Lack of insight is a common clinical problem in psychiatric patients, but few times has been properly studied until recently. Patients with good insight tend to show a better treatment adherence with a better prognosis and show less hostility. This study aims to investigate whether there is a relationship between the hostility degree and insight or not and to analyse if there are insight quantitative differences between the patients regarding their diagnoses.
MethodOne hundred and sixty-eight psychotic patients were studied (including 86 patients with schizophrenia and 43 with bipolar disorder). PANNS P7 (hostility) item and G14 (poor impulse control) were analysed in order to assess patients’ violence and G12 in order to assess insight. All these data were correlated. It was also analysed the PANSS results of schizophrenic vs bipolar patients regarding insight and hostility separately looking for a more homogenic pull of patients.
ResultsPatients with greater hostility showed a worse impulse control and poorer insight than the rest. Schizophrenic patients showed a greater hostility and lower insight than bipolar patients.
DiscussionLack of insight may lead to a greater hostility and worse impulse control. Therapeutic interventions addressed to improve insight could indirectly lower hostility and gain a better impulse control for psychotic patients.
En pacientes con trastornos psiquiátricos el déficit en la capacidad de introspección o insight es frecuentemente un problema clínico importante, pero ha sido pocas veces objeto de estudio formal. Los pacientes psicóticos con buen insight suelen cumplir mejor las pautas de medicación siendo un factor de buen pronóstico y muestran menor hostilidad. Con este estudio se pretende valorar si existe una relación entre el grado de hostilidad del paciente y la conciencia de enfermedad además de analizar si el grado de conciencia de enfermedad varía según el diagnóstico del paciente (esquizofrenia vs. trastorno bipolar).
MetodologíaSe estudiaron en 168 pacientes psicóticos (entre ellos 86 con esquizofrenia y 43 con trastorno bipolar) los ítems de la PANSS P7 (hostilidad) y G14 (control deficiente de impulsos) para valorar el grado de violencia y el ítem G12 (ausencia de juicio e introspección) correlacionándolos entre ellos. Para observar si había diferencias en cuanto a insight y hostilidad según el diagnóstico, se estudiaron los datos utilizando una muestra más reducida y homogénea comparando los pacientes diagnosticados de esquizofrenia con los diagnosticados de trastorno bipolar.
ResultadosLos pacientes con mayor hostilidad presentaban un peor control de impulsos y una pobre conciencia de enfermedad. Los pacientes diagnosticados de esquizofrenia presentan una mayor hostilidad y un peor insight comparados con los diagnosticados de trastorno bipolar.
DiscusiónLa ausencia de introspección supondría un mayor nivel de hostilidad y mayor déficit de control de impulsos. Las estrategias terapéuticas encaminadas a aumentar el grado de insight del paciente podrían disminuir indirectamente el grado de hostilidad y proporcionar un mejor control de los impulsos.
In patients with psychiatric disorders, the deficit in the capacity for introspection, or insight, is frequently a significant clinical problem, but it has seldom been studied formally.1 Limited capacity for insight in psychosis has been described as a limited capacity to recognise the deficits, consequences and need for treatment linked to the disorder. Insight is made up of several phenomena, including the capacity for past and current introspection. Insight in relation to mental health makes reference to individuals’ perception of themselves compared to the one that their cultural and community surroundings have. At one end of the range of insight, it is understood as a psychological defence, while it is conceived as a neurocognitive deficit at the other end.2 Insight in psychosis is a clinical construct that researchers and clinicians find useful to make the patients’ difficulty in recognising their illness and its consequences understandable.3 Previous scientific publications suggest that a lack of insight can be related to worse disease evolution and worse therapy adherence. With respect to psychotic patients, a low capacity for insight has been related to high mood, lack of suicidal thoughts, apathy, mental disorganisation and emotional flattening. In contrast, good insight has been linked to better therapy adherence and less hostility.1,4–10
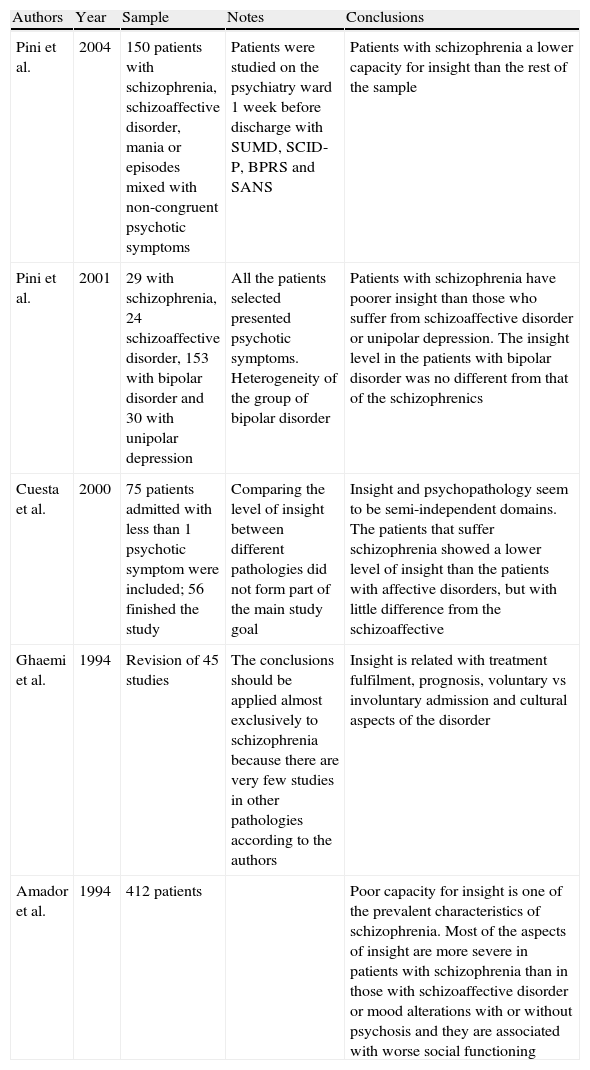
Table 1 presents a summary of the most relevant scientific articles on the differences in insight among various psychiatric pathologies. The results in a 2004 study indicated worse insight in patients with schizophrenia than in those with mania or mixed mood episodes.11 Another study was that of Pini et al.,12 in which no differences in insight were found between schizophrenia and bipolar disorder. There is also a review in this area by Ghaemi and Pope4 and a study by Amador et al.13 The Spanish team of Cuesta et al.14 published an article in which they investigated whether insight changed over time and how it was related to patient psychopathology, as well as examining the relationships between insight scale in patients with psychosis.
Previous articles on differences in insight among psychiatric pathologies.
| Authors | Year | Sample | Notes | Conclusions |
| Pini et al. | 2004 | 150 patients with schizophrenia, schizoaffective disorder, mania or episodes mixed with non-congruent psychotic symptoms | Patients were studied on the psychiatry ward 1 week before discharge with SUMD, SCID-P, BPRS and SANS | Patients with schizophrenia a lower capacity for insight than the rest of the sample |
| Pini et al. | 2001 | 29 with schizophrenia, 24 schizoaffective disorder, 153 with bipolar disorder and 30 with unipolar depression | All the patients selected presented psychotic symptoms. Heterogeneity of the group of bipolar disorder | Patients with schizophrenia have poorer insight than those who suffer from schizoaffective disorder or unipolar depression. The insight level in the patients with bipolar disorder was no different from that of the schizophrenics |
| Cuesta et al. | 2000 | 75 patients admitted with less than 1 psychotic symptom were included; 56 finished the study | Comparing the level of insight between different pathologies did not form part of the main study goal | Insight and psychopathology seem to be semi-independent domains. The patients that suffer schizophrenia showed a lower level of insight than the patients with affective disorders, but with little difference from the schizoaffective |
| Ghaemi et al. | 1994 | Revision of 45 studies | The conclusions should be applied almost exclusively to schizophrenia because there are very few studies in other pathologies according to the authors | Insight is related with treatment fulfilment, prognosis, voluntary vs involuntary admission and cultural aspects of the disorder |
| Amador et al. | 1994 | 412 patients | Poor capacity for insight is one of the prevalent characteristics of schizophrenia. Most of the aspects of insight are more severe in patients with schizophrenia than in those with schizoaffective disorder or mood alterations with or without psychosis and they are associated with worse social functioning |
Our study represents an attempt to assess whether there is a relationship between the degree of the patient's hostility and their awareness of illness. In addition, we analysed if the level of patient awareness of their mental disorder varied according to patient diagnosis (schizophrenia vs bipolar disorder).
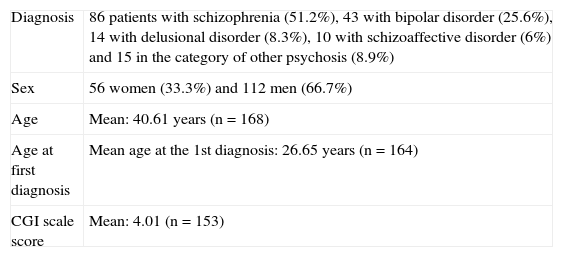
MethodologyA sample of 168 patients, with the characteristics detailed in Table 2, was used. The inclusion criteria were as follows: patients diagnosed with any psychotic disorder based on DSM-IV-TR criteria, age over 18 years old and informed consent form appropriately filled in by the patient. We included the diagnosis of bipolar disorder, given that previous studies have emphasised the high prevalence of psychotic symptoms in this type of patients.15
Descriptive sample data.
| Diagnosis | 86 patients with schizophrenia (51.2%), 43 with bipolar disorder (25.6%), 14 with delusional disorder (8.3%), 10 with schizoaffective disorder (6%) and 15 in the category of other psychosis (8.9%) |
| Sex | 56 women (33.3%) and 112 men (66.7%) |
| Age | Mean: 40.61 years (n=168) |
| Age at first diagnosis | Mean age at the 1st diagnosis: 26.65 years (n=164) |
| CGI scale score | Mean: 4.01 (n=153) |
The exclusion criteria were: mental retardation, clinically influential concomitant substance dependence, organic disease interfering with behaviour, alterations of consciousness or attention and any alteration preventing a proper capacity to respond to the study questions.We studied the Positive and Negative Symptom Scale (PANSS) items P7 (hostility) and G14 (poor impulse control) to assess the level of violence and item G12 (insight) for the patients, correlating them by the Spearman test. Item P7 refers to verbal and nonverbal expressions of anger and resentment, including sarcasm, passive–aggressive behaviour, insults and physical aggression. Item G14 measures disorders in regulation and control of impulses, which cause a sudden, unmodulated, arbitrary or poorly-directed discharge of the tension and emotions without any concern for the consequences. Item G12 refers to disorders in awareness or understanding by the patients of their own psychiatric disorder and life situation. This is manifested by difficulties in recognising past or present psychiatric disorder, refusal to undergo treatment or be hospitalised, decisions characterised by poor sense of anticipation and by unrealistic short- and long-term projects. The PANSS scale is one of the most used instruments in psychiatric clinical practice and research and is validated in Castilian Spanish.16–18
Although many multidimensional scales on insight have been created recently, one of the methods most often used to assess the capacity for introspection is still PANSS Item G12.2,16 In fact, some of the studies in this respect use only this item and even emphasise that multidimensional approximation is of little use in the complex relationship between insight and psychopathology.19 Insight is currently considered a complex multidimensional phenomenon. However, Startup et al. have indicated that, in spite of the fact that many researchers accept insight as multidimensional, the factorial scale analyses usually provide unique factorial results and the majority of the scales significantly correlate among themselves and with instruments using only 1 item for assessment.14,20,21
To see whether there were differences in insight and hostility based on diagnosis, we studied the data using a smaller, more homogenous sample, comparing patients diagnosed with schizophrenia (86 patients) with those diagnosed with bipolar disorder (43 patients). The statistical tests used to compare these two groups were non-parametric ones (Mann–Whitney U for two independent samples), given that the variables, disorder awareness and hostility, did not have a normal distribution (Kolmogorov–Smirnov test <0).
ResultsHostility (P7), poor impulse control (G14) and insight (G12) were correlated positively (P=.000 for P7 with G12 and G14, and P=.003 for G12 with G14). That is, the greater the hostility, the worse the impulse control and disorder awareness were in these patients.
In the subsample of schizophrenic and bipolar patients, these variables were also correlated in the same way. Comparing the mean scores of these variables in these two groups, we found significant differences in insight (P=.008) and in hostility (P=.05). Patients diagnosed with schizophrenia presented greater hostility (mean: 1.88) and worse insight (mean: 2.71) compared with those diagnosed with bipolar disorder (mean hostility: 1.49; mean lack of judgement and insight: 2.02).
ConclusionsIn the sample studied, the patients with the greatest hostility presented the least insight. These results agree with the data from the most important previous studies.6,9,22–24 Perhaps other future longitudinal studies can shed some light on the possible causal relationship between insight and hostility.
The PANSS item on poor impulse control (G14), which was highly linked to hostility, was also very significantly correlated with the item measuring the level of insight (G12). That is, the poorer a patient's impulse control, the lower the capacity for insight generally found was. The reverse was also true; if we dealt with a patient having a high level of insight, it was logical to suppose that it was highly probable that they would present with better impulse control.
In view of the results described, we can conclude that therapy strategies aimed at increasing the level of patient insight could help to decrease the degree of hostility indirectly and provide better impulse control.
Patients with bipolar disorder have, according to our results, greater capacity for insight than those diagnosed with schizophrenia. One possible explanation is that patients diagnosed with schizophrenia suffer from more psychopathological alterations. These results agree with the majority of the previous studies analysed in the references,13,14 but not with all of them.12 Cuesta et al.14 studied 75 patients diagnosed with schizophrenia, affective disorders with psychotic symptoms and patients with schizoaffective disorder consecutively admitted in a hospital, after the acute episode remitted and again 6 months later. Up to a certain point, illness awareness improved with time in patients with psychosis, regardless of the diagnosis. Few significant relationships between psychopathology and insight remain stable in follow-up. The higher the scores in the dimensions of disorganisation and negatives, the less the attitude towards therapy changed in the follow-ups. Patients who suffered from schizophrenia showed worse awareness of illness than those who had affective disorders, but there were few differences with schizoaffective disorders.14
Ethical responsibilitiesProtection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.Confidentiality of data. The authors declare that no patient data appears in this article.Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Lera Calatayud G, et al. Relación entre insight, violencia y diagnóstico en pacientes con psicosis. Rev Psiquiatr Salud Ment (Barc.). 2012;5:43–7.