The enormous potential effects of health behavior change on mortality, morbidity, and health care costs provide ample motivation for the concept of lifestyle medicine. Lifestyle medicine involves the therapeutic use of lifestyle interventions on health and quality of life, and considers not only risk factors and markers, but also a range of antecedent factors from all levels of causality. Treatment would ultimately employ a combination of clinical (patient-centered) and public-health interventions. Examples of target patient behaviors include, but are not limited to, eliminating tobacco use, moderating alcohol consumption, increasing physical activity, improving diet, sleep, and emotional and mental well-being. The effective implementation of lifestyle medicine should be a priority within the necessary changes in current healthcare systems and public health policies.
Los enormes efectos potenciales de determinadas intervenciones en el estilo de vida sobre la mortalidad, morbilidad y costes sanitarios son motivación más que suficiente para el interés actual en la medicina del estilo de vida. La medicina del estilo de vida se ocupa de las intervenciones sobre el estilo de vida que afectan a la salud y a la calidad de vida, y tiene en cuenta todas las causas anteriores a la enfermedad y al riesgo de enfermar, desde todos los niveles de causalidad. En consecuencia, en su manejo terapéutico se incluye una combinación de intervenciones preventivas de salud con actuaciones clínicas personalizadas para cada paciente. Ejemplos de dichas intervenciones incluyen, sin limitarse a, el abandono tabáquico; una dieta equilibrada; el control de peso corporal; el aumento de la actividad física; el consumo moderado de alcohol; el sueño y descanso adecuados; y el incremento del bienestar emocional y mental, entre otros. La aplicación efectiva de la medicina del estilo de vida debería considerarse prioritaria dentro de los cambios necesarios en los actuales sistemas sanitarios y en las políticas públicas de salud.
In the developed world, lifestyle is one of the major determining factors concerning the health condition of a population. A high percentage of medical consultations in primary and specialist healthcare are due to lifestyle-related illnesses (which are, therefore, preventable). Likewise, the great majority of practice guidelines recommend lifestyle changes as the first line of treatment. Consequently, lifestyle is not only a public health issue, but also very clinically relevant in current therapeutic management of illnesses especially chronic pathologies. The advent of “lifestyle medicine” seeks to resolve the current shortcomings and provide continuity between preventative medicine and current patient-centred clinical practice.1
The burden of chronic disease: mental healthCoronary disease, stroke, hypertension, high cholesterol, obesity, diabetes, chronic obstructive pulmonary disease (COPD), many types of neoplasms, osteoporosis, back and muscle pain, migraines, constipation, allergic pathologies, sexually transmitted diseases (STD), infertility, erectile dysfunction and many mental disorders, among other diseases, are health conditions directly related to lifestyle. Out of these, mental illnesses enormously contribute to the total disease burden, due to the combination of high prevalence, early onset, persistence and dysfunction. The World Health Organization (WHO) attributes 31% of collective years lived with a disability and 1.4% of collective years lost2 to neuropsychiatric disorders. However, the latter figure is most likely underestimated, as it does not include suicides. Schizophrenia and related psychoses, bipolar affective disorder, major depression and panic disorder are those that contribute most to the global disease burden. By the year 2030, it unipolar depression is predicted to be the primary cause of the total disease burden.3
What is a lifestyle?The author and futurist Alvin Toffler4 used the concept “lifestyle” for the first time in 1979 when he predicted the explosion of different lifestyles in a post-industrial society. The way we eat, exercise, rest, play, behave with others, think, plan, drive a vehicle, sleep, work, do other things–in general, the way we live–are all included under the term “lifestyle.” It includes patterns for social relations, leisure and clothing and it also reflects the typical individual's attitude, values or self-image. A specific lifestyle indicates the conscious or unconscious choice between one type of behaviour or another and can affect the basic biological mechanisms that lead to disease: changes in genetic expression, inflammation, oxidative stress and metabolic dysfunction.
What is lifestyle medicine?Lifestyle medicine is a clinical discipline based on facts (“evidence”) that deals with lifestyle interventions that affect health and quality of life. It could also be defined as the “application of medical, environmental, motivational and behavioural principles to clinical and therapeutic management of health problems related to lifestyle”.5 In addition to prevention of illness (risk reduction), lifestyle medicine also focuses on its therapeutic management (if such a condition is already present), often in a more cost-effective way6 than conventional treatments based on drugs and surgery. The enormous potential effects of such lifestyle interventions on mortality, morbidity and healthcare costs are more than sufficient incentives for interest in lifestyle medicine.7 Examples of such interventions include, but are not limited to, all of the following: cessation of tobacco use, balanced diet, weight control, increased physical activity, moderate alcohol consumption; adequate sleep and rest, and increased mental and emotional well-being.
Lifestyle medicine was originally developed in the United States.8 There, as well as in Spain,9 various medical associations and ongoing projects exist related to lifestyle medicine. Furthermore, the American Journal of Lifestyle Medicine (http://ajl.sagepub.com/), the first publication specialising in this issue, has been available since January 2007. While it is a new discipline, lifestyle medicine does not purport to be an alternative to conventional medicine, but rather a complementary strategy to deal with the clinical challenges that modern lifestyle changes represent. Nonetheless, lifestyle medicine is not lucrative and is not typically funded by public health systems or private insurers. For that reason, its use in current clinical practice is very limited and is not usually part of medical training programs.
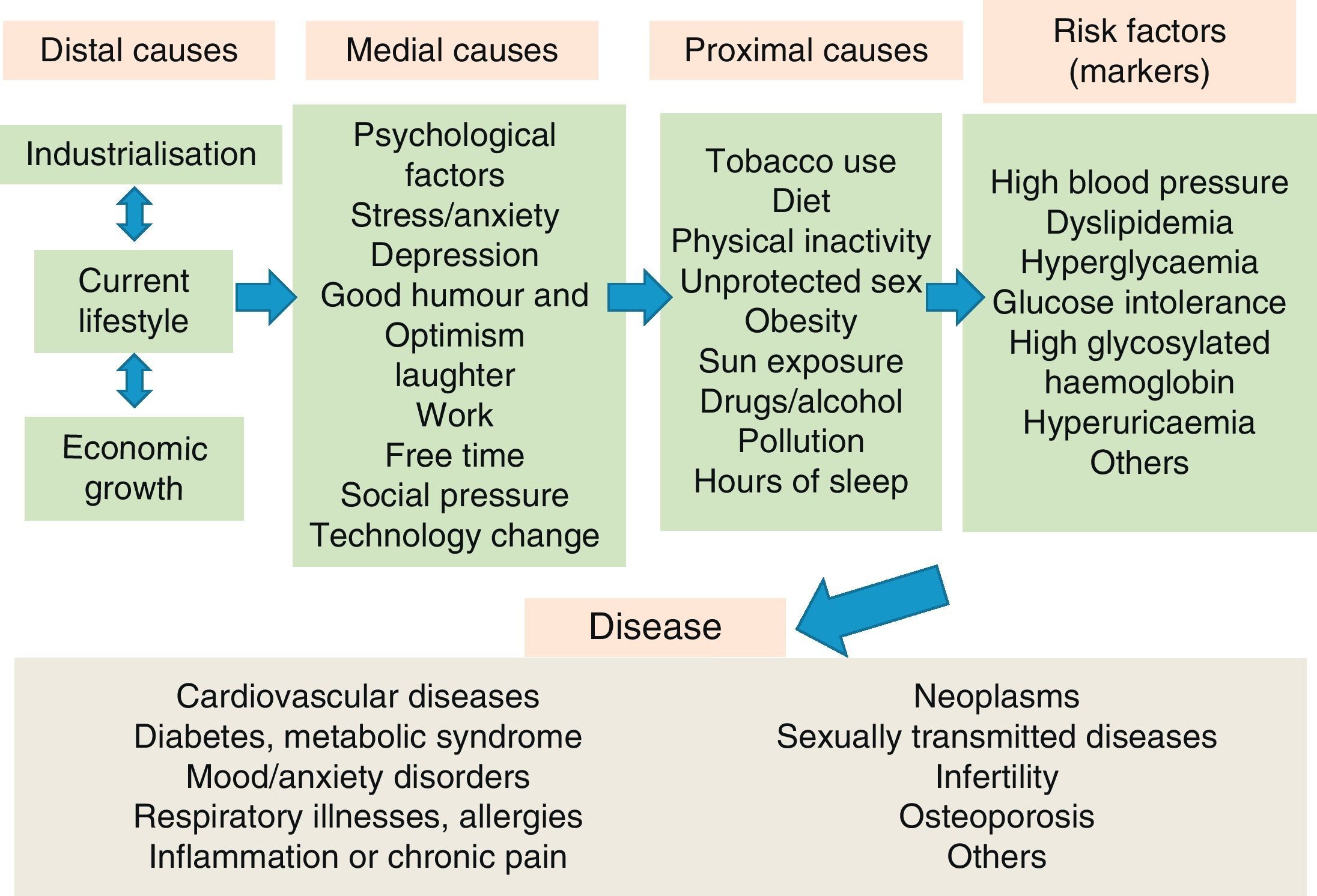
The causes of illnessIn the present day, the therapeutic approach to disease, and particularly to chronic pathologies, usually focuses on risk factors and biological markers. However, these factors and markers have numerous “causes” that precede the disease (Fig. 1). In lifestyle medicine, all preceding risks and causes of disease are considered, on all levels of causality. Consequently, its therapeutic management includes a combination of preventative health interventions (public and individual) and clinical activities personalised for each patient. For example, the prevalence of high blood pressure in the population could be reduced with not only individualised treatment at the clinical practice level, but also with community activities to raise awareness of the environmental effects of using fossil fuels instead of human powered transport (like riding a bicycle or walking). This intervention would also result in an increase in physical activity and a decrease in obesity10 or depressive and anxiety symptoms, among other risk factors for cardiovascular and mental disease. Thus, the final impact might be superior to the present approach to high blood pressure in conventional medicine.
Hierarchy of causality of chronic diseases.
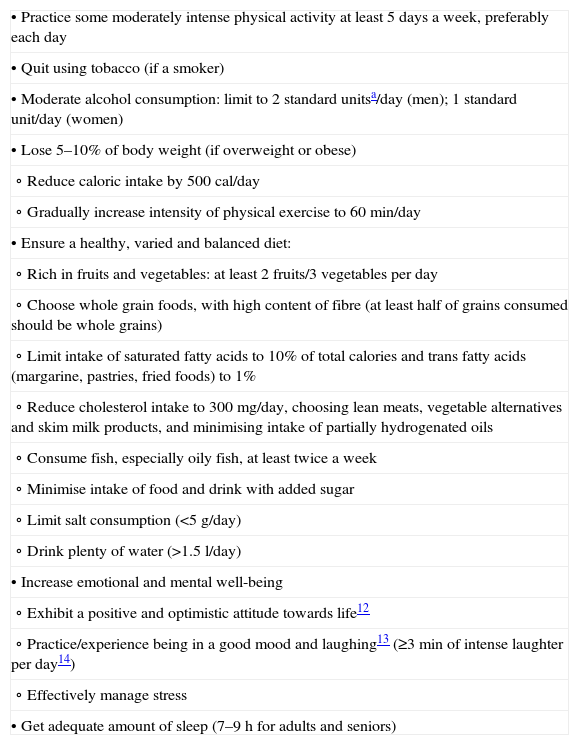
Many studies (“evidence”) guarantee the effectiveness of lifestyle interventions in reducing the risk of developing a chronic disease, as well as aiding in the therapeutic management of an existing health condition.11 Based on available data, national and international guides emphasise the relevance of lifestyle interventions to general good health, as well as to the majority of conditions and diseases. The general consensus of these recommendations include, but are not limited to, various changes in diet, toxic habits, physical exercise, weight control and emotional and mental well-being, among others (Table 1).12–15 For specific medical conditions, there are other recommendations (occasionally, there are variations of the general ones), yet they always stress the following 2 key points: they specify healthy behaviour and they highlight that even small lifestyle improvements, if maintained over time, can also help reduce risk of disease or slow the progression of a disease.
Lifestyle medicine: general health recommendations.
| • Practice some moderately intense physical activity at least 5 days a week, preferably each day |
| • Quit using tobacco (if a smoker) |
| • Moderate alcohol consumption: limit to 2 standard unitsa/day (men); 1 standard unit/day (women) |
| • Lose 5–10% of body weight (if overweight or obese) |
| ∘ Reduce caloric intake by 500 cal/day |
| ∘ Gradually increase intensity of physical exercise to 60min/day |
| • Ensure a healthy, varied and balanced diet: |
| ∘ Rich in fruits and vegetables: at least 2 fruits/3 vegetables per day |
| ∘ Choose whole grain foods, with high content of fibre (at least half of grains consumed should be whole grains) |
| ∘ Limit intake of saturated fatty acids to 10% of total calories and trans fatty acids (margarine, pastries, fried foods) to 1% |
| ∘ Reduce cholesterol intake to 300mg/day, choosing lean meats, vegetable alternatives and skim milk products, and minimising intake of partially hydrogenated oils |
| ∘ Consume fish, especially oily fish, at least twice a week |
| ∘ Minimise intake of food and drink with added sugar |
| ∘ Limit salt consumption (<5g/day) |
| ∘ Drink plenty of water (>1.5l/day) |
| • Increase emotional and mental well-being |
| ∘ Exhibit a positive and optimistic attitude towards life12 |
| ∘ Practice/experience being in a good mood and laughing13 (≥3min of intense laughter per day14) |
| ∘ Effectively manage stress |
| • Get adequate amount of sleep (7–9h for adults and seniors) |
Patients with a mental illness usually have worse physical health than the general population, with higher morbidity and mortality rates.16 Comorbidity with other disorders is frequent and can occur at 4 levels: with other mental illnesses, with substance abuse and dependence, with other chronic diseases, or with accidental or intentional injuries; comorbidity can also be attributed to social factors and lifestyle.17,18 In particular, a greater percentage of patients suffer from inadequate diets, physical inactivity, tobacco abuse, diabetes, obesity or hyperlipidaemia, among other health conditions.19,20 Furthermore, secondary effects from the mental illness drugs themselves can aggravate or add additional risks, such as obesity, diabetes, cardiovascular disease or metabolic syndrome.21 Consequently, promoting and maintaining a healthy lifestyle become very important for these patients. Lifestyle changes can be effective in decreasing morbidity and mortality and increasing quality of life,22,23 as well as in optimising clinical performance of treatments used, increasing their observance or improving the doctor–patient relationship.24–28 Therefore, the most cost-effective therapeutic strategies would include a combination of pharmacological therapies with different preventative and psychosocial lifestyle interventions, which would be facilitated at a community or primary healthcare level.29,30 The major barriers for the implementation of lifestyle medicine are factors derived from the disease itself and from its treatment, such as lack of motivation, low self-esteem and confidence; or side effects such as sedation or weight increase associated with pharmacological treatment.19 This suggests that it is necessary to ensure that health professionals, in addition to setting an example, have certain abilities and have a positive and encouraging attitude towards lifestyle intervention, which is preferentially applied in groups (although this is not always recommended).
Competency to prescribe lifestyle medicineMotivating someone effectively to change their lifestyle can be highly frustrating and a great challenge, for all types of patients. In addition to establishing a plan of action in collaboration with the patient and to arranging a follow-up, motivational interviewing31 has been shown to be a useful technique in clinical practice for improving the results o desired from these prescribed changes. Behavioural techniques, the most recommended method to influence change in risk factors, include all of the following11: evaluating the patient, establishing goals, increasing awareness, overcoming barriers, managing stress effectively, cognitive restructuring, preventing relapse and providing adequate support and treatment. Nevertheless, health professionals express a lack of knowledge and ability needed to motivate and to advise their patients to undergo lifestyle interventions.32 Among the competencies proposed for being able to prescribe lifestyle medicine, all the following are included33: (a) leadership to practice and promote healthy lifestyles; (b) knowing how to identify markers of a patient's health condition related to lifestyle and to demonstrate knowledge of specific and precise changes; (c) evaluating how motivated and willing the patients and their families are to perform such changes and establishing joint plans of action; (d) using clinical practice guides in order to help patients manage their own health behaviour and lifestyle; and (e) working with a multidisciplinary team in order to treat the patient from all aspects necessary.
ConclusionsLifestyle medicine has shown to be a more cost-effective strategy than the approaches currently used in disease prevention and treatment, particularly chronic pathologies. Nevertheless, health professionals currently lack the training and resources to manage lifestyle interventions for their patients. Among other limiting factors, there are not sufficient incentives and support programs to encourage professionals to treat the true causes of disease with lifestyle interventions, rather than intervening at the level of risk factors or markers. Effective application of lifestyle medicine should be considered a priority within the changes needed in current health systems and in public health policies. In this day and age, health spending is rationalised and available resources are put to optimal use. Lifestyle medicine, as well as reducing total costs, has the potential to notably increase the indicators of physical and mental health and the population's quality of life.
Conflicts of interestThe author has no conflict of interest to declare.
Please cite this article as: Mora Ripoll R. Medicina del estilo de vida: la importancia de considerar todas las causas de la enfermedad. Rev Psiquiatr Salud Ment (Barc.). 2012;5(1):48–52.