Pre-surgical orthopedics is a treatment that modifies the position of fissured maxillary segments. In children with Bilateral Cleft Lip and Palate (BCLP); the collapse of the maxillary segments and protrusion of the premaxilla imply that during the surgical procedure there may be an excessive tension and make cheilopasty difficult. A modification of the Latham’s Device (MLD) was performed to correct the position of the premaxilla and the palatal processes. The study was conducted with photographs and dental casts of 14 BCLP patients, 0 to 12 months old with a protruding premaxilla of more than10mm. On a lateral view, the average reduction was 19.75mm; in an occlusal view, the left side was reduced 15.15mm and on the right side 13.87mm. A significant protrusion decrease was achieved.
La ortopedia prequirúrgica es el tratamiento que modifica la posición de los segmentos maxilares fisurados. En niños con labio y paladar hendido bilateral (LPHB) el colapso de los segmentos maxilares y la protrusión premaxilar implican una excesiva tensión y dificulta la queiloplastia. Se realizó una modificación al aparato de Latham para corregir la posición de la premaxila y los procesos palatinos. El estudio se hizo en registros fotográficos y modelos de estudio de 14 pacientes de 0 a 12 meses con LPHB con premaxilas protruidas de más de 10mm. La reducción en promedio de la distancia en una vista lateral fue de 19.75mm. En un vista oclusal del lado Izquierdo fue de 15.15mm y del lado derecho de 13.87mm, se logró una disminución significativa de la protrusión.
Abramovich, in 19971 explained that the neural crest cells of the cranial and vagal area generate the ectomesenquima of the skull-cervical-facial region and the pharyngeal arches, from which the facial processes derive. Cell migration and multiplication result in the formation of the facial process. The branchial or pharyngeal arches arise in the fourth and fifth week of intrauterine development. In an initial period these are constituted by mesenchymal tissue, separated by grooves called pharyngeal clefts. The pharyngeal arches contribute not only to neck formation, but also play an important role in face development, mainly the first and second arch.
The face is formed between the fourth and eighth week of the embryonic period through the development of five facial processes: The cephalic or frontonasal process constitutes the upper edge of the stomodeum or primitive mouth; the maxillary processes that can be seen lateral to the stomodeum, and in a caudal position from the latter, the mandibular processes (both processes derive from the first branchial arch).
In the sixth and seventh week of intrauterine life the maxillary processes grow simultaneously in a medial direction, compressing the nasal processes toward the midline. In a later stage the cleft located between the internal nasal process and the maxillary process is covered and they both merge. Consequently, the upper lip is formed by the internal nasal and the maxillary processes.1
EpidemiologyFacial and oral clefts may occur between the fifth and seventh week of intrauterine life.1
Armendares and Lisker2 determined a cleft lip and palate (CLP) incidence of 1.39 out of 1,000 newborns in Mexico. Each day, there are 9.6 new cases which represent 3521 cases per year and are considered as the CLP national annual incidence.3
Oral clefts are associated with multiple genetic and environmental factors: they may be part of a syndrome, for example: Van der Woude, Apert, Pierre Robin, etc. and/or be associated with drugs, teratogenic agents or medical conditions. In isolated clefts, etiology is more difficult to determine. Current concepts suggest folic acid deficiency as an active predisposing factor.4
Given its complexity, this anomaly requires a multi- and interdisciplinary team for its management.
Pre-surgical orthopedics is the procedure in which the position of the cleft maxillary segments and the premaxilla is managed prior to the lip and palate reconstruction. Its main objective is to reduce cleft width, re-establish an adequate anatomical relationship and decrease tension between maxillary segments. It is recommended for children with 10 or moremm clefts.
Presurgical orthopedics in CLP patients was first performed in 1791 by Desault who described and used a cap that applied an extraoral force on the premaxilla.5 In 1956, in England, McNeal6 used dentofacial orthopedics to align the maxillary segments in unilateral CLP and to bring the pre maxilla towards the midline in bilateral CLP. In 1960 Burston7 suggested managing the segments before lip closure in newborns.
Ortiz Monasterio8 in 1966 demonstrated in his study that CLP adult patients who were not surgically treated, did not exhibit midface growth restriction.
Moss9 in 1972 developed the functional matrix theory where he states that craniofacial growth and development are determined by different structures, soft tissues among them.
In 1972, Friede and Pruzansky10,11 were not in favor of orthopedic-surgical treatment. They claimed that there was growth restriction that caused concave profiles due to maxillary retrusion and supported the idea that it was best to re-establish the continuity of labial musculature early after birth to allow natural muscular forces that mold the palate to normalize the distorted oral and pharyngeal skeletal architecture.
Georgiade and Latham12,13 in the 70’s decade performed intraoral traction appliances anchored to the segments by chains.
In 1977 Millard, Robertson and Shaw14,15 examined the efficacy of pre-surgical orthopedic treatment and reported favorable results.
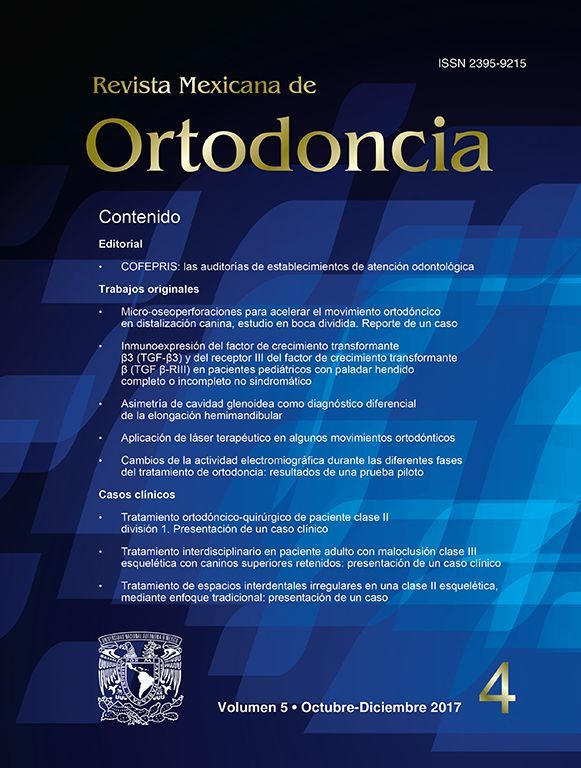
Millard and Latham16 in the 90’s decade performed premaxillary retrusion and expansion of the maxillary processes by means of a device with 4 intermaxillary pins, one pin of transmaxillary anchorage and an expansion mechanism in the palatal processes activated through elastomeric chains (Figure 1 and 2). Shaw17 in 1992 stated that presurgical orthopedics does not increase maxillary growth and that its benefits are limited.
In 2004 Berkowitz18 described the long-term consequences of the Latham’s orthopedic device which would not produce a harmonious development of the face and palate. However in 2004 Pérez19 et al reported favorable results with the use of Latham’s device in 14 patients through photographic and cephalometric records of 11mm expansion of the maxillary process and 18mm retrusion in the transverse dimension.
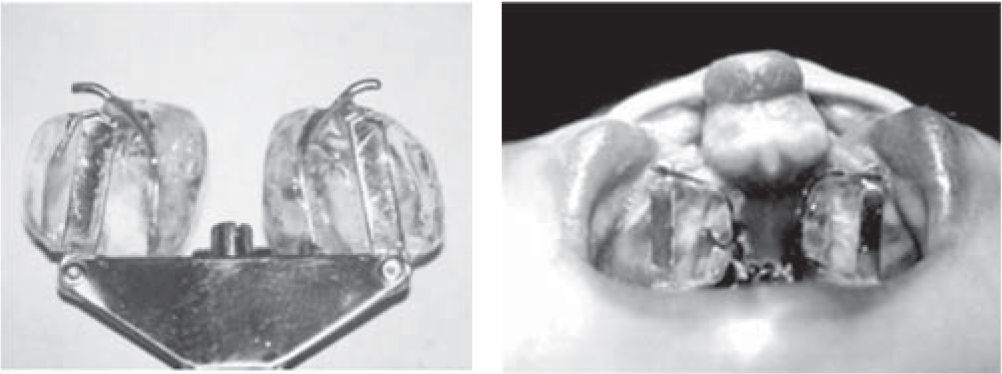
A modification of the Latham’s device was made at the Stomatology-Orthodotnics Division where the Latham screw was replaced with an 8mm expansion screw and two buttons in the anterior portion of the device. It was called Modified Latham’s Device (MLD) (Figure 3).
Definition of the problemDoes the use of MLD in patients with CLP modify favorably the transverse and anteroposterior relations of the premaxilla and the lateral processes of the maxilla in order to carry out the cheiloplasty?
RationaleIn patients with excessive CLP the transverse and antero-posterior discrepancies between the processes make chieloplasty difficult. The Latham appliance has been used to align the three segments in a favorable manner16 but its cost exceeds $7,000 which makes it less accessible. A modification was designed at the Division of Stomatology- Orthodontics with the same principles as the original Latham device but at an affordable cost for the hospital’s patients.
If the functionality of this appliance allows us to obtain favorable conditions for bringing the maxillary processes to a suitable position, this type of treatment will be accessible and beneficial for our patients.
HypothesisThe use of the modified Latham device by the Division of Stomatology and Orthodontics for presurgical orthopedics in patients with CLP modifies favorably the transverse and antero-posterior relationship of the premaxilla and maxillary processes.
General objectiveTo determine the functionality of the modified Latham device by the Division of Stomatology-Orthodontics for presurgical orthopedics.
Specific objectives- •
Quantify the premaxilla retraction in photos and study models of patients with CLP after the use of the MLD.
- •
Assess the expansion of the maxillary processes in study models of patients with CLP after the use of the MLD.
- •
Quantify the rotation and deflection of the premaxilla in study models of patients with CLP after the use of the MLD.
Observational, comparative, open, retrospective and longitudinal research.
Material and methodsStudy universeAll the complete files of syndromic and non-syndromic CLP patients, with more than 10mm premaxillary protrusion, less than one year of age, who were treated with the modified Latham appliance at the Plastic and Reconstructive Surgery Division and at the Stomatology-Orthodontics Division in the period from 2005 to 2008.
SampleData was obtained by means of pre- and postoperative records: plaster models, intraoral and extraoral photographs from files of the Stomatology-Orthodontics Division of patients treated with the MLD. The files from patients who abandoned or discontinued treatment were excluded and the records that had that could not be assessed were eliminated. The total number of files that met all the criteria was 14.
VariablesThe studied variables were:
- •
Premaxilla protrusion lateral view (photographs)
- •
Premaxilla protrusion left occlusal view (models)
- •
Premaxilla protrusion right occlusal view (models)
- •
Anterior cleft size (transverse) (models)
- •
Posterior cleft size (transverse)(models)
- •
Transverse width of the premaxilla
- •
Degree of rotation of the premaxilla
- •
Degree of deflexion of the premaxilla
All the variables in the study were measured by one operator with an electronic calibrated protractor and a vernier. The results were transferred to data capture sheets.
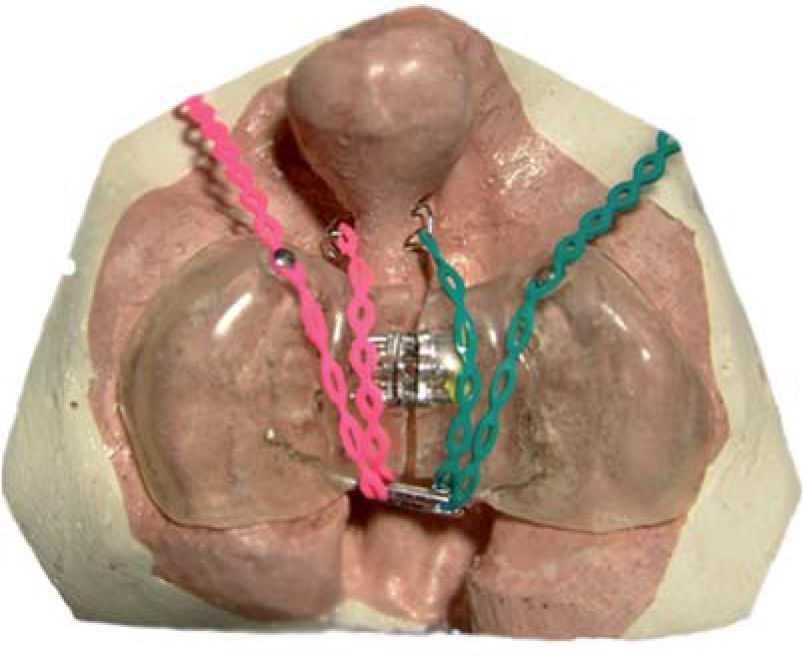
In the pre and post-treatment with the Latham appliance extraoral lateral photographs the distance from the most posterior point of the nasogenian cleft at the alar insertion level to the most anterior of the premaxilla was measured to determine the amount of retraction.
In the pre and post-treatment models, the distance from the most upper and lateral point of the premaxilla external ridge to the most upper and anterior point of the left and right alveolar ridges was measured. The cleft size was measured at the anterior and at the posterior portion of the model, as well as the transverse width of the premaxilla. The angle formed by the midline between the two maxillary and a line at the center of the premaxilla was taken into consideration to determine the degree of rotation. The degree of deflexion was measured from the distance between the most superior ridge of the maxillary processes to the most superior point of the pre and post-treatment premaxilla (Figure 4).
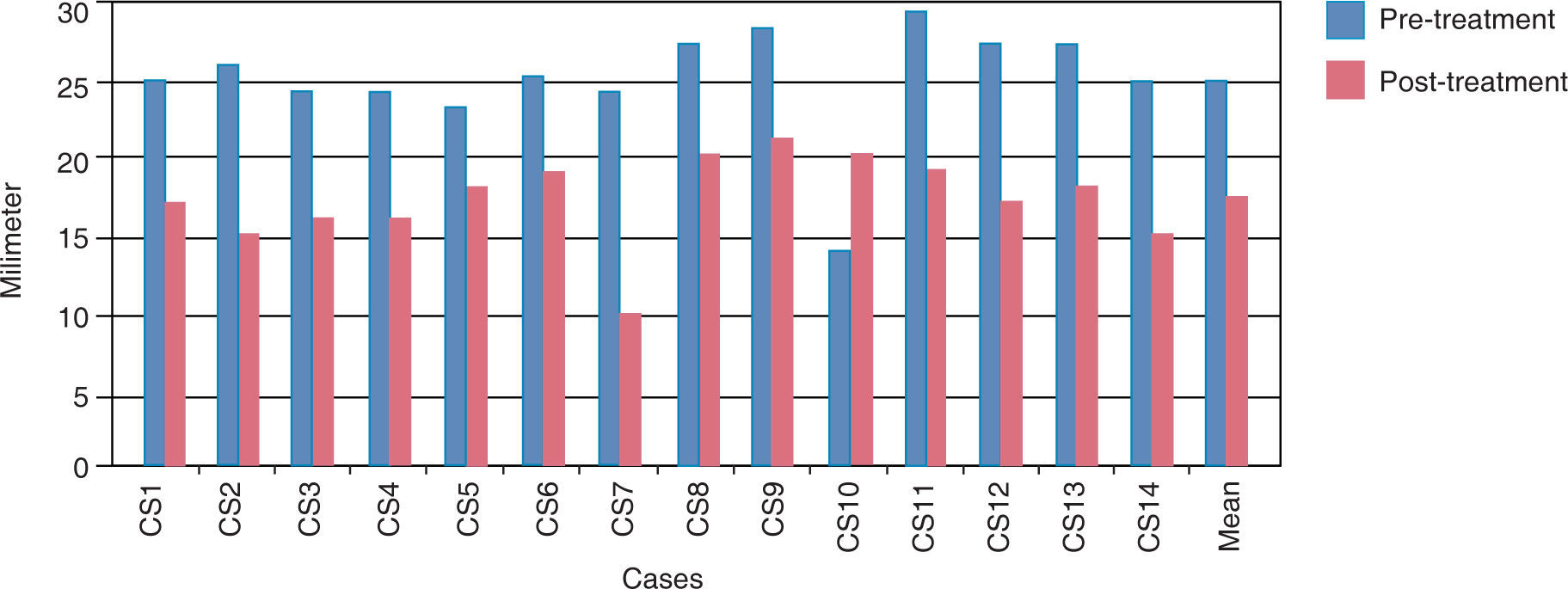
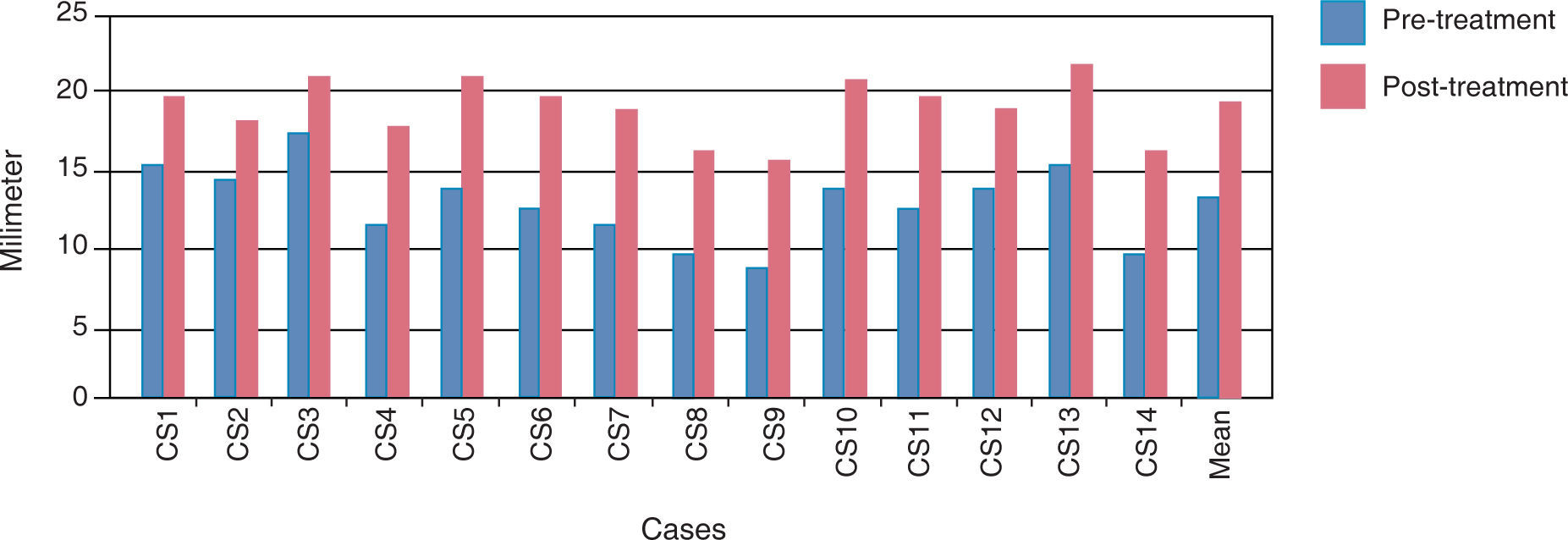
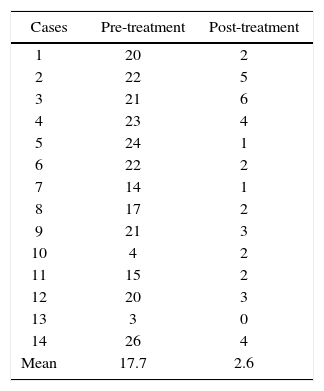
ResultsIn the mean results of the lateral photographs’ measurements a 7.64mm sagittal retroposition of the premaxilla was observed (Table I) (Figure 5).
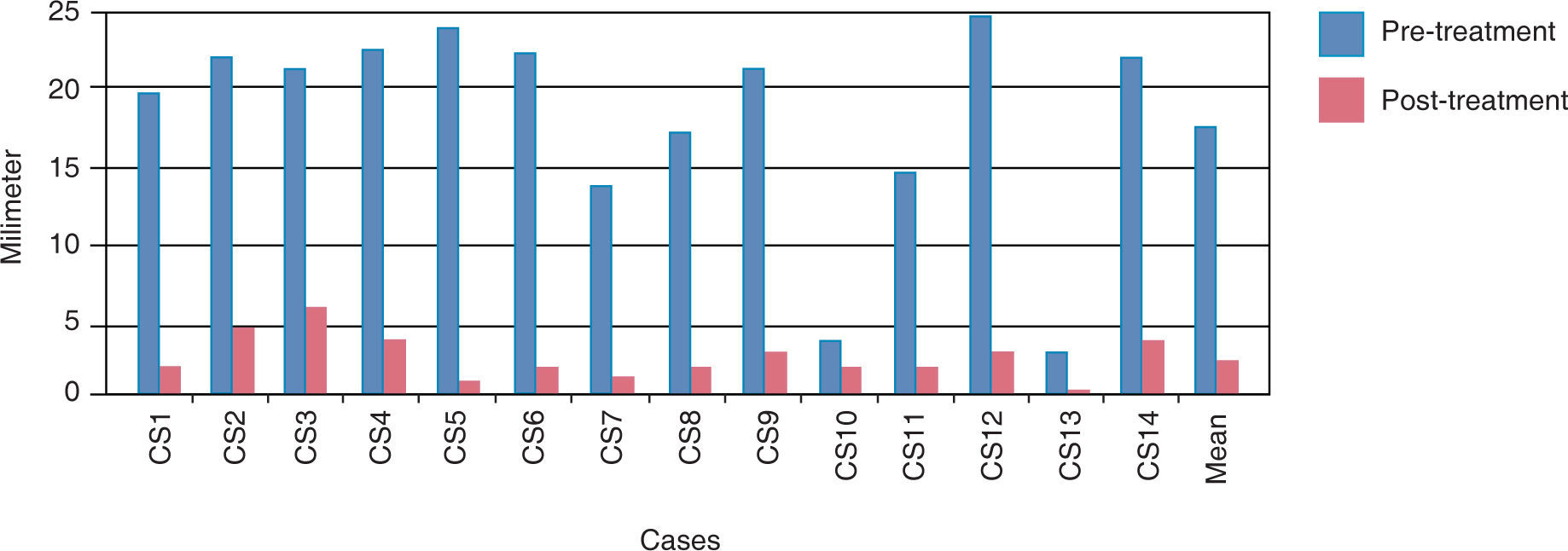
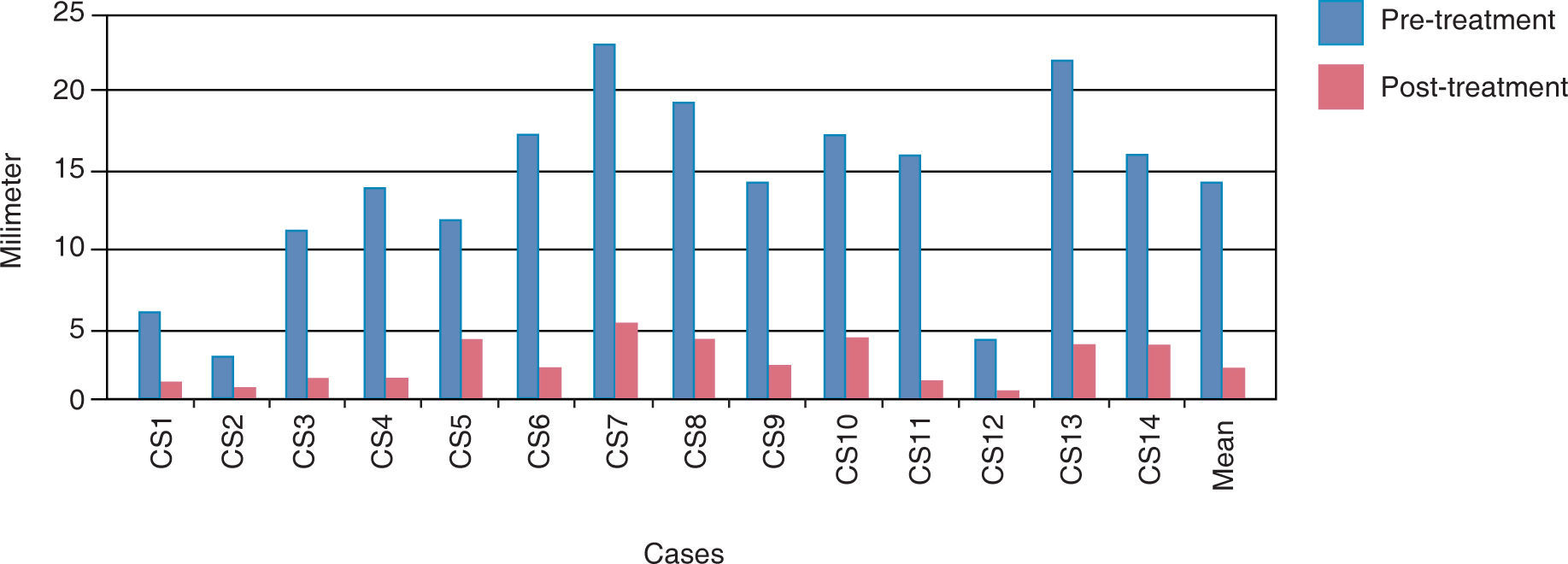
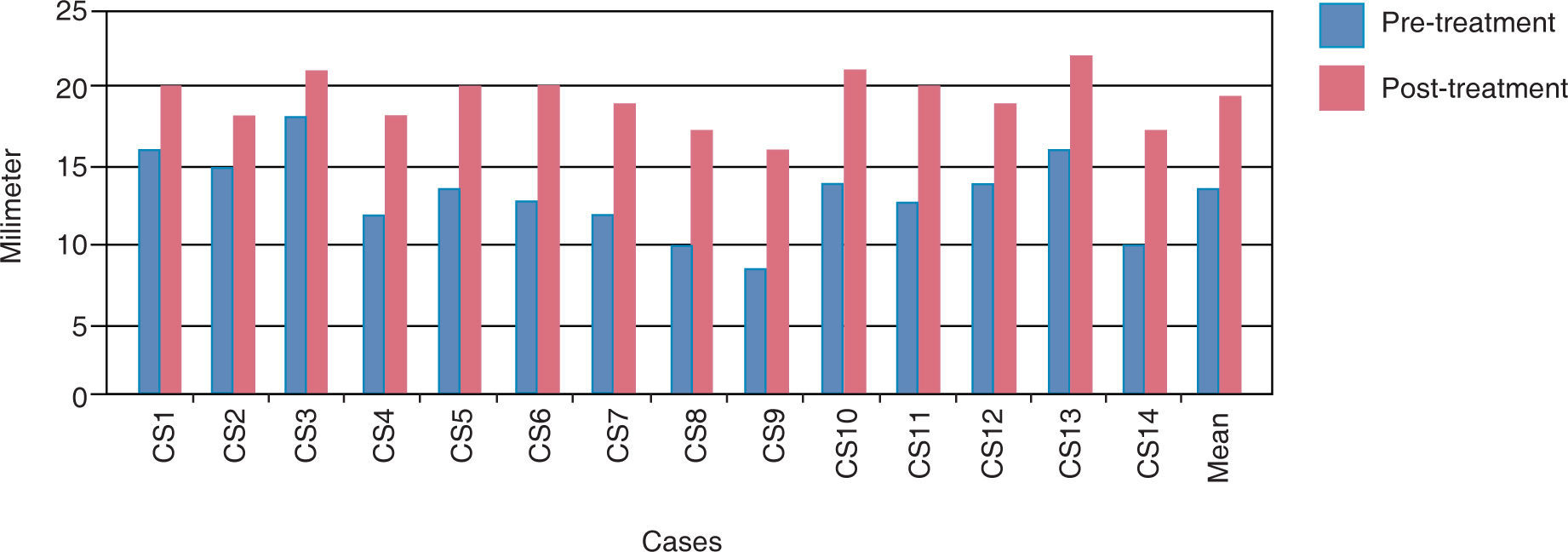
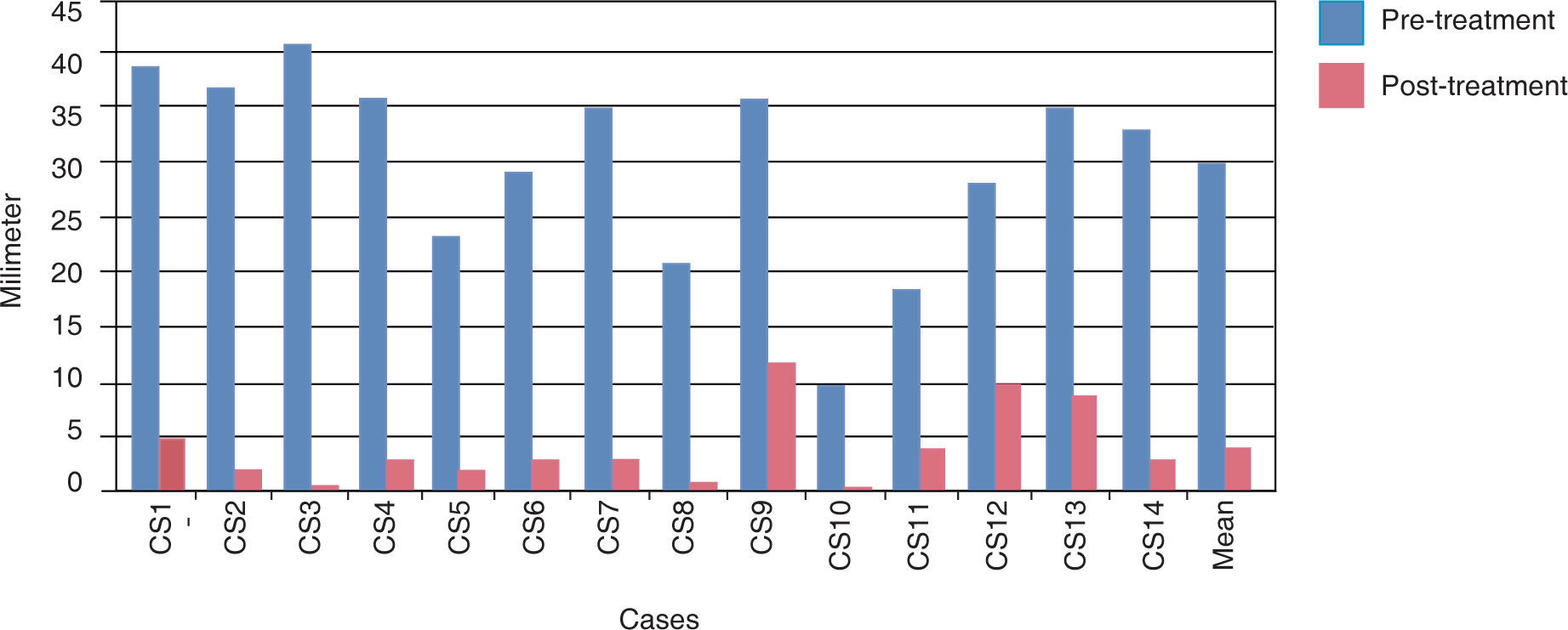
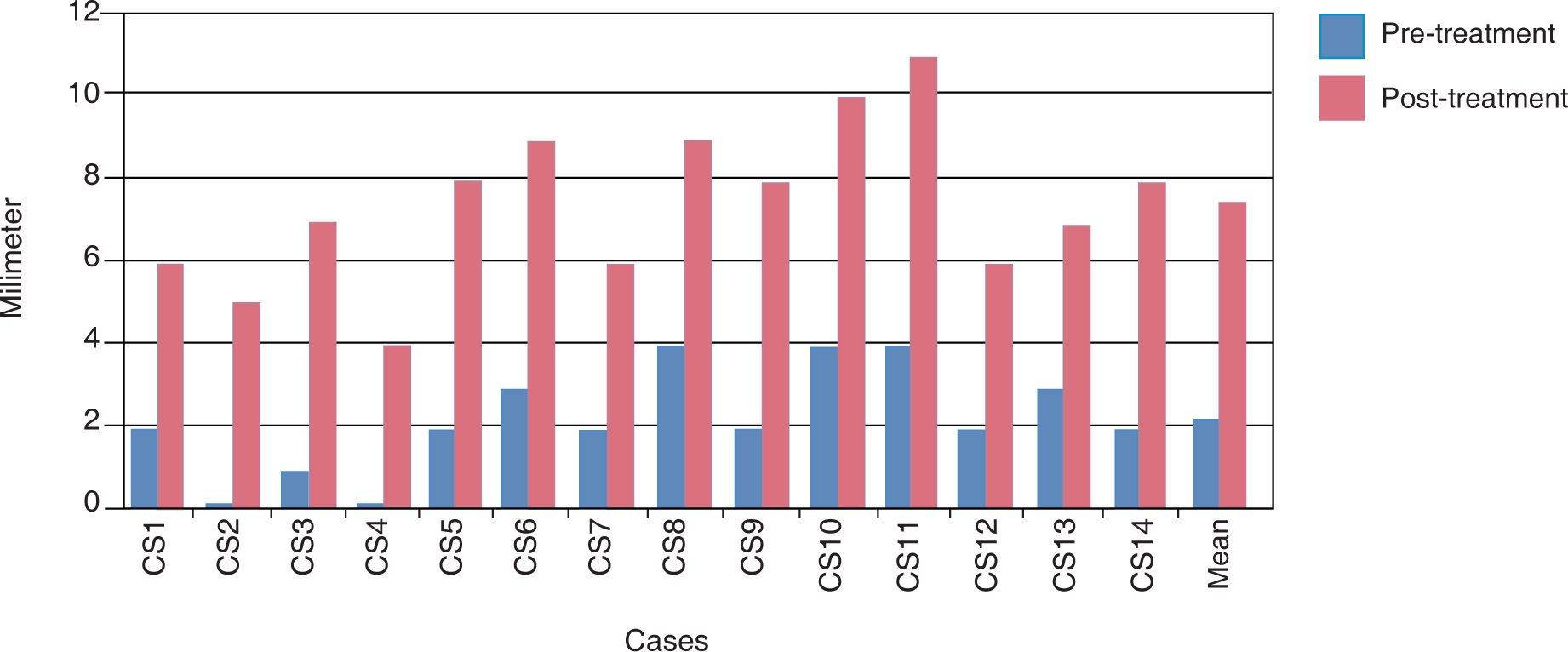
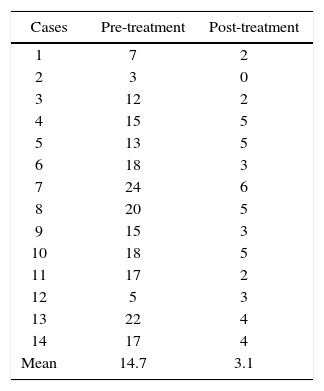
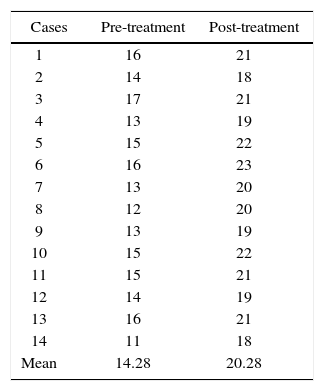
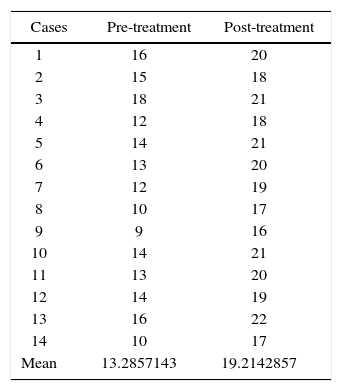
In the anteroposterior study, model measurement a 15.1mm reduction on the right side and an 11.6 decrease on the left side was obtained (Tables IIandIII) (Figures 6and7). In the anterior portion of the palatal cleft the mean measurements were 14.2mm at the beginning of treatment and 20.2mm at the end. The amount of expansion was 6mm (Tables IVandV) (Figures 8and9).
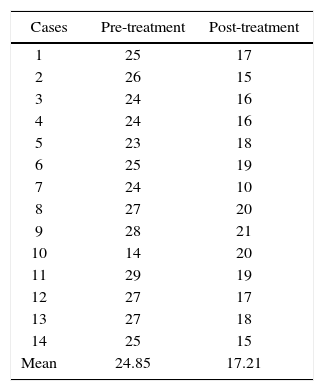
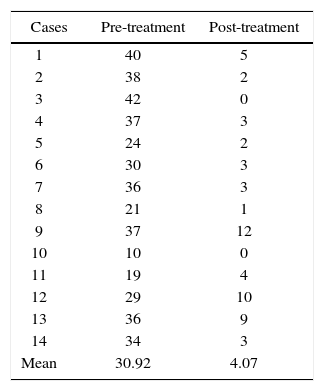
The premaxilla rotationwas measured in degrees in relation to the midline between the two maxillary segments. The initial mean was 30.92° and after treatment it was 4.97°, a favorable alignment of the maxilla was achieved (Table VI) (Figure 10).
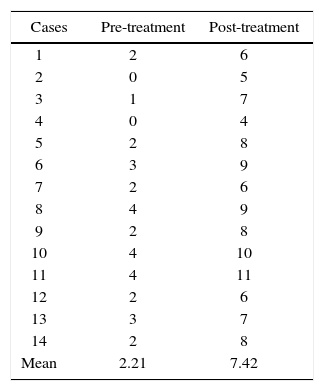
The pre-treatment degree of premaxilla deflection was a mean of 2.21mm and after treatment it was 7.42mm thus producing a 5.21mm deflection and an unfavorable surgical prognosis (Table VII) (Figure 11).
The anatomical alignment and the tension decrease in the soft tissues that Latham and Perez et al. achieved in the 90’s is significant when compared to the results obtained with other pre-surgical orthopedic devices.
With the use of the modified Latham appliance statistically significant results were achieved, similar to the ones obtained with the Latham appliance, such as premaxilla retroposition, expansion of the maxillary segments and premaxilla alignment. This provides a low-cost alternative for orthopedic treatment since the patients that attend the General Hospital «Dr. Manuel Gea González» are a low-income population.
ConclusionsWith the use and activation of the Modified Latham Appliance, the premaxilla distance was reduced in the sagittal plane and in the transverse plane, it was aligned. The maxillary segments were expanded and formed in a period of 3 months. In this study, clinically significant favorable results were obtained in the management of patients with BCLP. With a tridimensional positive handling of the premaxilla and the palatal segments by means of the Latham Modified Appliance, the cheiloplasties in all 14 patients could be performed.
In the pos-treatment assessment of the patients on the medium and long term we may be able to observe the degree of scarring bridle restriction on the tissues, assess the clinician’s expertise and the effectiveness of the studied appliance. The orthopedic-surgical treatment follow-up may also be determined and modify and create new alternatives for the treatment of these patients.