Osteomas are benign osteogenic lesions characterized by compact and/or cancellous bone proliferation. The aetiology of these lesions remains unknown. It is usually asymptomatic and it is often detected incidentally on routine radiographic examination or until it causes facial asymmetry or dysfunction. It is characterized by very slow and continuous growth. The peripheral osteoma of the jaw is uncommon. Radiographically, peripheral osteomas are seen as oval radiopaque well-circumscribed masses attached to the cortex by a broad base or a pedicle. Three theories have been proposed: developmental, neoplasic and reactive. The possibility that peripheral osteomas may be a reaction to trauma could explain the occurrence on the lower border and buccal aspect of the mandible. The objective of this article is to present the radiographic features of two cases of osteomas, one in the lingual site of the mandibular angle and another one on the zygomatic arch.
Osteomas são lesões osteogénicas benignas caracterizadas pela proliferação de osso compacto e/ou esponjoso. A etiologia destas lesões permanece desconhecida. Geralmente é assintomática e muitas vezes é detectada acidentalmente no exame radiográfico de rotina ou quando há assimetria facial ou disfunção. É caracterizada por um crescimento lento e contínuo. O osteoma periférico da mandíbula é raro. Radiograficamente, osteomas periféricos são vistos como uma imagem radiopaca oval, bem circunscrita ligada ao córtex por uma base ampla ou pedículo. Três teorias têm sido propostas: desenvolvimento, neoplásica e reativa. A possibilidade dos osteomas periféricos poderem ser uma reacção ao trauma poderia explicar a ocorrência no bordo inferior e face lingual da mandíbula. O objetivo deste artigo é apresentar as características radiográficas de dois casos de osteomas, um na face lingual do ângulo mandibular e outro no arco zigomático.
Osteomas are benign, osteogenic lesions that may arise from proliferation of cancellous (trabeculae), compact bone (dense lamellae) or can be composed by a combination of both.1–8 There are three different types of osteomas: central, peripheral and extra-skeletal.7,9 Osteomas are more commonly found in the cortical plate of long bones but they can also affect the maxillofacial region. It is usually asymptomatic, and exhibit continuous growth at adulthood but it can grow into large sizes and cause facial asymmetry or severe dysfunction.1,5,8,10 In these cases, surgery is usually required. Since osteoma is often detected incidentally on routine radiographic examination, the dentist should be aware of the features of this lesion. Osteomas can cause facial deformity, limitation or deviation of the mandible on opening, headache, bone pain, dysphagia or exophthalmos.7,11
The objective of this article is to present the radiographic features of two cases of osteomas, one in the lingual site of the mandibular angle and another one on the zygomatic arch.
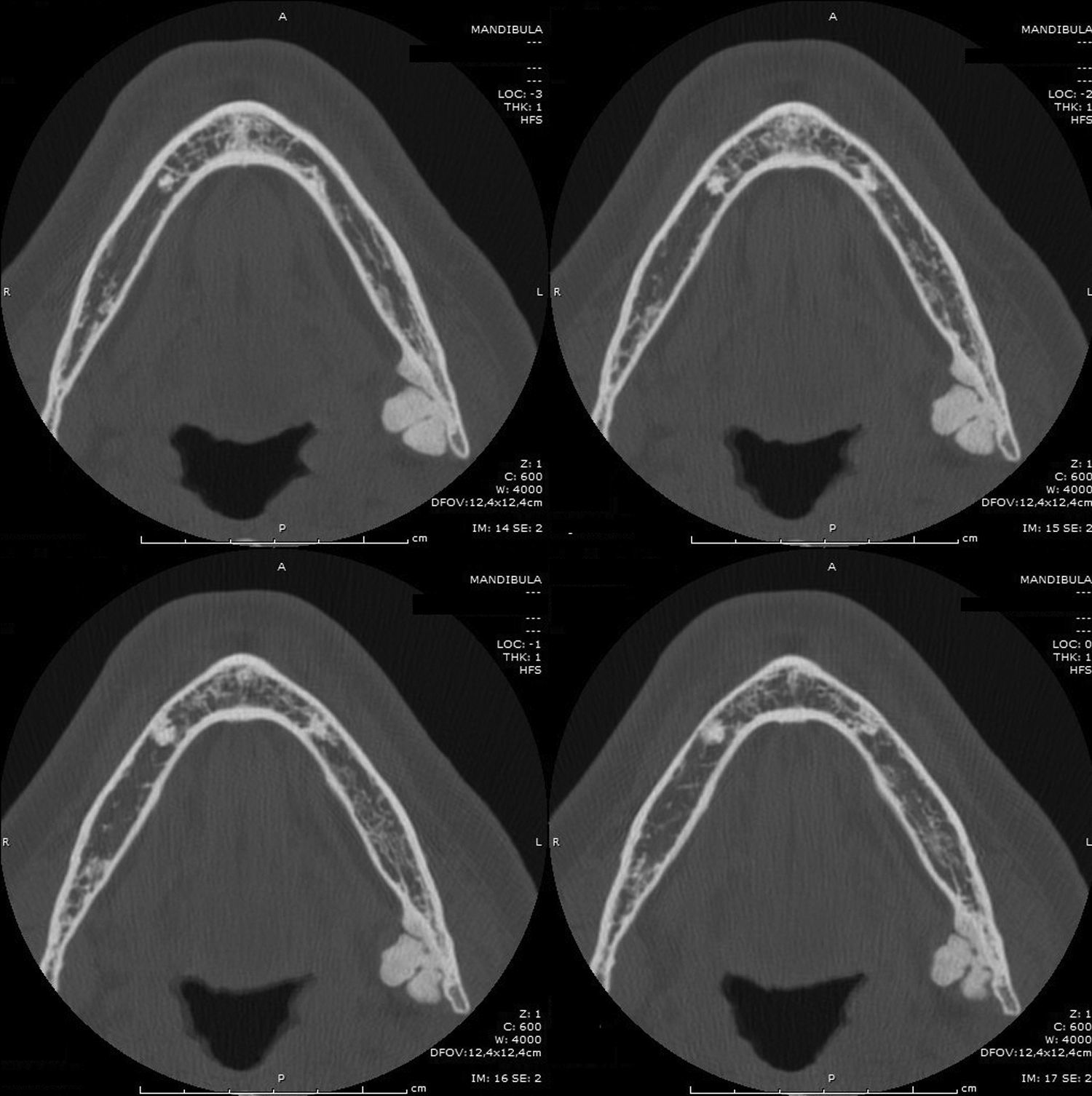
Case reportsCase 1A 57-year-old male patient was referred to the Department of Oral Radiology for evaluation of a radiopaque mass located on the left side of the mandible. The lesion was found incidentally in a dental panoramic tomography during routine evaluation for dental treatment (Fig. 1). The patient was completely asymptomatic with no history of previous facial trauma or contributory medical factors. The panoramic radiograph demonstrated a unilateral, well-circumscribed, mushroom-like radiopacity located at the left angle of the mandible.
A Computed Tomography was performed with a HiSpeed NX-I Dual Slice (General Electrics Dentascan, General Electrics Healthcare, United Kingdom; Dentascan). Axial slices of 1.0mm thick with an interval of 1.0mm were obtained and these images were further reformatted using the software DentaScan to achieve cross-sectional images (Fig. 2). The axial and cross-sectional images revealed a pedunculated, well-defined and lobulated mass involving the right lingual border of the mandible, measuring 16.94mm (height) and 12.14mm (width) and with a density similar to bone tissue (UH=1425). Since the lesion did not interfere with normal function and had no cosmetic problem, the lesion was not treated, and the patient was kept under observation.
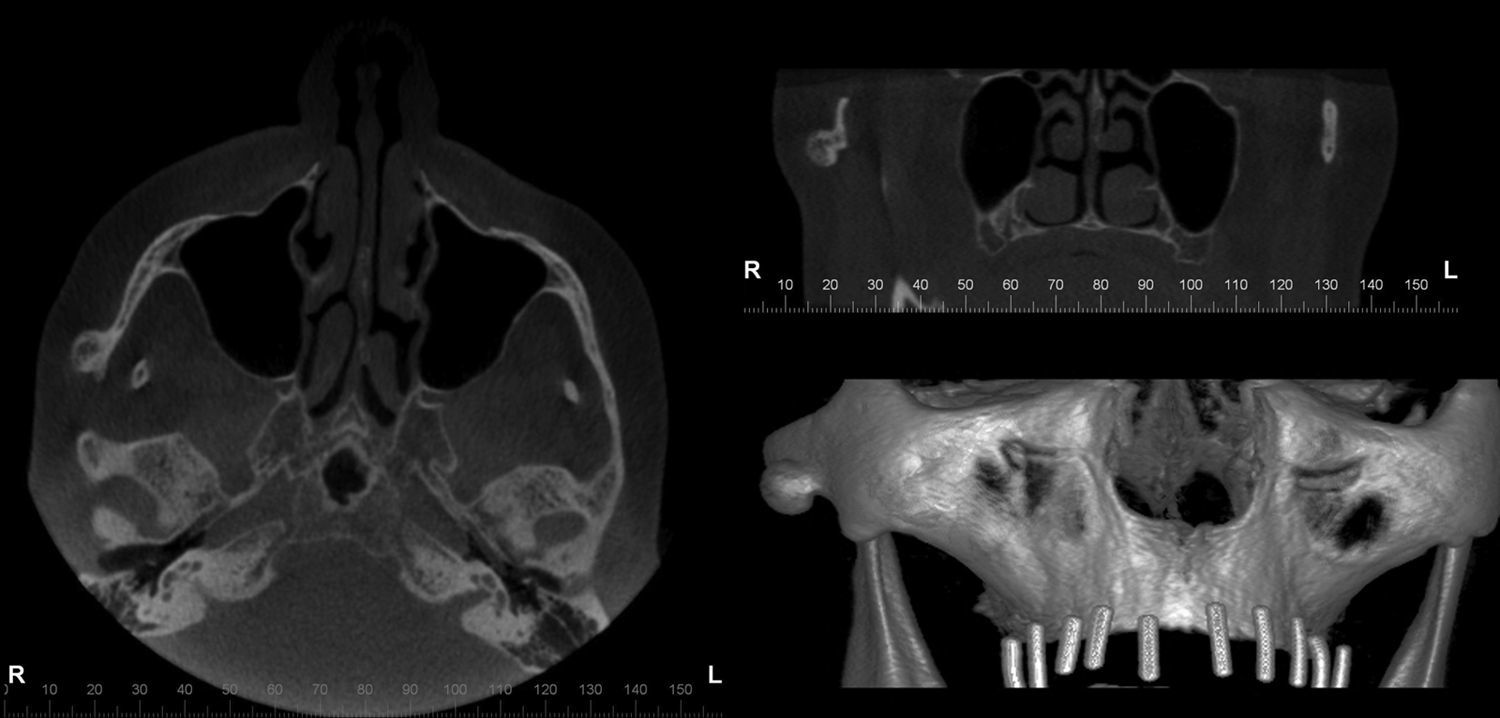
Case 2A 61-year-old woman was referred to perform a Cone Beam Computed Tomography (CBCT) evaluation for implant planning in the maxilla. The patient was asymptomatic and the lesion was found incidentally. She could open her mouth without any mechanical interference, did not complain of pain or other symptoms and had no history of previous facial trauma or additional medical factors. CBCT was performed with an i-CAT Vision® (Imaging Sciences Int. Hatfield, Pennsylvania, USA) and revealed a bonelike, extensive, pedunculated osseous lesion, in the anterior region of the right zygomatic arch, measuring 8.5mm (height)×6.7mm (width)×9.85mm (length) (Fig. 3).
Given that the patient was asymptomatic, treatment was not required. The patient was kept under observation.
Discussion and conclusionOsteomas are benign, osteogenic lesions that may arise from proliferation of cancellous (trabeculae), compact bone (dense lamellae) or can be composed by a combination of both.1,2 There are three different types of osteomas: central, peripheral and extra-skeletal.12 Central osteomas arise from the endosteum, peripheral osteomas from the periosteum and extra-skeletal osteomas usually develops within a muscle.4,8,9,11,13
Osteomas can occur at any age, but are found most frequently in individuals older than 40 years.5 There are reports of cases varying from 16 to 74 years of age, with a mean age between 10 and 25 years. Osteomas in the maxillofacial region have been reported in patients between 29.4 and 40.5 years.7 They are more frequent in males than females (approximately 2:1).1,3,8
Osteomas are more commonly found in the cortical plate of long bones such as the femur and the tibia. In the maxillofacial region, osteomas occur most frequently in the sinuses. The most common site is the frontal sinus, followed by ethmoidal and maxillary sinuses.5 Other documented locations include the external auditory canal, orbit, temporal bone and the pterygoid plates and, rarely, in or on the jaws. However, when it affects the jaws, the mandibular angle and the inferior border of the body are more commonly involved in association with the buccal plate.8,9,14 The involvement of the lingual surface of the mandible, such as in this present case, is uncommon.3,5,9,15,16
In the literature, case reports publishing osteomas in the mandible include 23 cases located in the body (4 cases in the anterior region and 19 cases in the posterior region) followed by the condyle (18 cases), angle (9 cases), ascending ramus (7 cases), coronoid process (5 cases) and sigmoid notch (1 case).2,11,17 In current literature, there is only one case reported of osteoma in the zygomatic arch by Furnaleto et al.18
Peripheral osteoma of the jaw is an osteogenic benign lesion of slow growth, which can be or not pedunculated.12,19 As in the present cases, peripheral osteoma are normally an incidental finding since they are asymptomatic, but other times depending on the location and the size of the lesion, it can cause facial deformity, deviation of the mandible on opening, headache, bone pain, dysphagia or exophthalmos.3,5,7,15,16,20,21
The most common symptom when present is pain.6
Conventional radiological examinations (dental panoramic tomography and Water’ s view) are generally sufficient to diagnose an osteoma. Radiographically, it appears as a unilateral, pedunculated, well-defined, oval or round mushroom-like radiopaque mass with similar density to normal bone.1,5,7,16 A dental panoramic radiography usually shows the position and benign nature of the lesion. The use of Computed Tomography (CT) results in better resolution and more precise localization, being the more accurate method for diagnosis and surgical planning.5,9,15
The differential diagnosis should include osteochondroma, fibrous dyplasia, chondroma, ossifying fibroma, condensing osteitis, exostoses including tori, which are bony excrescences that occur on the buccal aspect of the alveolar bone. Bony exostoses (except tori) tend to appear on the buccal/facial aspects of the alveolar bone in contrast to peripheral osteomas, which almost always occur on the lingual/palatal aspects of the alveolar bone. Focal sclerosing osteomyelitis, osteosarcoma, peripheral ossifying fibroma, chondroma, Paget's disease, monostotic fibrous dysplasia, calcified meningioma and odontoma should also be considered in the differential diagnosis.1,6–9,11,12,22,23 These lesions are of reactive or developmental origin and are not thought to be true neoplasms. Osteoblastomas and osteoid osteoma are, usually, more painful and have a greater growth rate than osteomas.
In the present cases, the radiological appearance with the clinical aspects such as absence of symptoms, slow growth rate and the location of the lesion are compatible with peripheral osteoma.11,14 Usually the radiological appearance are characteristic; however a conclusive diagnosis is determined by histological microscopic examination.
The pathogenesis of the osteoma is unknown. Some investigators consider osteoma a true neoplasm, and others classify it as a developmental anomaly. The possibility that peripheral osteomas may be a reactive mechanism, triggered by trauma or infection, has also been suggested.7 Most peripheral osteomas are on the lower border or buccal aspect of the mandible, and these sites are more susceptible to trauma than the lingual aspect and are in close proximity to muscle attachment.1,24 Even minor trauma may cause subperiosteal edema or bleeding, and the muscle traction could locally elevate the periosteum. This could initiate an osteogenic reaction that might be preserved by continuous muscle traction. Nevertheless, osteomas on the lingual aspect cannot be explained by this theory.
There are no reports of malignant transformation of peripheral osteoma.9,20 The removal of peripheral osteomas generally is not necessary. Instead, routine clinical and radiographic follow-up should be performed considering that most of the tumours are asymptomatic.1,24 In 15 cases of peripheral osteoma, follow-ups were reported from 6 months to 9 years. Bosshardt et al. (1971) described a case of recurrence 9 years after the surgery, which may indicate the need for prolonged periodical clinical and radiographic follow-up after surgery.9
In the literature we could find references of absence of recurrence after 5 years.3,7 Surgery is indicated when there are symptoms, deformity or if the lesion presents active growth.9,14,19 Recurrence is extremely rare. In these patients, surgery was not performed.
The presence of osteomas may be a sign of the presence of Gardner's syndrome, which is characterized by a triad of colorectal polyposis, skeletal abnormalities (with multiple osteomas of the skull and face) and multiple impacted supernumerary teeth.11,23 Since the osteomas develop before the colorectal polyposis, early recognition of the syndrome is very important to the prognosis of the disease.1,7
General Dental Practitioners may identify regularly impacted teeth and when they are associated with osteomas of the jaw, they should be aware of the triad of the Gardner's syndrome.
In conclusion, the identification of the radiographic features is essential to diagnose the osteoma, since its radiographic appearance is characteristic and should be kept in mind in order to do the diagnosis. Although its aetiology remains unknown, we could suggest developmental aetiology for the present cases, as no previous history of trauma or medical factors were referred. Since osteomas, can cause facial deformity, limitation or deviation of the mandible on opening, headache, bone pain, dysphagia or exophthalmos, the clinician should look for these findings while examining the patient.3,7 Periodical clinical and radiographic follow-ups were performed in both patients and this is advised in similar cases.
Ethical disclosuresProtection of human and animal subjects: The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of data: The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent: The authors must have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence must be in possession of this document.
The authors have no conflicts of interest to declare.