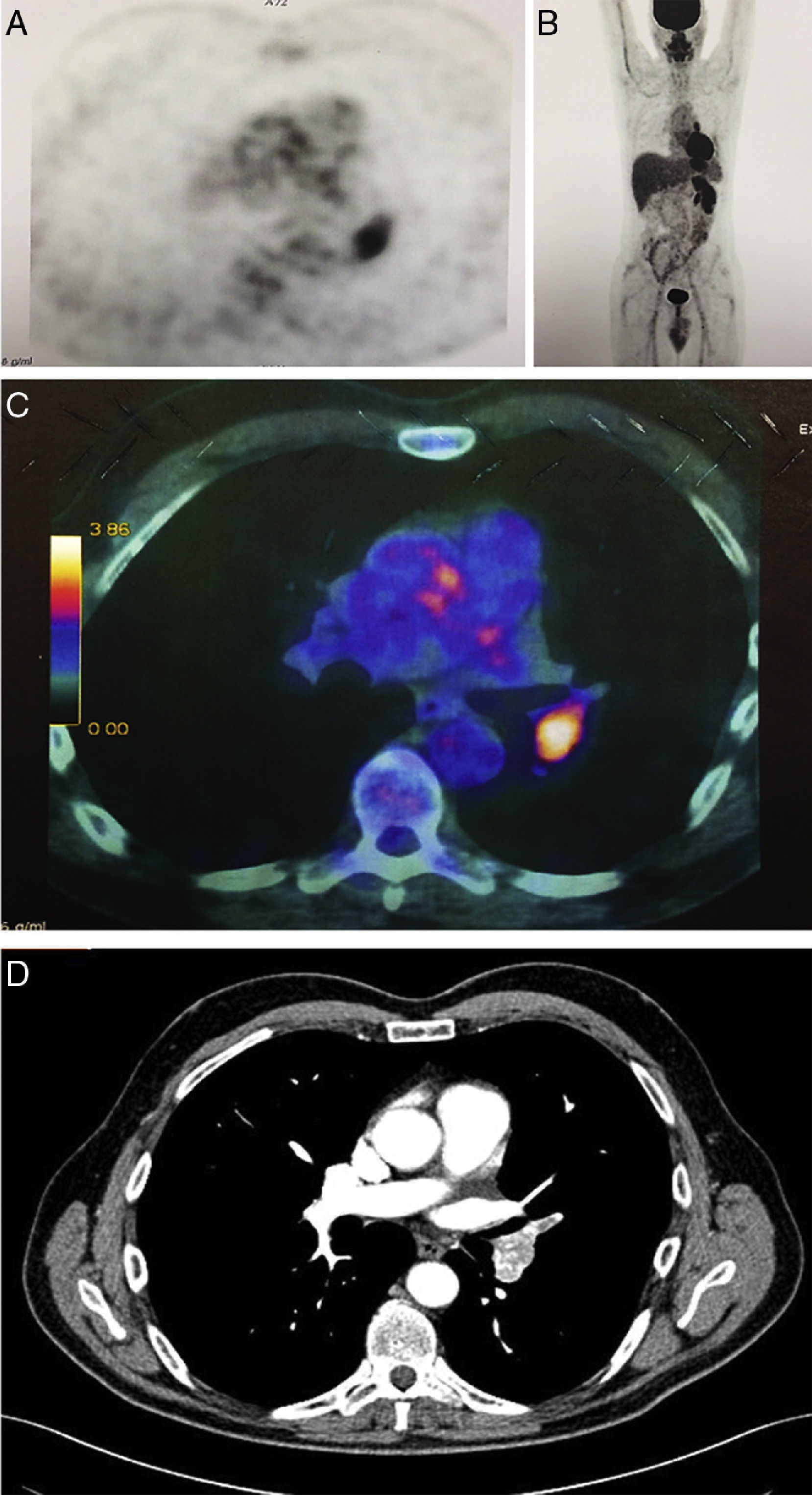
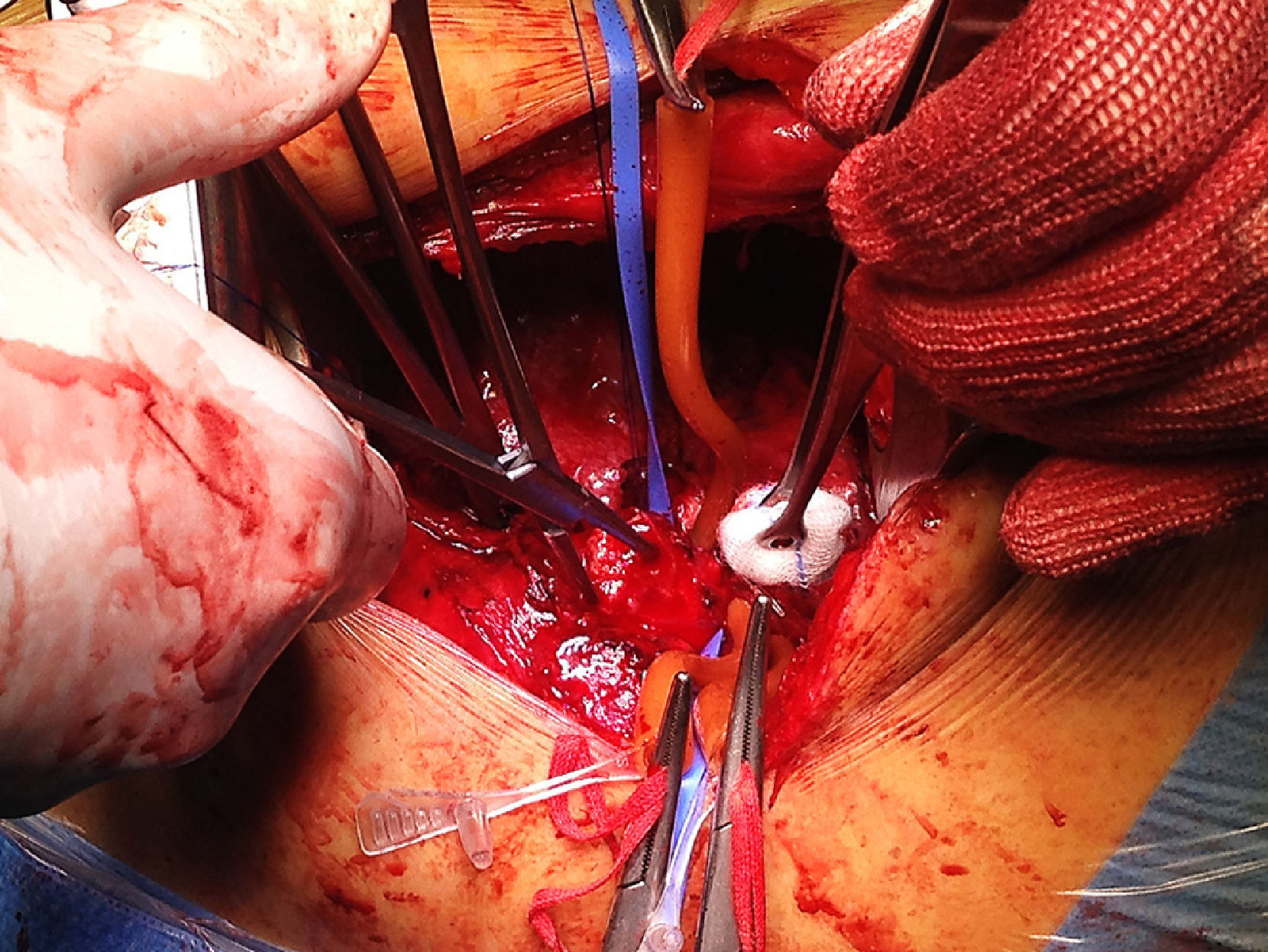
array:23 [ "pii" => "S2253808915000841" "issn" => "22538089" "doi" => "10.1016/j.remnie.2015.07.010" "estado" => "S300" "fechaPublicacion" => "2015-09-01" "aid" => "667" "copyright" => "Elsevier España, S.L.U. and SEMNIM" "copyrightAnyo" => "2014" "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Rev Esp Med Nucl Imagen Mol. 2015;34:325-6" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:2 [ "total" => 100 "formatos" => array:2 [ "HTML" => 20 "PDF" => 80 ] ] "itemSiguiente" => array:18 [ "pii" => "S2253808915000853" "issn" => "22538089" "doi" => "10.1016/j.remnie.2015.07.011" "estado" => "S300" "fechaPublicacion" => "2015-09-01" "aid" => "671" "copyright" => "Elsevier España, S.L.U. and SEMNIM" "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Rev Esp Med Nucl Imagen Mol. 2015;34:327-8" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:2 [ "total" => 98 "formatos" => array:2 [ "HTML" => 12 "PDF" => 86 ] ] "en" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Interesting images</span>" "titulo" => "An 18-year delay in the clinical presentation of bronchial carcinoid" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "327" "paginaFinal" => "328" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Retraso de 18 años en la presentación clínica de carcinoide bronquial" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Figure 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 2334 "Ancho" => 1668 "Tamanyo" => 614710 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">(A) CT scan performed in 1996: the image evidences a round-shaped solid nodule (measuring 21<span class="elsevierStyleHsp" style=""></span>mm in the major axis) localized near to the apical bronchus of the right lower lobe. The clinical diagnosis was consistent with intrapulmonary lymph-node associated to tuberculosis. (B) CT scan performed 18 years after: CT slice demonstrates the enlargement of the lung nodule (26<span class="elsevierStyleHsp" style=""></span>mm in the major axis). (C) Whole body PET/CT performed 1<span class="elsevierStyleHsp" style=""></span>h after the administration of 296<span class="elsevierStyleHsp" style=""></span>MBq of <span class="elsevierStyleSup">18</span>FDG (axial, coronal and sagittal slices): the images evidenced an increased uptake of a round-shaped solid nodule of the right lower lobe (SUV max 4.7). No sign of mediastinal or extra-thoracic disease was disclosed.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Giovanni Leuzzi, Daniele Forcella, Enrico Melis, Paolo Visca, Francesco Facciolo" "autores" => array:5 [ 0 => array:2 [ "nombre" => "Giovanni" "apellidos" => "Leuzzi" ] 1 => array:2 [ "nombre" => "Daniele" "apellidos" => "Forcella" ] 2 => array:2 [ "nombre" => "Enrico" "apellidos" => "Melis" ] 3 => array:2 [ "nombre" => "Paolo" "apellidos" => "Visca" ] 4 => array:2 [ "nombre" => "Francesco" "apellidos" => "Facciolo" ] ] ] ] ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2253808915000853?idApp=UINPBA00004N" "url" => "/22538089/0000003400000005/v1_201508130058/S2253808915000853/v1_201508130058/en/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S2253808915000750" "issn" => "22538089" "doi" => "10.1016/j.remnie.2015.07.001" "estado" => "S300" "fechaPublicacion" => "2015-09-01" "aid" => "684" "copyright" => "Elsevier España, S.L.U. and SEMNIM" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "crp" "cita" => "Rev Esp Med Nucl Imagen Mol. 2015;34:321-4" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:2 [ "total" => 204 "formatos" => array:2 [ "HTML" => 39 "PDF" => 165 ] ] "en" => array:13 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Clinical note</span>" "titulo" => "<span class="elsevierStyleSup">111</span>In-octreotide SPECT–CT in head and neck paragangliomas" "tienePdf" => "en" "tieneTextoCompleto" => "en" "tieneResumen" => array:2 [ 0 => "en" 1 => "es" ] "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "321" "paginaFinal" => "324" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "SPECT-TC con <span class="elsevierStyleSup">111</span>In-octreotide en paragangliomas de cabeza y cuello" ] ] "contieneResumen" => array:2 [ "en" => true "es" => true ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0010" "etiqueta" => "Figure 2" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr2.jpeg" "Alto" => 857 "Ancho" => 2500 "Tamanyo" => 108767 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0030" class="elsevierStyleSimplePara elsevierViewall">Clinical case 2. Resected paraganglioma in left mastoid lesion. (A) SPECT with <span class="elsevierStyleSup">111</span>In-octreotide showing left nodular lesion with high expression of SSR; (B) MR: lesion in the anterior wall of the tympanic cavity which does not differentiate between residual tissue, recurrence or scar tissue; (C) fused images of SPECT-MR. Characterization of persistent post-surgical tumour tissue.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "C. Castillo-Berrio, M. Castrillón, F. Zelaya, D. Ruíz, F. Loira, J.M. Nogueiras, A. López, R. Guitián, J. Outomuro, A. Serena, L.M. Campos" "autores" => array:11 [ 0 => array:2 [ "nombre" => "C." "apellidos" => "Castillo-Berrio" ] 1 => array:2 [ "nombre" => "M." "apellidos" => "Castrillón" ] 2 => array:2 [ "nombre" => "F." "apellidos" => "Zelaya" ] 3 => array:2 [ "nombre" => "D." "apellidos" => "Ruíz" ] 4 => array:2 [ "nombre" => "F." "apellidos" => "Loira" ] 5 => array:2 [ "nombre" => "J.M." "apellidos" => "Nogueiras" ] 6 => array:2 [ "nombre" => "A." "apellidos" => "López" ] 7 => array:2 [ "nombre" => "R." "apellidos" => "Guitián" ] 8 => array:2 [ "nombre" => "J." "apellidos" => "Outomuro" ] 9 => array:2 [ "nombre" => "A." "apellidos" => "Serena" ] 10 => array:2 [ "nombre" => "L.M." "apellidos" => "Campos" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S2253654X1500027X" "doi" => "10.1016/j.remn.2015.02.007" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2253654X1500027X?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2253808915000750?idApp=UINPBA00004N" "url" => "/22538089/0000003400000005/v1_201508130058/S2253808915000750/v1_201508130058/en/main.assets" ] "en" => array:16 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Interesting image</span>" "titulo" => "Pulmonary tumor embolus with high <span class="elsevierStyleSup">18</span>FDG uptake mimicking lung metastasis from renal-cell cancer" "tieneTextoCompleto" => true "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "325" "paginaFinal" => "326" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "Giovanni Leuzzi, Enrico Melis, Daniele Forcella, Francesco Facciolo" "autores" => array:4 [ 0 => array:4 [ "nombre" => "Giovanni" "apellidos" => "Leuzzi" "email" => array:1 [ 0 => "gio.leuzzi@yahoo.it" ] "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">*</span>" "identificador" => "cor0005" ] ] ] 1 => array:2 [ "nombre" => "Enrico" "apellidos" => "Melis" ] 2 => array:2 [ "nombre" => "Daniele" "apellidos" => "Forcella" ] 3 => array:2 [ "nombre" => "Francesco" "apellidos" => "Facciolo" ] ] "afiliaciones" => array:1 [ 0 => array:2 [ "entidad" => "Department of Surgical Oncology, Thoracic Surgery Unit, Regina Elena National Cancer Institute, IFO, Rome, Italy" "identificador" => "aff0005" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Embolia pulmonar tumoral con alta captación de <span class="elsevierStyleSup">18</span>FDG imitando metástasis pulmonar de cáncer de células renales" ] ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0010" "etiqueta" => "Fig. 2" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr2.jpeg" "Alto" => 1246 "Ancho" => 1660 "Tamanyo" => 490579 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">Intraoperative findings: after arteriotomy of the lower pulmonary artery, an attempt to remove the thrombus was performed. Due to macroscopic infiltration of the arterial posterior wall, a left lower lobectomy was carried out in order to obtain a radical resection. Final pathology was consistent with tumor embolus from RCC.</p>" ] ] ] "textoCompleto" => "<span class="elsevierStyleSections"><p id="par0005" class="elsevierStylePara elsevierViewall">A 60-year-old Caucasian man referred to our Department for chest pain and dry cough from 15 days. His medical history was unremarkable with the exception of renal-cell cancer (RCC) diagnosed and resected six months earlier by a right radical nephrectomy. Few days before the admission, a whole body <span class="elsevierStyleSup">18</span>FDG positron emission tomography (PET-CT) scan was performed: nuclear images evidenced a left hilar hyper-metabolism (SUV max 6.7) suggestive of intrapulmonary recurrence (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>A–C). After the admission, due to symptoms aggravation, a contrast-enhanced computed tomography (CT) scan was carried out disclosing a hyper-vascularized solid nodule (measuring 19<span class="elsevierStyleHsp" style=""></span>mm in the major axis) localized into the left inferior pulmonary artery and with extension through the lingular artery (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>D), consistent with tumor embolus. After a multidisciplinary meeting, the patient underwent surgery in order to obtain immediate arterial desobstruction. Intra-operatively, an infiltration of the vascular posterior wall was disclosed (<a class="elsevierStyleCrossRef" href="#fig0010">Fig. 2</a>) so the patient underwent a left lower lobectomy for radical intent without complication. Final pathology was consistent with RCC embolus. No evidence of recurrence was found at 1 year of follow-up.</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><elsevierMultimedia ident="fig0010"></elsevierMultimedia><p id="par0010" class="elsevierStylePara elsevierViewall">In literature, thrombosis in cancer patients is usually reported, while tumor thrombosis is very uncommon. As a rule, such complication may develop in patients with tumors arising from liver, pancreas, kidney and colon as a result of direct infiltration of vena cava or other major vessels.<a class="elsevierStyleCrossRef" href="#bib0020"><span class="elsevierStyleSup">1</span></a></p><p id="par0015" class="elsevierStylePara elsevierViewall">In this setting, discrimination between regular and tumor thrombus is a challenging clinical issue in RCC patients<a class="elsevierStyleCrossRef" href="#bib0025"><span class="elsevierStyleSup">2</span></a> because of the different treatments proposed (antithrombotic therapy vs endovascular/surgical removal). PET-CT has been evaluated by others in the assessment of embolism, however, due to low sensitivity rate reported, its utility for metastases identification is still controversial in RCC.<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">3</span></a></p><p id="par0020" class="elsevierStylePara elsevierViewall">According to these findings and to the case we presented, we believe that contrast-enhanced CT scan may be more sensitive in diagnosing lung tumor embolism. When this condition is suspected, radiological (CT-scan) and nuclear (PET-CT) imaging should be jointly employed in order to obtain a more accurate evaluation in RCC patients and to distinguish between benign or malignant thrombus and lung metastases. Furthermore, a thromboarteriectomy (and pulmonary resection if vascular infiltration is evidenced) is mandatory to perform oncological and vascular treatment simultaneously.</p><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0005">Conflict of interest</span><p id="par0025" class="elsevierStylePara elsevierViewall">None declared.</p></span></span>" "textoCompletoSecciones" => array:1 [ "secciones" => array:2 [ 0 => array:2 [ "identificador" => "sec0005" "titulo" => "Conflict of interest" ] 1 => array:1 [ "titulo" => "References" ] ] ] "pdfFichero" => "main.pdf" "tienePdf" => true "fechaRecibido" => "2014-11-21" "fechaAceptado" => "2014-12-16" "multimedia" => array:2 [ 0 => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 3051 "Ancho" => 1658 "Tamanyo" => 437233 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">(A–C) Whole body PET-CT performed 1<span class="elsevierStyleHsp" style=""></span>h after the administration of 296<span class="elsevierStyleHsp" style=""></span>MBq of <span class="elsevierStyleSup">18</span>FDG: the images evidenced an increased uptake of a round-shaped solid nodule localized in the left pulmonary hilum (SUV max 6.7). No sign of mediastinal or extra-thoracic disease was disclosed. (D) Contrast-enhanced CT scan performed after patient's admission: CT slice showed a hyper-vascularized solid nodule (measuring 19<span class="elsevierStyleHsp" style=""></span>mm in the major axis) localized into the left inferior pulmonary artery and with extension through the lingular artery. Based on nuclear and radiological imaging, a diagnosis of tumor thrombus was achieved.</p>" ] ] 1 => array:7 [ "identificador" => "fig0010" "etiqueta" => "Fig. 2" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr2.jpeg" "Alto" => 1246 "Ancho" => 1660 "Tamanyo" => 490579 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">Intraoperative findings: after arteriotomy of the lower pulmonary artery, an attempt to remove the thrombus was performed. Due to macroscopic infiltration of the arterial posterior wall, a left lower lobectomy was carried out in order to obtain a radical resection. Final pathology was consistent with tumor embolus from RCC.</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0005" "bibliografiaReferencia" => array:3 [ 0 => array:3 [ "identificador" => "bib0020" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Malignancies, prothrombotic mutations, and the risk of venous thrombosis" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "J.W. Blom" 1 => "C.J. Doggen" 2 => "S. Osanto" 3 => "F.R. Rosendaal" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1001/jama.293.6.715" "Revista" => array:6 [ "tituloSerie" => "JAMA" "fecha" => "2005" "volumen" => "293" "paginaInicial" => "715" "paginaFinal" => "722" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/15701913" "web" => "Medline" ] ] ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0025" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Positron emission tomography-computed tomography imaging characteristics of an inferior vena cava tumor thrombus with magnetic resonance imaging correlation" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "J.N. Rydberg" 1 => "G.S. Sudakoff" 2 => "R.S. Hellman" 3 => "W.A. See" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "J Comput Assist Tomogr" "fecha" => "2004" "volumen" => "28" "paginaInicial" => "517" "paginaFinal" => "519" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/15232383" "web" => "Medline" ] ] ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0030" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Positron emission tomography enhancing tumor thrombus in patient with renal cell carcinoma" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "D. Snow" 1 => "D. Cohen" 2 => "W.C. Chapman" 3 => "R.L. Grubb 3rd" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.urology.2008.08.463" "Revista" => array:6 [ "tituloSerie" => "Urology" "fecha" => "2009" "volumen" => "73" "paginaInicial" => "270" "paginaFinal" => "271" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/18950838" "web" => "Medline" ] ] ] ] ] ] ] ] ] ] ] ] ] "idiomaDefecto" => "en" "url" => "/22538089/0000003400000005/v1_201508130058/S2253808915000841/v1_201508130058/en/main.assets" "Apartado" => array:4 [ "identificador" => "7927" "tipo" => "SECCION" "en" => array:2 [ "titulo" => "Interesting images" "idiomaDefecto" => true ] "idiomaDefecto" => "en" ] "PDF" => "https://static.elsevier.es/multimedia/22538089/0000003400000005/v1_201508130058/S2253808915000841/v1_201508130058/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2253808915000841?idApp=UINPBA00004N" ]
Consulte los artículos y contenidos publicados en éste medio, además de los e-sumarios de las revistas científicas en el mismo momento de publicación
Esté informado en todo momento gracias a las alertas y novedades
Acceda a promociones exclusivas en suscripciones, lanzamientos y cursos acreditados
The Revista Española de Medicina Nuclear e Imagen Molecular (Spanish Journal of Nuclear Medicine and Molecular Imaging), was founded in 1982, and is the official journal of the Spanish Society of Nuclear Medicine and Molecular Imaging, which has more than 700 members. The Journal, which publishes 6 regular issues per year, has the promotion of research and continuing education in all fields of Nuclear Medicine as its main aim. For this, its principal sections are Originals, Clinical Notes, Images of Interest, and Special Collaboration articles. The works may be submitted in Spanish or English and are subjected to a peer review process. In 2009, it became the leading Spanish journal in the field of Medical Imaging on having an Impact Factor , awarded by the Journal Citation Reports.
Science Citation Index Expander, Medline, IME, Bibliomed, EMBASE/Excerpta Medica, Healthstar, Cancerlit, Toxine, Inside Conferences, Scopus
See moreThe Impact Factor measures the average number of citations received in a particular year by papers published in the journal during the two preceding years.
© Clarivate Analytics, Journal Citation Reports 2022
SRJ is a prestige metric based on the idea that not all citations are the same. SJR uses a similar algorithm as the Google page rank; it provides a quantitative and qualitative measure of the journal's impact.
See moreSNIP measures contextual citation impact by wighting citations based on the total number of citations in a subject field.
See more
Revista Española de Medicina Nuclear e Imagen Molecular (English Edition)

¿Es usted profesional sanitario apto para prescribir o dispensar medicamentos?
Are you a health professional able to prescribe or dispense drugs?
Você é um profissional de saúde habilitado a prescrever ou dispensar medicamentos