The main objective of this study was to analyse the cocaine addict subgroup from the Madrid study of prevalence of dual disorders in community mental health and substance misuse services.
MethodsThe sample consisted of 837 outpatients from Madrid, Spain. We compared 488 subjects who had a lifetime diagnosis of cocaine abuse or dependence, and 222 subjects who did not have a cocaine substance use disorder. We used the Mini International Neuropsychiatric Interview to evaluate Axis i mental disorders, and the Personality Disorder Questionnaire to evaluate personality disorders.
ResultsAlmost three-quarters (73.4%) of cocaine addicts had a current dual disorder. Most prevalent were mood and anxiety disorders. Almost half (49.6%) had a personality disorder. Most of them (94.9%) had other substance use disorders. Cocaine addicts did not have higher prevalence rates of dual pathology than addicts with no cocaine abuse or dependence. Cocaine addicts were associated to a diagnosis of antisocial personality disorder, agoraphobia, and post-traumatic stress disorder, and they had an early age of onset of alcohol and cannabis use.
ConclusionsDual pathology is not higher in cocaine addicts in treatment than in addicts who do not use cocaine, however cocaine addicts started other drugs earlier, and were associated with specific mental disorders.
El objetivo de este estudio es analizar el subgrupo de adictos (criterios de abuso o dependencia) a la cocaína procedentes del estudio Madrid sobre prevalencia de diagnóstico dual en varios dispositivos asistenciales.
Material y métodosLa muestra está constituida por 837 sujetos en tratamiento en la red de salud mental o en la red de drogas de la Comunidad de Madrid, de los cuáles 488 tenían un diagnóstico de abuso o dependencia de cocaína a lo largo de la vida y 222 tenían otros trastornos por uso de sustancias distintos de la cocaína. Se uso la entrevista MINI (Mini Internacional Neuropsychiatric Interview) para el diagnóstico de los trastornos mentales del eje I y el cuestionario PDQ (Personality Disorder Questionnaire) para la valoración de los trastornos de personalidad.
ResultadosSe consideró que un 73.4% de los adictos a la cocaína tenían un diagnóstico dual en el momento actual, destacando la prevalencia de los trastornos del estado de ánimo y de ansiedad. El 49.6% de los adictos a la cocaína tenían un diagnóstico de trastorno de la personalidad. Un 94.9% de estos adictos a la cocaína tenían otros diagnósticos asociados de trastornos por uso de sustancias. El subgrupo de adictos a la cocaína no tenía mayor prevalencia de diagnóstico dual que el resto de los adictos. El subgrupo de adictos con abuso o dependencia de cocaína tenían mayor prevalencia de trastorno antisocial de la personalidad, agorafobia y trastorno por estrés postraumático que los adictos no consumidores de cocaína y habían iniciado de forma más precoz el consumo de alcohol y cannabis.
ConclusionesLa presencia de diagnóstico dual no es más elevada en adictos a la cocaína en tratamiento que en otros adictos, aunque han iniciado más precozmente otros consumos y se asocia más que el resto de adictos a ciertos trastornos mentales específicos.
Dual diagnosis is defined as the presence of a substance use disorder (SUD) and a mental disorder in an individual, within a specific period.1 Such comorbidity is normal, as indicated in important epidemiological studies in the general population,2,3 and likewise in clinical samples.4 Comorbidity is associated with greater used of health services, distinct phenotypes, increased severity of the condition, greater functional disability and worse progression.4,5
We have little data on the prevalence of dual diagnosis in a Spanish population and on its distribution among the 2 main healthcare networks that provide aid, the drug network and that of mental health. Knowledge about the distribution of dual diagnosis and the characteristics of these subjects can help to optimise health resources.
Cocaine use is associated with a wide variety of mental disorders. Multiple studies in the general and clinical populations indicate this.3,4,6–17 The most prevalent mental disorders are depressive, anxiety and personality disorders.11,16,17
In a pilot study on the prevalence of dual diagnosis carried out by the Spanish Society of Dual Pathology (SEPD in Spanish), an association was seen between alcohol dependence and the presence of other Axis i mental disorders, especially with mood disorders, and between cocaine dependence and personality disorders.18 This pilot study served to design the study on the prevalence of dual diagnosis with a wider sample. The main objective was to quantify the prevalence of the various types of affectations included within the “dual diagnosis” complex (mental disorder and substance use disorder) in the 2 networks involved in Madrid. The design and some overall results of the study have been published before.19 In this article we present the data concerning patients with criteria of abuse or dependence on cocaine.
Materials and methodsSampleThe patients were selected consecutively by their own therapists in the drug treatment centres (CAID and CAD in Spanish: drug dependency care centres run by the Autonomous Community of Madrid and by the Madrid City Council, respectively) and in the mental health centres (MHC) in the Comunidad of Madrid. Consequently, we were able to include both first-time patients and follow-up patients. There were interviewers (psychiatrists, psychologists or general practitioners having extensive experience with addiction) at 64 drug treatment centres run by the Community of Madrid and at 17 MHC. All the interviewers received training in the administration of the structured interview. The participants signed an informed consent. The study was approved by the Committee for Ethical Research at the Hospital Gregorio Marañon in Madrid. The percentage of participation was 87.2%.
MethodsA data collection notebook was prepared to record the data from the pilot study mentioned previously on the most informative variables and those of greatest clinical interest for analysis. To establish the presence of mental disorders, the structured Mini International Neuropsychiatric Interview (MINI)20 was used. This instrument permits diagnoses based on DSM-IV and ICD-10 criteria (Sheehan and Lecrubier, version 5.0; Fernando L, Bobes J, Gubert J, Soto M, Soto O, 2000); it is an interview that makes it possible to explore the main current and lifetime Axis i psychiatric disorders. Clinical interviews were used to explore mental disorders that the MINI did not assess on a lifetime basis.
To establish the diagnosis of personality disorders, the PDQ4+ scale (Personality Disorder Questionnaire) (adapted to Spanish by Calvo et al.21) was used. This instrument combines the quickness and ease of use of a self-report questionnaire with the control of the effect of the symptoms of an interview. It is a good screening instrument at the clinical level, functioning as a good diagnostic tool according to o DSM-IV criteria when the clinical significance scale is administered.
Statistical analysisDescriptive parameters were calculated for all the variables: mean and standard deviation (SD) in the quantitative variables that adjusted to a normal distribution (Shapiro–Wilk test); and mean and inter-quartile range in variables that did not adjust to it. Qualitative variables were expressed by relative frequency percentages. The comparison between 2 groups was performed by using the Chi-square test (χ2) or Fisher's exact test for categorical variables, and Student's t-test or Mann–Whitney U test for quantitative variables. The main variable was calculated in a 95% confidence interval. Tests were considered significant if P<.05. We used the programme SPSS® v.17 for the statistical analysis.
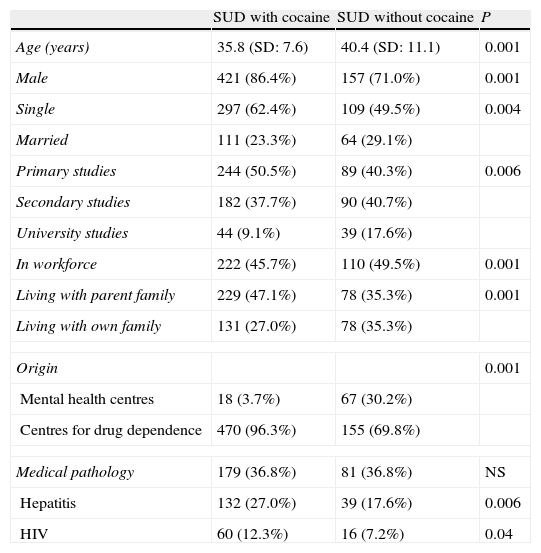
ResultsThe study included 837 patients: 208 (24.9%) from MHC and 629 (75.1%) from CAID and CAD. Of these 837 patients assessed, 710 had a lifetime diagnosis of SUD (including alcohol and excluding tobacco). There were 127 subjects (26.5%) without SUD. As for the disorder for cocaine use, 488 patients had a lifetime diagnosis (abuse or dependence); of these, 365 presented current abuse of or dependence on cocaine. There were 25 subjects with a lifetime diagnosis of cocaine abuse or dependence without other SUD associated. Table 1 presents the sociodemographic characteristics of the patients with lifetime cocaine use disorder.
Characteristics of the patients with lifetime cocaine use disorder (n=488) compared with addicts without cocaine abuse or dependence (n=222).
| SUD with cocaine | SUD without cocaine | P | |
| Age (years) | 35.8 (SD: 7.6) | 40.4 (SD: 11.1) | 0.001 |
| Male | 421 (86.4%) | 157 (71.0%) | 0.001 |
| Single | 297 (62.4%) | 109 (49.5%) | 0.004 |
| Married | 111 (23.3%) | 64 (29.1%) | |
| Primary studies | 244 (50.5%) | 89 (40.3%) | 0.006 |
| Secondary studies | 182 (37.7%) | 90 (40.7%) | |
| University studies | 44 (9.1%) | 39 (17.6%) | |
| In workforce | 222 (45.7%) | 110 (49.5%) | 0.001 |
| Living with parent family | 229 (47.1%) | 78 (35.3%) | 0.001 |
| Living with own family | 131 (27.0%) | 78 (35.3%) | |
| Origin | 0.001 | ||
| Mental health centres | 18 (3.7%) | 67 (30.2%) | |
| Centres for drug dependence | 470 (96.3%) | 155 (69.8%) | |
| Medical pathology | 179 (36.8%) | 81 (36.8%) | NS |
| Hepatitis | 132 (27.0%) | 39 (17.6%) | 0.006 |
| HIV | 60 (12.3%) | 16 (7.2%) | 0.04 |
HIV: human immunodeficiency virus; NS: not significant; SD: standard deviation; SUD: substance use disorder.
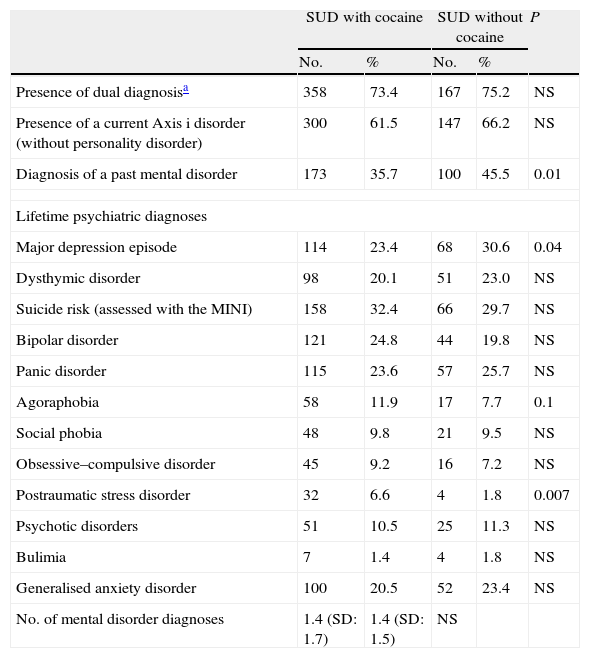
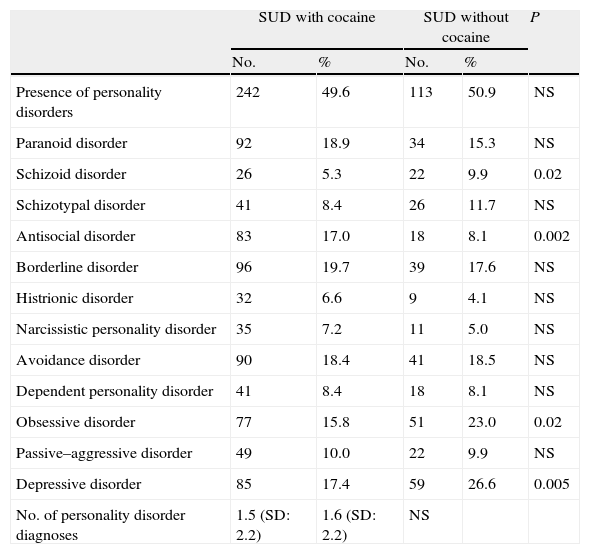
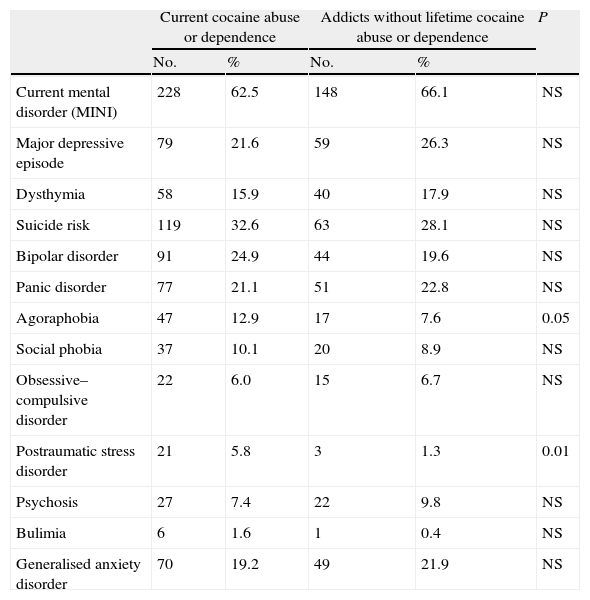
Table 2 shows the distribution of lifetime co-occurring mental disorders. Dual diagnosis was considered to exist if there was the presence of a diagnosis of a current mental disorder established by the MINI or a diagnosis of personality disorder by using the PDQ questionnaire. A total of 73.4% of the addicts (criteria of abuse or dependence) had a dual diagnosis. Table 3 indicates the distribution of the personality disorders in the patients with lifetime abuse of or dependence on cocaine. Table 4 presents the current diagnoses of Axis i disorders by means of the MINI interview in the subjects with current cocaine abuse or dependence.
Lifetime mental disorders (Axis i) in subjects with lifetime cocaine use disorder (n=488) compared with addicts lacking cocaine abuse or dependence (n=222).
| SUD with cocaine | SUD without cocaine | P | |||
| No. | % | No. | % | ||
| Presence of dual diagnosisa | 358 | 73.4 | 167 | 75.2 | NS |
| Presence of a current Axis i disorder (without personality disorder) | 300 | 61.5 | 147 | 66.2 | NS |
| Diagnosis of a past mental disorder | 173 | 35.7 | 100 | 45.5 | 0.01 |
| Lifetime psychiatric diagnoses | |||||
| Major depression episode | 114 | 23.4 | 68 | 30.6 | 0.04 |
| Dysthymic disorder | 98 | 20.1 | 51 | 23.0 | NS |
| Suicide risk (assessed with the MINI) | 158 | 32.4 | 66 | 29.7 | NS |
| Bipolar disorder | 121 | 24.8 | 44 | 19.8 | NS |
| Panic disorder | 115 | 23.6 | 57 | 25.7 | NS |
| Agoraphobia | 58 | 11.9 | 17 | 7.7 | 0.1 |
| Social phobia | 48 | 9.8 | 21 | 9.5 | NS |
| Obsessive–compulsive disorder | 45 | 9.2 | 16 | 7.2 | NS |
| Postraumatic stress disorder | 32 | 6.6 | 4 | 1.8 | 0.007 |
| Psychotic disorders | 51 | 10.5 | 25 | 11.3 | NS |
| Bulimia | 7 | 1.4 | 4 | 1.8 | NS |
| Generalised anxiety disorder | 100 | 20.5 | 52 | 23.4 | NS |
| No. of mental disorder diagnoses | 1.4 (SD: 1.7) | 1.4 (SD: 1.5) | NS | ||
MINI: Mini International Neuropsychiatric Interview; NS: not significant; PDQ: Personality Disorder Questionnaire; SD: standard deviation; SUD: substance use disorder.
Personality disorders in patients with lifetime cocaine use disorder (n=488) compared with addicts lacking cocaine abuse or dependence (n=222).
| SUD with cocaine | SUD without cocaine | P | |||
| No. | % | No. | % | ||
| Presence of personality disorders | 242 | 49.6 | 113 | 50.9 | NS |
| Paranoid disorder | 92 | 18.9 | 34 | 15.3 | NS |
| Schizoid disorder | 26 | 5.3 | 22 | 9.9 | 0.02 |
| Schizotypal disorder | 41 | 8.4 | 26 | 11.7 | NS |
| Antisocial disorder | 83 | 17.0 | 18 | 8.1 | 0.002 |
| Borderline disorder | 96 | 19.7 | 39 | 17.6 | NS |
| Histrionic disorder | 32 | 6.6 | 9 | 4.1 | NS |
| Narcissistic personality disorder | 35 | 7.2 | 11 | 5.0 | NS |
| Avoidance disorder | 90 | 18.4 | 41 | 18.5 | NS |
| Dependent personality disorder | 41 | 8.4 | 18 | 8.1 | NS |
| Obsessive disorder | 77 | 15.8 | 51 | 23.0 | 0.02 |
| Passive–aggressive disorder | 49 | 10.0 | 22 | 9.9 | NS |
| Depressive disorder | 85 | 17.4 | 59 | 26.6 | 0.005 |
| No. of personality disorder diagnoses | 1.5 (SD: 2.2) | 1.6 (SD: 2.2) | NS | ||
NS: not significant; SD: standard deviation; SUD: substance use disorder.
Current Axis i mental disorders in subjects with cocaine abuse or dependence (n=365) compared with addicts without history of cocaine abuse or dependence (n=224).
| Current cocaine abuse or dependence | Addicts without lifetime cocaine abuse or dependence | P | |||
| No. | % | No. | % | ||
| Current mental disorder (MINI) | 228 | 62.5 | 148 | 66.1 | NS |
| Major depressive episode | 79 | 21.6 | 59 | 26.3 | NS |
| Dysthymia | 58 | 15.9 | 40 | 17.9 | NS |
| Suicide risk | 119 | 32.6 | 63 | 28.1 | NS |
| Bipolar disorder | 91 | 24.9 | 44 | 19.6 | NS |
| Panic disorder | 77 | 21.1 | 51 | 22.8 | NS |
| Agoraphobia | 47 | 12.9 | 17 | 7.6 | 0.05 |
| Social phobia | 37 | 10.1 | 20 | 8.9 | NS |
| Obsessive–compulsive disorder | 22 | 6.0 | 15 | 6.7 | NS |
| Postraumatic stress disorder | 21 | 5.8 | 3 | 1.3 | 0.01 |
| Psychosis | 27 | 7.4 | 22 | 9.8 | NS |
| Bulimia | 6 | 1.6 | 1 | 0.4 | NS |
| Generalised anxiety disorder | 70 | 19.2 | 49 | 21.9 | NS |
MINI: Mini International Neuropsychiatric Interview; NS: not significant.
We compared the subgroup of subjects addicted to cocaine (n=488; 68.7%) with the rest of addicts lacking abuse of or dependence on cocaine (n=222; 31.3%). Of the 488 addicted to cocaine, the majority (463; 94.9%) had other co-occurring SUD, while 25 (5.1%) had only the diagnosis of cocaine use disorder. Among the SUD associated with cocaine, the most prevalent were: alcohol, 366 (75.0%); cannabis, 276 (56.6%) and opiates, 175 (35.9%). The mean age for initiating cocaine use was 21.0 years (SD=6.5). There were differences in the age of initiation in the other uses between the cocaine subgroup and the rest of the addicts. Subjects addicted to cocaine had begun earlier use of alcohol (15.5 years; SD=4.1 vs 18.1 years; SD=8.2; P<.001) and of cannabis (15.8 years; SD=3.9 vs 17.6 years, SD=5.5; P=.006).
With respect to the sociodemographic characteristics, cocaine addicts were younger, with a predominance of males, lower level of studies and worse work situation, and greater presence of serology positive for hepatitis and human immunodeficiency virus (HIV) (Table 1).
The subgroup of patients addicted to cocaine had the same frequency of dual diagnoses as the rest of the addicts. With respect to Axis i diagnosis, the main differences were found in the relationship between cocaine and post-traumatic stress disorder (PTSD), and a tendency not statistically significant towards agoraphobia (Table 2).
The main differences were revealed in the diagnoses of personality disorders (Table 3). Antisocial disorder was more prevalent in those addicted to cocaine, while the schizoid and obssesive personality disorders were more prevalent in the rest of the addicts.
Comparison between the subjects with only cocaine use disorder and cocaine addicts to cocaine with other co-occurring diagnoses for substance useThe main differences between patients addicted exclusively to cocaine (n=25) and patients with poly-addiction that included cocaine use disorder (n=463) were produced in the sociodemographic characteristics. In the poly-addiction subgroup there was a predominance of single individuals, living with their parent families, and fewer that were active in the workforce. In addition, there was a tendency that was not statistically significant towards earlier initiation to cocaine use.
There were no differences with respect to the prevalence of dual diagnosis in the 2 subgroups. Diagnoses of antisocial personality disorder and agoraphobia were significantly more prevalent in the subgroup of patients with poly-addiction.
Comparison between the subjects with cocaine use disorder exclusively and dual diagnosis cocaine addicts (with comorbid psychiatric diagnoses)As we have indicated earlier, there were 358 cocaine addicts with a dual diagnosis, while the 130 patients addicted to only cocaine did not have any co-occurring psychiatric diagnoses. The dual addicts had a lower predominance of males (93.8 vs 83.8%; P=.004) and were active in the workforce at a lower percentage (51.5 vs 43.5%; P=.03). The dual subgroup had a greater number of comorbid SUDs (2.9; SD=1.2 vs 3.2; SD=1.2; Mann–Whitney U test P=.02) and a non-significant tendency to a younger age for initiation to cocaine use (21.9 years, SD=6.4 vs 20.6 years; SD=6.5; P=.07).
Comparison of comorbid mental disorders between the subjects with current cocaine use disorder and the addicts that were not using cocaineWe compared the diagnoses of Axis i mental disorders between the patients with diagnosis of current abuse of or dependence on cocaine (n=365) with the addicts who had never been addicted to cocaine (n=224). The main differences were likewise found in prevalence of agoraphobia and PTSD (Table 4).
DiscussionThe data of this study offered us information on psychiatric comorbidity in one of the largest samples of cocaine addicts in treatment in our country. These data present the usual limitation of these clinical sample studies, in that the presence of poly-users is what is standard. The presence of multiple diagnoses of SUD are normally presented among addicts that seek treatment.16,21
Prevalence of dual diagnosis in cocaine addicts under treatmentApproximately 3 out of 4 cocaine addicts in this sample had a current mental disorder, including personality disorders. In our pilot study,18 based on the information obtained from the case histories, it was observed that almost half of the patients addicted to cocaine had a dual diagnosis. When the methodology was improved by using a structured interview, we saw that the majority of cocaine addicts in treatment some Axis i diagnosis using the MINI and/or a personality disorder diagnosis. The high rate of comorbidity that we found for cocaine addicts in treatment coincides with other studies.3,8,9,13,14,17
The most prevalent disorders were the various mood and anxiety disorders, which coincides with results from other studies.9,11,13,16,17 Likewise, MINI-assessed suicide risk was present in one-third of the addicts. Half of the patients had some personality disorder diagnosis, a figure equivalent to that provided by other studies,3,4 with the most prevalent being the paranoid, antisocial, borderline, depressive and avoidance disorders. The self-report questionnaire can overdiagnose these disorders; however, the clinical significance scale, which can correct such an overdiagnosis, provided a posterior check. In the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), the SUDs were basically associated with mood, anxiety and personality disorders.6,7,22,23 Likewise, the Epidemiologic Catchment Area (ECA) study also observed this association with dependence on cocaine.3 This comorbidity has been equally emphasised in other studies.8,17 In non-clinical samples, the prevalence of dual diagnosis might be less, although equally elevated; in out environment, by using a structured interview, 42.5% of dual diagnoses were indicated among cocaine addicts, with emphasis on mood disorders (26.6%) and anxiety disorders (13%) in the sample.11
Comparison between the addicts with cocaine use disorders and addicts that did not use cocaineAmong the subjects addicted to cocaine, most had other associated SUD, so these data are not extrapolatory to patients addicted exclusively to cocaine. Among addicts in treatment, this concomitance of use is what is normal and favours seeking treatment.16,24 To study possible differences as to psychopathology attributable to cocaine, we compared the cocaine-using addicts with the rest of addicts.
In the subgroup of cocaine addicts there were notable sociodemographic differences from the rest of addicts. They were younger, predominantly single, had a lower education level and worse work situation. In addition, they presented greater prevalence of serology positive for hepatitis and for HIV. This indicates a subgroup of addicts having worse medical and social consequences.
Furthermore, this subgroup initiated use of other drugs such as alcohol and cannabis earlier than the rest of the addicts. Likewise, this indicates a subgroup of more severe addiction.
However, in spite of the elevated prevalence of dual diagnosis in the cocaine addicts, it was not higher than in the rest of the addicts. In the ECA study, cocaine dependence was seen to be the one most associated with the presence of mental disorders.3 However, later studies observed that other dependencies such as that of alcohol and cannabis can be more intensely associated with the presence of dual diagnosis4,8,9 (and habitually in the case of poly-use patterns, as we have pointed out) and that the presence of various SUD diagnoses is more associated with dual diagnosis than the consumption of a single drug,16,25 especially the combination of alcohol with an illegal drug.15 Likewise, it has been indicated that the risk of suicide is greater in subjects dependent on alcohol than in those dependent on cocaine.26
All the mood and anxiety disorders were very prevalent, with figures that coincide with those of other studies on cocaine addicts.3,13,16,17 However, the diagnoses most specifically associated with cocaine were PTSD and agoraphobia. In the NESARC study, agoraphobia was the anxiety disorder most associated with the SUDs7 and PTSD was a diagnosis also intimately associated with subjects con SUD in treatment, constituting a more severe subgroup.9,13,27–29 In contrast, the diagnosis of major depressive disorder has been associated more with the presence of various SUD diagnoses and alcohol dependence than with dependence on illegal drugs.8 An association between depression and alcohol consumption in cocaine addicts has been reported.30 Likewise, the previously indicated authors observed that phobias were associated with the presence of various diagnoses for SUD.8 The mechanisms that justify these Axis i diagnostic differences between different substances have not been established and, as we have indicated, the presence of several concomitant SUD diagnoses makes interpreting these relationships more difficult. Studying these relationships in depth can help to clarify the etiopathogenic mechanisms underlying the frequent comorbidity between SUDs and mental disorders.
With respect to personality disorders, the one most associated with the subgroup of cocaine addicts was antisocial disorder. This disorder may be associated with a pattern of multiple dependencies on illegal drugs,6 so we did not observe this diagnosis in the small subgroup of addiction to cocaine exclusively. This personality disorder is usually among the most prevalent in the addicts to illegal drugs and the one most associated with the presence of a SUD,3,6,9,17,31–33 especially with various diagnoses of concomitant SUD.8,24 However, there were no differences between the 2 subgroups in prevalence of personality disorders. Other authors have even reported higher prevalence of personality disorders in assistance services for alcohol addicts than in assistance centres for other drugs.34
In our pilot study,18 we also saw that the presence of mood disorders were more associated with alcohol dependence, and this association was likewise reported this way in other studies such as the National Comorbidity Survey (NCS).35 In contrast, cocaine dependence was more associated with the diagnosis of personality disorders in that survey. In the ECA study, cocaine dependence was the one that presented the greatest association with antisocial personality disorder3 and, in the NESARC study, personality disorders likewise presented a close association with SUDs in general.6
Comparison between the subjects with exclusively disorder for cocaine use and dual cocaine addicts (with comorbid psychiatric diagnoses)When we compared the subgroup of cocaine addicts without dual diagnoses with the dual addicts, we found that non-dual subjects had a greater predominance of males and better work situations. The dual addicts tended to present an earlier initiation to cocaine use and had a greater number of concomitant SUD diagnoses. As we have indicated previously, other authors have indicated that the greater the number of SUDs, the more the psychiatric symptoms25 and the greater the risk of comorbid mental disorders.8,24 This indicates that dual patients constitute a more severe subgroup.
Study limitationsIn our study, SUD was diagnosed by using a clinical interview, not included in the toxicological analysis protocol or using other sources of information. However, the majority of the patients were known in the centres for drug dependency assistance, where urine analyses are routinely performed and the staff know their use patterns well. It is possible that the involvement of more motivated researchers in the dual diagnosis study might have led to an overdiagnosis of the problem; however, standardised instruments were used, prior training was given and a large number of researchers participated.
We consider that the high number of researchers and centres participating constitutes strength of the study, given that the data can be extrapolated to the subjects in treatment in the salud mental and drug network of the Community of Madrid. The use of a structured interview and the sample size obtained are other strengths of this study.
Ethical disclosuresProtection of human and animal subjectsThe authors state that the procedures followed were adapted to the ethical regulations of the human research committee in charge and in agreement with the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors state that they followed the protocols of their work centres on publishing patient data and that all the patients included in the study received sufficient information and gave their informed consent in writing for participating in this study.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects mentioned in this article. This document is in the power of the corresponding author.
FundingThis study was funded by the Obra Social Caja Madrid, the Institute of Addictions of the Madrid City Council, the Antidrug Agency of the Community of Madrid and the Regional Office of Mental Health in the Community of Madrid. The project was promoted by the SEPD.
Conflict of interestsThe authors have no conflict of interest to declare.
We wish to express our gratitude to all the researchers at the CAD, CAID and mental health centres.
Please cite this article as: Arias F, et al. Abuso o dependencia a la cocaína y otros trastornos psiquiátricos. Estudio Madrid sobre la prevalencia de la patología dual. Rev Psiquiatr Salud Ment (Barc.). 2013;6:121–8.